Uta Jappe1, Wolfgang Uter2, Cristiane A. Menezes de Pádua2, Rudolf A. Herbst3 and Axel Schnuch4
1Department of Dermatology, University of Heidelberg, 2Department of Medical Informatics, Biometry and Epidemiology, University of Erlangen,
3Department of Dermatology and Allergology, Klinikum Bayreuth GmbH, and 4Information Network of Departments of Dermatology (IVDK), University of Goettingen, Germany
Topically applied ophthalmic drugs are a potential cause of allergic contact dermatitis of the periorbital region. The objectives of this study were to assess the frequency
and spectrum of contact allergy to topically applied
β-blocker containing eye drops. Data of the Information
Network of Departments of Dermatology (IVDK) collected between 1993 and 2004 was analysed. Out of 112,430 patch-tested patients, 332 had been tested with their
own topical anti-glaucoma eye drops containing different β-blockers because of suspected allergic contact dermatitis. The frequency of positive test reactions was related to exposure intensity, as estimated by annual prescription rates in Germany. A total of 43/332 (12.95%) showed at least one positive patch test reaction. Positive reactions were observed to products containing timolol (n = 21), metipranolol (n = 13) and levobunolol (n = 11) without conceivable cross-reactivity. Whereas exposure to β-blocker-containing eye drops remained stable over the years, as estimated by the prescription rates, a slight, non-significant increase in positive patch-reactions to these substances was noted. This is the first systematic analysis of a large set of data on patients’ own β-blocker topical medications, the results indicating that contact allergy should be considered as important, if rare, adverse event caused by this family of drugs. Key words: allergic contact dermatitis; β-blocker; cross-reaction; eye drops; eyelid dermatitis; glaucoma; own medicaments.
(Accepted June 8, 2006.)
Acta Derm Venereol 2006; 86: 509–514.
Uta Jappe, MD, MSc, Department of Dermatology, University of Heidelberg, Voßstrasse 2, DE-69115 Heidelberg, Germany. E-mail: Uta_Jappe@med.uni-heidelberg.de
Cutaneous reactions to ophthalmic drugs are usually mild and transitory. Causative agents include preservatives (e.g. thimerosal or benzalkonium chloride) and a large number of pharmaceutical compounds (antibiotics, sympathomimetics, sympatholytics, cholinergics, cholinolytics, antiallergics, antivirals, local anaesthetics, local antihistamines, corticosteroids, antiphlogistics, and β-blockers) (1, 2). Contact allergy after topical administration of anti-glaucoma agents is apparently rare. β-blockers (timolol, metipranolol, levobunol, betaxolol, and carteolol (Fig. 1) are used in cases of pathologically increased intraocular pressure and manifest glaucoma, because of their efficacy and relatively low incidence of systemic side-effects, such as hypotension, bradycardia and bronchospasm (3, 4).
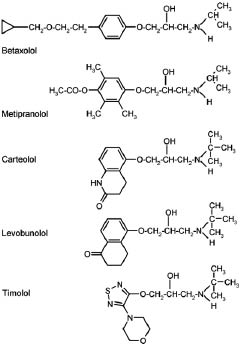
Fig. 1. Chemical structure of various β-blockers.
However, local adverse events in terms of skin reactions also occur. Initially, it may be difficult to distinguish between irritant contact dermatitis and allergic contact dermatitis. Allergic contact conjunctivitis and dermatitis from eye drops have previously been found to be due to preservatives, especially benzalkonium chloride, sodium EDTA and thimerosal (5, 6). However, according to recent reports in the literature, the culprit agents have changed over the years: the pharmacologically active ingredients now seem to play the major role as contact sensitizers, whereas preservatives usually remain negative in diagnostic allergy testing (7–10). Moreover, allergic reactions to ophthalmic drugs are probably more frequent than described in the literature so far. Diagnostic efforts to identify an alternative agent tolerated by the patient allergic to one β-blocker, led to the observation of delayed-type cross-reactivity between levobunol and carteolol, levobunol and timolol, levobunol and befunolol, befunolol and metipranolol, metipranolol and 1-penbutolol, and befunolol and carteolol in several cases, the development of cross-reactions so far not being predictable (11–19). Furthermore, it is a question if previous exposure to the “cross-reacting” compound (and concomitant sensitization) was excluded in every case of assumed cross-reaction. Thus, in the present analysis, we aimed to describe the frequency and pattern of (cross-) sensitization to β-blocker eye drops among patients on topical treatment for glaucoma, who were patch-tested with their eye drops in the departments of IVDK (Information Network of Departments of Dermatology) (www.ivdk.org) – between 1993 and 2004 because of suspected allergic contact dermatitis to these products.
MATERIALS AND METHODS
Study population
From 1993 to 2004, 112,430 patients altogether were patch-tested in the departments of dermatology comprising the IVDK. The IVDK is a multicentre surveillance system on contact allergies, with more than 40 departments of dermatology in Germany, Austria and Switzerland participating. Patch test results and history of all patients tested are recorded electronically in a standardized way, and transferred regularly to the IVDK data centre at the University of Goettingen (20). A total of 332/112,430 patients were on topical treatment with anti-glaucoma drugs, suspected to have contact dermatitis to the eye drops and thus patch-tested with these eye drops. Data analysis is based on these 332 patients.
Patch test procedure
Patch tests were performed according to the international guidelines of the ICDRG (21) further extended by the German
Contact Dermatitis Research Group (22). Commercially available patch test substances were obtained from Hermal (Reinbek, FRG); however, up to now, β-blocking agents are not commercially available as pure test substance to the best of our knowledge. Patch test exposure time was 2 days for
250 of the 332 patients and one day for the remainder, according to the routine test procedure in the respective centre. Results presented on β-blockers are based on readings between D3 and D7 after the application of patch test material. It should be noted that, according to current guidelines (22) all tests were read until D3. In several instances, but not routinely, readings were continued until D7.
While standardized patch test series have routinely been applied in virtually all the patients considered, this analysis focuses on patients’ own medications (Table I) and those ingredients of relevant eye drop brands available as standardized, commercial allergens (Table II).
Table I. Patch tests results of 332 patients tested with their own β-blocker containing eye drops in the Information Network of Departments of Dermatology centres from 1993 to 2004
| β-blocker | Patients n | Positive n (%) | 95% CI |
| Betaxolol | 25 | 0 | 0.0–11.3 |
| Carteolol | 13 | 0 | 0.0–20.6 |
| Levobunolol | 84 | 11 (13.1) | 6.7–22.2 |
| Metipranolol | 86 | 13 (13.3) | 7.2–21.4 |
| Timolol | 189 | 21 (11.1) | 7.0–16.5 |
CI, confidence interval.
Data handling and statistics
Data analysis was done using the statistical program system SAS (version 8.2, SAS Institute, Cary, NC, USA) (20). Important demographic characteristics of a patch test population are
summed-up by the MOAHLFA index (23).
Proportions (frequency of sensitization to β-blocker-containing eye drops) were supplemented with an exact 95% confidence interval (CI) based on the binomial distribution (24). The degree of concordance between positive reactions to β-blockers (e.g. due to immunological cross-reactivity) or other patient’s own eye drops used as anti-glaucoma drugs was quantified using Cohen’s kappa.
Share of the market analysis
Information on ophthalmic specialties containing β-blockers on the German market from 1993 to 2004 was retrieved from a list of drug specialties (25). The prescription rate of the major brand specialties commercialized in Germany in the same period in terms of “defined daily doses” (DDD) was determined based on another reference (26).
RESULTS
Important demographic characteristics of the subgroup of β-blocker positively patch-tested ophthalmic patients according to the MOAHLFA-index are: Males (n=16, 37.2%), Occupational dermatosis (n=0), Atopic Dermatitis (n=2, 4.7%), Hand dermatitis (n=0), Leg dermatitis (n=0), Face dermatitis (n=34, 79.1%), >=40 years of Age (n=41, 95.3%) – note that information on site or occupational causation may have referred to concurrent contact dermatitis due to other causes.
In 59.4% of the patients, allergic contact dermatitis to ophthalmics was “strongly suspected” prior to patch testing, based on the clinical picture at presentation and on past history. In contrast, in 32.1% of the cases, patch-testing was performed only to rule out contact allergy. In 28 patients (8.5%), other reasons for patch- testing were given.
A total of 153 out of 332 patients (46.1%) showed positive patch test reactions to commercial test substances, including metals, fragrances, and a number of other common allergens (data not shown). As these allergens are unrelated to the use of β-blocker containing eye drops and the elicitation of (suspected allergic) contact dermatitis to these eye drops, these test results are considered uninformative and are, therefore, not shown.
In total, 43/332 patients tested with their own eye drops were positive for at least one product (Table I).
Although the proportion of patients testing positive (range 0–16.3%) increased somewhat during the study period, albeit with marked variability, this was not a significant trend (p = 0.057, Cochran-Armitage trend test).
Patient’s own β-blocker-containing eye drops comprised several brand specialties, which also contained different adjuvants. Among these, however, only benzalkonium chloride, sodium EDTA and sodium disulphite were additionally tested. Although at present not included in such commercial preparations, thimerosal was also patch-tested, since it is still present as preservative in other eye drops. The patch tests results with these substances are presented in Table II.
Table II. Results of patch testing four common adjuvants of eye drops in patients positive for β-blockers (Group 1, n = 43) and patients tested with their own β-blockers 1993–2004 in the Information Network of Departments of Dermatology (readings 3 days after application of patch test)
| β-blocker positive (n = 43) | β-blocker negative (n = 289) | ||||||||
| No. of patch tests | No. of positives | % pos. tests | 95% CI | No. of patch tests | No. of positives | % pos. tests | 95% CI | ||
| Benzalkonium chloride | 40 | 0 | 0.0 | 0.0–7.2 | 257 | 2 | 0.8 | 0.0–2.8 | |
| Sodium disulphite | 39 | 0 | 0.0 | 0.0–7.4 | 240 | 9 | 3.8 | 1.7–7.0 | |
| Thimerosal | 39 | 3 | 7.7 | 1.6–20.9 | 254 | 8 | 3.1 | 0.1–6.1 | |
| Sodium EDTA | 39 | 0 | 0.0 | 0.0–7.4 | 241 | 0 | 0.0 | 0.0–1.2 | |
CI, confidence interval; EDTA, ethylene diamine tetra-acetic acid.
Potential cross-reactivity between β-blocker containing products was assessed, as far as patients have been patch-tested with more than one product (Table IIIa). Concordance was limited: κ = 0.34 (95% CI 0–0.91) between levobunolol and timolol, and κ = 0.21 (95% CI 0–0.65) between metipranolol and timolol. Moreover, simultaneous positive reactions to other anti-glaucoma drugs – dorzolamide, a carbonic anhydrase inhibitor, and latanoprost, a prostaglandin analog were descriptively analysed in those few cases tested with the two respective drugs (Table IIIb).
Table III. Concomitant positive reactions to more than one β-blocker (a) and concomitant positive reactions of β-blockers and other anti-glaucoma drugs patch-tested (b) in the Information Network of Departments of Dermatology centres 1993–2004
| Positive | Negative | ||
| (a) Potential immunological cross-reactivity | Timolol | ||
| Levobunolol | Positive | 1 | 1 |
| Negative | 2 | 23 | |
| Metipranolol | Positive | 1 | 4 |
| Negative | 1 | 24 | |
| (b) Other anti-glaucoma drugs | Levobunolol | ||
| Dorzolamide | Positive | 1 | 1 |
| Negative | 0 | 0 | |
| Timolol | |||
| Dorzolamide | Positive | 2 | 3 |
| Negative | 0 | 0 | |
| Latanoprost | Positive | 1 | 1 |
| Negative | 1 | 4 | |
Table IV presents the prescription rate of eye drops containing β-blockers (mono drugs and combinations) commercialized in Germany. Those eye drops including timolol had been prescribed more often than other β-blocking agents. In general, the prescription rate of β-blocker preparations was quite steady during the 12-year period.
In the clinical sample of 332 patients, allergic contact
dermatitis caused by topical drugs (including expo
sures other than to β-blocker containing eye drops) was suspected in 156 (47%); in the remainder allergic contact dermatitis was to be excluded, or other exposures were considered more important. In 25 of these 156 patients, this clinical suspicion was confirmed (positive predictive value 16%). Conversely, among those 176 patients without – strongly – suspected allergic contact dermatitis to topical drugs, the patch test with β-blocker containing eye drops was indeed negative in 158 (negative predictive value: 90%).
Table IV. Prescription rate of β-blocker eye drops in Germany over a 12-year period. Average of the number of prescriptions in Defined Daily Dose (1 DDD = 0.2 ml) and the relative market share is represented for each 2-year period (26)
| Year | ||||||
| β-blocker | 1993–1994 | 1995–1996 | 1997–1998 | 1999–2000 | 2001–2002 | 2003–2004 |
| DDD in million (%) | ||||||
| Betaxolol | 8.0 (3.9) | 9.2 (4.1) | 8.2 (3.8) | 7.3 (3.4) | 5.7 (2.6) | 4.2 (1.9) |
| Carteolol | 14.6 (7.1) | 12.5 (5.5) | 8.6 (4.0) | 6.7 (3.1) | 5.1 (2.3) | 3.6 (1.6) |
| Levobunolol | 21.8 (10.6) | 24.3 (10.8) | 23.0 (10.6) | 20.5 (9.5) | 15.4 (6.9) | 11.6 (5.3) |
| Metipranolol | 42.1 (20.5) | 39.4 (17.4) | 33.3 (15.3) | 28.0 (12.9) | 24.0 (10.8) | 19.9 (9.1) |
| Timolol | 118.4 (57.8) | 140.7 (62.2) | 144.4 (66.4) | 154.0 (71.1) | 172.5 (77.5) | 179.9 (82.1) |
| Total | 204.9 | 226.1 | 217.5 | 216.5 | 222.7 | 219.2 |
DISCUSSION
β-blocker containing eye drops may induce irritant as well as allergic contact dermatitis, the latter being rarely
reported. The rarity of positive patch test results to patients’
own medicaments which are first-line treatment topical ophthalmics was considered to be due to their inherently low sensitizing potential. However, the true prevalence of contact sensitization to topically applied β-blockers may be higher than suggested from literature reports. Since ophthalmic series containing β-blockers are not commercially available, patients’ own substances have to fill this diagnostic gap. However, these are either not regularly included in the patch tests in cases of periorbital dermatitis in the first place, or they may produce false-negative results. The latter may be due to a suboptimal test concentration or a suboptimal test procedure (27).
Few investigations have been performed assessing the value of patch-testing patients’ own cosmetics, toiletries and medicaments (28, 29). One of them had focussed on allergic and non-allergic periorbital dermatitis, revealing that in 4% of cases only, patients’ own substances, including ophthalmics, had been tested (29).
The present study is, to our knowledge, thus the first systematic analysis of a large set of data on patients’ own β-blocker topical medication, assessing the frequency and spectrum of contact allergy to topically applied β-blockers. It revealed contact allergy to at least one β-blocker in 43/332 cases (12.95%), indicating that contact allergy is not an entirely exceptional event. Whereas early reports point to preservatives, for example, as culprit agents, reports documenting the active ingredient as contact allergen are increasing in number, which is in accordance with our own results: most β-blocker containing eye drops are preserved with benzalkonium chloride. However, none of the tested individuals were positive to this ingredient. Only a small number of tested patients reacted to thimerosal. However, this preservative is not used in the commercial preparations of β-blocker containing eye drops we have analysed.
For the first time the question of possible cross-reactivity can be addressed based on a larger group of patients tested. Several case reports diagnosed contact sensitization to only one β-blocker without cross-reactions between topical substances of this group (30) as well as between systemic and topical β-blockers (31), several others, however, observed different patterns of concomitant β-blocker contact allergy. In some cases, sensitization to another β-blocker was observed after having used it as alternative treatment for some time, indicating subsequent sensitization (co-sensitization) rather than immunologic cross-reactivity. Two groups observed patch test reactions to β-blockers which had never been used by the patient, indicating true cross-reactions: the first between befunolol/carteolol (19), the second observed a delayed-type reaction to timolol, subsequent sensitization to carteolol with additional positive patch test reaction to levobunol, which had never been used (18).
However, in our investigation concomitant reactions were rare, namely to timolol and levobunol as well as to timolol and metipranolol, in the subset of patients tested with both agents. This pattern is not surprising, because it is the most probable in view of the use of these three drugs (Table IV). Due to the small size of our sample of patients tested with the two respective drugs, substantial concordance can neither be confirmed nor excluded (the 95% CIs to the κ estimate include 0). As a practical consequence, in a situation where compelling evidence regarding relevant structural similarity of topically used β-blockers is lacking, the patient should probably best tested not only with the culprit agent, but also with possible alternative preparations, to try to rule out contact allergy to the other compounds.
Some 9000 patients have been patch-tested each year in the German centres of the IVDK network. Related to the total number of patch tests performed in Germany each year – estimated to range between 600,000 (32) and 390,000 in the more recent years (data on file) – this is a proportion of 1.5% to 2.3%. Under the assumption that the proportions of patients presenting with periorbital dermatitis and their spectrum of causative allergens do not differ substantially between the IVDK centres and the remaining dermatologists, the average of 3.58 cases seen per year in the IVDK could thus be extrapolated to a total of 157–239 cases testing positive to their own β-blocker eye drops each year on a population level. Related to 205–226 million DDD per year (Table IV), this does appear as a relatively low incidence of this adverse event ((less than) one per million DDDs), compared with, for example, the similarly estimated 6000 annual cases of contact allergy to the topical agent bufexamac, related to 12.532 million DDDs (479 cases per one million DDDs) (33). However, the true incidence of allergic contact dermatitis to β-blocker eye drops may be underestimated, as patients with periorbital allergic contact dermatitis due to this medication may not always consult a dermatologist, but merely be switched to an alternative agent by their ophthalmologist. Regarding allergic contact dermatitis in general, it has been estimated that only 15–38% of all affected persons consult a dermatologist (32).
Despite the much higher prescription rate of timolol-containing eye drops between 1993 and 2004 (Table IV), the frequency of sensitization to this drug was close to the frequency observed for levobunolol and metipranolol in the same period. Hence, with some caution owed to the overall small numbers of cases, risk assessment with regard to contact allergy is obviously more favourable in case of timolol, compared with the other two agents.
In the routine documentation of the IVDK eye drops, or even β-blocker containing eye drops, are not specifically listed as suspected exposure, but merely “topical drugs”. Hence, the true positive predictive value of the clinical suspicion of causation, as evaluated against the subsequent patch test result with these particular topical drugs may be somewhat underestimated. However, the fact that these eye drops were patch tested at all may indicate at least some degree of suspicion in any of the cases. From this background, the yield of confirmative positive patch test reactions seems surprisingly low. This may indicate that the clinical suspicion can indeed be ruled out by patch testing in a certain number of cases; however, the low positive predicted value may also be due to a certain proportion of false-negative patch tests with β-blocker containing eye drops. Thus, validation tests like repeated open application test or a “stop-re-start test”, if feasible, are recommendable in those cases where the patch test results do not seem to be in accordance with the patient’s history and/or the presented clinical symptoms.
In conclusion, contact allergy should be considered an important, if rare adverse event of β-blocker-containing eye drops, false-negative patch test-results probably being of relevance due to the fact that test procedures so far have not been standardized. However, this study demonstrates the diagnostic value of patch testing patients’ own substances where standardized allergens are not available.
ACKNOWLEDGEMENTS
The following departments of dermatology, all members of the German Contact Dermatitis Research Group (DKG), contributed to this study: Aachen (H. Dickel, S. Erdmann), Augsburg (A. Ludwig), Berlin Benjamin-Franklin (B. Tebbe, R. Treudler), Berlin Charité (B. Laubstein, T. Zuberbier, M. Worm), Berlin UKRV (J. Grabbe, T. Zuberbier), Dortmund (P.J. Frosch, B. Pilz, C. Pirker, R. Herbst), Dresden (G. Richter, R. Aschoff), Duisburg (J. Schaller), Erlangen (K.-P. Peters, Th. Diepgen, M. Fartasch, V. Mahler), Essen (H.-M. Ockenfels, U. Hillen), Göttingen (Th. Fuchs, J. Geier), Graz (W. Aberer, B. Kränke), Halle (G. Gaber, D. Lübbe), Hamburg (M. Kiehn, D. Vieluf, R. Weßbecher), Heidelberg (M. Hartmann, U. Jappe, A. Schulze-Dirks), Homburg / Saar (P. Koch), Jena (M. Gebhardt, A. Bauer, W. Wigger-Alberti, S. Schliemann-Willers), Kiel (J. Brasch), Lübeck (J. Kreusch, J. Grabbe), Magdeburg (U. Beier, B,
Stötzel, R. Vetter, U. Jappe), Mainz (D. Becker), Mannheim (Ch. Bayerl), Marburg (I. Effendy, H. Löffler), München Schwabing (M. Agathos), München TU (J. Rakoski), Nürnberg (I. Müller),
Osnabrück (N. Schürer, H. J. Schwanitz , W. Uter, S.M. John),
Rostock (H. Heise), Tübingen (G. Lischka, T. Biedermann), Ulm (H. Gall, P. Gottlöber, G. Staib, H. Pillekamp, R.
Hinrichs), Wuppertal (O. Mainusch, J. Raguz, B. Dierbach)
REFERENCES
1. Herbst AR, Maibach IH. Contact dermatitis caused by allergy to ophthalmic drugs and contact lens solutions. Contact Dermatitis 1991; 25: 305–312.
2. Jappe U, Niebrügge B, Gollnick H. Allergische Reaktionen am äußeren Auge. Teil I: Kontaktallergie (Typ IV-Reaktionen). Der Augenspiegel 1997; 5: 29–33.
3. Nelson WL, Fraunfelder FT, Sills JM, Arrowsmith JB, Kuritsky JN. Adverse respiratory and cardiovascular events attributed to timolol ophthalmic solution, 1978–1985. Am J Ophthalmol 1986; 102: 606–611.
4. Faunfelder FT. Ocular beta-blockers and systemic effects. Arch Intern Med 1986; 146: 1073–1074.
5. Tosti A, Tosti G. Allergic contact conjunctivitis due to ophthalmic solution. In: Frosch PJ, Dooms-Goossens A, Lachapelle JM, Rycroft RJG, Scheper RJ, eds. Current topics in contact dermatitis. Berlin: Springer-Verlag, 1989: p. 269–272.
6. Katz IM. Beta blockers and the eye: an overview. Ann Ophthalm 1978, 10: 847–850.
7. Fernandez Vozmediano JM, Blasi NA, Romero Cabrera MA, Carrascosa Cerquero A. Allergic contact dermatitis to timolol. Contact Dermatitis 1986; 14: 252.
8. Romaguera C, Grimalt F, Vilaplana J. Contact dermatitis by timolol. Contact Dermatitis 1986; 14: 248.
9. Cameli N, Vicenzi C, Tosti A. Allergic contact conjunctivitis due to timolol in eyedrops. Contact Dermatitis 1991; 25: 129–130.
10. der Meeren HLM van, Meurs PJ. Sensitization to levobunolol eyedrops. Contact Dermatitis 1993; 28: 41–42.
11. Van Joost T, Middelkamp Hup J, Ros FE. Dermatitis as a side effect of long-term topical treatment with certain beta-blocking agents. Br J Dermatol 1979; 101: 171–176.
12. DeGroot AC, Conemans J. Contact allergy to metipranolol. Contact Dermatitis 1988; 18: 107–108.
13. Gailhofer G, Ludvan M. Beta-blockers: sensitizers in periorbital allergic contact dermatitis. Contact Dermatitis 1990; 23: 262.
14. Corazza M, Virgili A, Mantovani L, Masieri LT. Allergic contact dermatitis from cross-reacting beta-blocking agents. Contact Dermatitis 1993; 28: 188–189.
15. O’Donnell BF, Foulds IS. Contact allergy to beta-blocking agents in ophthalmic preparations. Contact Dermatitis 1993; 28: 121–122.
16. Zucchelli V, Silvani S, Vezzani C, Lorenzi S, Tosti A. Contact dermatitis from levobunolol and befunolol. Contact Dermatitis 1995; 33: 66–67.
17. Förster W. Allergisches Kontaktekzem auf Levobunolol und Timolol in der Glaukombehandlung. Derm 1997; 3: 130–131.
18. Quiralte J, Florido F, de-San-Pedro BS. Allergic contact dermatitis from carteolol and timolol in eyedrops. Contact Dermatitis 2000; 42: 245.
19. Nino M, Suppa F, Ayala F, Balato N. Allergic contact dermatitis due to the beta-blocker befunolol in eyedrops, with cross-
sensitivity to carteolol. Contact Dermatitis 2001; 44: 369.
20. Uter W, Schnuch A, Geier J, Frosch PJ. The epidemiology of contact dermatitis – the Information Network of Departments of Dermatology (IVDK) in Germany. Eur J Dermatol 1998; 8: 36–40.
21. Wahlberg JE. Patch Testing. In: Rycroft RJG, Menné T, Frosch PJ, Lepoittevin J-P. eds. Textbook of contact dermatitis, 3rd edn. Berlin: Springer, 2001: p. 435–468.
22. Schnuch A, Aberer W, Agathos M, Brasch J, Frosch PJ, Fuchs Th, Richter G für die Deutsche Kontaktallergie-Gruppe. Leitlinien der Deutschen Dermatologischen
Gesellschaft (DDG) zur Durchführung des Epikutantests mit Kontaktallergenen. Hautarzt 2001; 52: 864–866.
23. Schnuch A, Geier J, Uter W, Frosch PF, Lehmacher W, Aberer W, et al. National rates and regional differences in sensitization to allergens of the standard series. Population adjusted frequencies of sensitization (PAFS) in 40,000
patients from a multicentre study (IVDK). Contact Dermatitis
1997; 37: 200–209.
24. Uter W, Schnuch A, Gefeller O. Guidelines for the descriptive presentation and statistical analysis of contact allergy data. Contact Dermatitis 2004; 51: 47–56.
25. Anonymus. Rote Liste 2004. ECV: Aulendorf, 2004.
26. Schwabe U, Paffrath D. Arzneiverordnungs-Report 2004. Berlin: Springer, 2004.
27. Sanchez-Perez J, Del Rio MJ, Fernandez-Villalta MJ, Garcia-Diez A. Positive use test in contact dermatitis from betaxolol hydrochloride. Contact Dermatitis 2002; 46; 313–314.
28. Uter W, Balzer C, Geier J, Frosch PJ, Schnuch A. Patch testing with patients’ own cosmetics and toiletries – results of the IVDK, 1998–2002. Contact Dermatitis 2005; 53: 226–233.
29. Herbst RA, Uter W, Pirker C, Geier J, Frosch PJ. Allergic and non-allergic periorbital dermatitis: patch test results of the Information Network of the Departments of Dermatology during a 5-year period. Contact Dermatitis 2004; 51: 13–19.
30. Koch P. Allergic contact dermatitis due to timolol and levobunolol in eyedrops, with no cross-sensitivity to other ophthalmic beta-blockers. Contact Dermatitis 1995; 33: 140–141.
31. Fedele R, Ricciardi L, Mazzeo L, Isola S. Allergic contact dermatitis to nebivolol. Allergy 2002; 57: 864–865.
32. Schnuch A, Uter W, Geier J, Gefeller O. Epidemiology of contact allergy: an estimation of morbidity employing the clinical epidemiology and drug-utilization research (CE-DUR) approach. Contact Dermatitis 2002; 47: 32–39.
33. Schnuch A, Gefeller O, Uter W. Eine heimtückische und häufige Nebenwirkung: Das Ekzemtherapeutikum Bufexamac verursacht Kontaktallergien. Ergebnisse des IVDK. Dtsch Med Wochenschr 2005; 130: 2881–2886.
