Natalie Locci-Molina1, Annie Wang2 and George Kroumpouzos2*
1The Warren Alpert Medical School of Brown University, and 2Department of Dermatology, The Warren Alpert Medical School of Brown University, 593 Eddy Street, Providence, RI 02903, USA. *E-mail: gk@gkderm.com
Accepted Nov 12, 2014; Epub ahead of print Nov 14, 2014
Melasma is a common acquired hypermelanosis of the skin that has been associated with several etiologic factors including ultraviolet light exposure, pregnancy, and oral contraceptives (OCPs) (1). Forty-one percent of women surveyed in one study had onset of melasma after pregnancy, and 25% after starting an OCP (2). Women who develop melasma during pregnancy may be more susceptible to developing melasma while on OCPs (1). OCP use has been an aggravating factor for melasma in several clinico-epidemiologic studies (3), and melasma was noted as rampant with the use of the very first combined oral contraceptives (COCPs) (4, 5). Although the association between melasma with OCP use has been well established, melasma associated with a hormone-releasing intrauterine device (IUD) has not been reported in the medical databases. Herein, we report 4 patients whose melasma, which initially occurred while taking (COCPs, improved after switching to a levonorgestrel (LNG)-releasing IUD (LNG-IUD) (6).
CASE REPORTS
Four women were evaluated for melasma while on a COCP and subsequently on LNG-IUD. The summary of clinical data is shown in Table I. All patients noticed a spontaneous improvement of melasma upon switching from COCP to LNG-IUD (Fig. 1). Patients were not receiving any treatment for their melasma at the time of the switch, and had been practicing sun protection throughout the course of treatment with both OCP(s) and LNG-IUD.
Table I. Summary of clinical data
|
Patient |
Age, years/race |
Distribution of melasma |
Oral contraceptive(s) |
Progestin contenta |
Estrogen contenta |
Improvement duration while on LNG-IUDb |
|
1 |
37/Caucasian |
Centrofacial |
Ortho Tri-Cyclen® (norgestimate/ethinyl estradiol) |
0.18/0.215/0.25 mg norgestimate |
35 µg EE |
1.5 years |
|
2 |
43/Hispanic |
Extensive facial |
YAZ® (drospirenone/ethinyl estradiol) |
3 mg drospirenone |
20 µg EE |
2 years |
|
3 |
44/Caucasian |
Malar |
Microgestin® 1/20 (norethidrone/ethinyl estradiol) then GianviTM (drospirenone/ethinyl estradiol) |
1 mg norethindrone 3 mg drospirenone |
20 µg EE 20 µg EE |
7 months |
|
4 |
32/Caucasian |
Malar |
Ortho Tri-Cyclen® (norgestimate/ethinyl estradiol) |
0.18/0.215/0.25 mg norgestimate |
35 µg EE |
1.5 years |
aData on progestin and estrogen content were obtained from http://dailymed.nlm.nih.gov/dailymed/about.cfm. bImprovement of melasma has been ongoing for all patients; it was interrupted in patient 3 by her switch from levonorgestrel-intrauterine device (LNG-IUD) back to MicrogestinTM because patient could not tolerate IUD well.
EE: ethinyl estradiol.
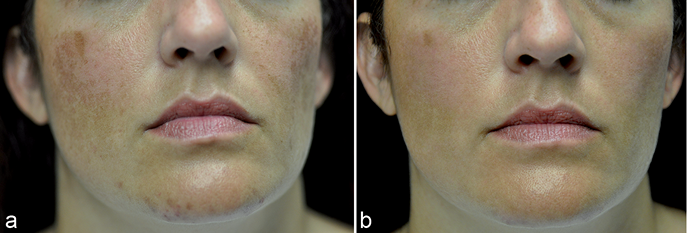
Fig. 1. Patient (No. 3) with melasma while on COCP (a) and after switching to levonorgestrel-releasing intrauterine device (LNG-IUD) (b), taken 5 months after switching to LNG-IUD.
DISCUSSION
Little is known about the incidence of melasma in women using LNG-IUD or non-hormone-releasing IUD. Given the lack of data relevant to melasma in patients on IUD, we posed the question whether melasma can improve when the patient is switched from a COCP to LNG-IUD.
The cases we report here indicate that melasma can improve when the patient is switched from a COCP to LNG-IUD. In an Internet-based survey combining data from the Food and Drug Administration (FDA) and social media reports, only 37 (0.06%) out of the 62,508 patients that reported adverse effects while on the LNG-IUD, had melasma (7). This percentage is significantly lower than the prevalence of melasma reported in several populations (1) and contrasts with the high prevalence of melasma in patients taking OCP, which was 25% in the study by Ortonne et al. (2). The fact that patients typically use LNG-IUD for several years while still having such a low prevalence of melasma in the aforementioned study further supports the lack of association between LNG-IUD use and melasma.
The improvement of melasma observed in our patients may be associated with the higher systemic progestin levels produced by COCPs when compared to those produced by LNG-IUD. LNG is a second-generation progestin (synthetic progestogen) that is used as an active ingredient in OCPs including COCPs, progestogen-only pills, contraceptive implants, and hormone-releasing IUDs (6). The hormone-releasing IUD contains 52 µg LNG, with an initial release rate of 20 µg/day, and a mean release rate of 14 µg/day over the 5-year wearing period (6, 8, 9). This produces extremely low systemic levels (147 ± 59 pg/ml) of LNG (10), while in comparison, there are no OCPs producing systemic progestogen levels in the picogram range. Blood LNG levels in LNG-IUD users are one-tenth those found in OCPs containing 0.1 mg LNG (11) and lower than the levels produced by progestin-only contraceptives and Norplant®, a long-acting subdermal implant that delivers a low daily dose of the same progestin (9). Moreover, the hormonal IUD releases LNG directly into the uterus, and as such its effects are mostly paracrine rather than systemic (9, 11). Most of the hormone stays inside the uterus, and only a very small amount of LNG is systemically absorbed.
The higher potential for triggering melasma among COCPs, when compared to the LNG-IUD, may also be related to the estrogen component of COCPs, since LNG-IUD does not release estrogen. All 4 patients presented took COCPs containing ethinyl estradiol at a fairly consistent level (see Table I). The association of melasma with hormone replacement therapy in post-menopausal women indicates a role for estrogen in melasma pathogenesis (12). Several studies have focused on the importance of hormone receptors in melasma. One study reported an increase in progesterone receptors in the epidermis and an increase in Estrogen Receptor β (ER β) in the dermis of melasma affected skin; ER β expression was observed in particular around fibroblast-like cells and small blood vessels (13). This may be clinically relevant as melasma may also have a vascular component in its pathogenesis (14), and estrogen has a proliferative effect on the vascular tissue, as illustrated by the wide spectrum of vascular changes during gestation (15). Therefore, it is possible that LNG-IUD may be less melasma-stimulating because it lacks the systemic effects of the estrogen component.
In sum, we present 4 patients whose melasma improved spontaneously when switched from a COCP to a LNG-IUD device. Further studies are required to clarify whether newer forms of contraception such as LNG-IUD and copper IUD are less melasma-stimulating than COCPs.
The authors declare no conflict of interest.
REFERENCES
