OBJECTIVE: Cardiac rehabilitation remains grossly under-utilized despite its proven benefits. This study prospectively compared verified cardiac rehabilitation enrollment following automatic vs usual referral, postulating that automatic referral would result in significantly greater enrollment for cardiac rehabilitation.
DESIGN: Prospective controlled multi-center study.
Patients and methods: A consecutive sample of 661 patients with acute coronary syndrome treated at 2 acute care centers (75% response rate) were recruited, one site with automatic referral via a computerized prompt and the other with a usual referral strategy at the physician’s discretion. Cardiac rehabilitation referral was discerned in a mailed survey 9 months later (n = 506; 84% retention), and verified with 24 cardiac rehabilitation sites to which participants were referred.
RESULTS: A total of 124 (52%) participants enrolled in cardiac rehabilitation following automatic referral, vs 84 (32%) following usual referral (p < 0.001). Automatically referred participants were more likely to be referred from an in- patient unit (p < 0.01), and to be referred in a shorter time period (p < 0.001). Logistic regression analyses revealed that, after controlling for sociodemographic characteristics and case-mix, automatically referred participants were significantly more likely to enroll in cardiac rehabilitation (odds ratio = 2.1; 95% confidence interval 1.4–3.3) than controls.
CONCLUSION: Automatic referral resulted in over 50% verified cardiac rehabilitation enrollment; 2 times more than usual referral. It also significantly reduced utilization delays to less than one month.
Key words: cardiac rehabilitation, automatic referral, access to care.
J Rehabil Med 2007; 39: 239–245
Correspondence address: Sherry L. Grace, York University, 368 Bethune, 4700 Keele St, Toronto, ON, M3J 1P3, Canada. E-mail: sgrace@yorku.ca
Submitted August 25, 2006; accepted November 11, 2006.
INTRODUCTION
Ischemic heart disease is the leading cause of death and disability in the developed world (1). Substantial health risks continue following coronary events and procedures (2, 3), and cardiac rehabilitation (CR) improves subsequent prognosis (4, 5). However, most research demonstrates low enrollment in CR, approximately 15–20% of eligible participants (6, 7). There are a combination of factors relating to patients (6), physicians (8, 9), and the healthcare system itself (10) leading to low CR referral and subsequent enrollment (11).
The literature promotes automatic referral to increase enrollment (12, 13). Automatic referral can be defined as the systematic, non-manual enrollment of all eligible patients with cardiac diseases (based on clinical practice guidelines (14)) from acute care to CR (15). As a health-system level intervention, automatic referral may minimize patient- and physician-related care gaps. To date, this type of referral mechanism has been tested empirically only in non-controlled studies (15–17).
The following study prospectively compares site-verified CR enrollment in a consecutive sample of acute coronary syndrome (ACS) patients automatically or usually referred to CR. This control condition of usual referral occurs non-systematically at the discretion of any physician involved in the patient’s care. It is postulated that automatic referral will result in significantly greater verified enrollment than usual referral mechanisms.
METHODS
Procedure and design
The Trillium Health Centre is a large, urban tertiary care facility in the Greater Toronto Area, Ontario, Canada, which offers advanced cardiac services. The automatic referral model implemented at this centre uses hospital electronic patient records to prompt the standard order for a CR referral for all eligible patients with cardiac diseases (based on American Association of Cardiovascular and Pulmonary Rehabilitation and Canadian Association of Cardiovascular Rehabilitation (CACR) guidelines (14, 18). This discharge order is initiated on the inpatient ward and printed on a hospital network printer in the CR center and again screened for eligibility. An information package, including a personalized letter stating the name of the referring physician, a program brochure, a schedule of classes, and a request that the patient telephone to book an appointment, is mailed to the patient’s home. Patients who live outside of the geographic area are also sent a similar package, but they are provided with the contact information of the site closest to their home. This alternate site is also sent the patient’s contact information.
Automatic referral at Trillium Health Centre was compared with usual referral practices at University Health Network, a network of large teaching hospitals also offering advanced cardiac services, located in urban Toronto, Ontario. This involves referral to CR at the discretion of the cardiologist, cardiovascular surgeon, general practitioner, or other healthcare provider through paper-based means.
This study constituted a prospective controlled design. Ethics approval was obtained from participating centers. Participants were followed from admission for their index ACS hospitalization for 9 months. Consecutive patients with ACS were recruited on relevant cardiovascular units by a research assistant when medically stable. Inclusion criteria were diagnosis with a confirmed myocardial infarction (MI), unstable angina (UA), ischemic congestive heart failure (CHF), percutaneous coronary intervention (PCI), or acute coronary bypass (ACB), and at least 18 years of age. Exclusion criteria included being medically unstable, too confused to participate, previous participation in CR, being ineligible for CR based on CACR guidelines due to musculoskeletal, vision, psychiatric, or other co-morbidities, or being unable to read or speak English. Those who met study criteria and agreed to participate signed a consent form and were provided with a self-report questionnaire. Consent was also obtained to link participant’s self-report questionnaire data with their clinical data.
Nine months later, participants completed a second survey to discern CR referral and participation. CR centers to which participants self-reported referral were then contacted to verify referral, enrollment and participation.
Participants
A total of 1362 consecutive patients who were diagnosed with an MI, UA, CHF, or who had undergone PCI or ACB at Trillium Health Centre or University Health Network between September 2003 and August 2004 were approached for the study. Of these patients, 661 consented to participate and 483 were ineligible for the study (response rate= 661/(1362–483) = 75%). Reasons for ineligibility were as follows: previous attendance at CR (n = 123; 25.5%), lack of English language proficiency (n = 119; 24.6%), too ill to participate (n = 98, 20.3%), condition not indicated for referral to CR (n = 70; 14.5%), patients too confused or experiencing cognitive impairment (n = 42; 8.7%), co-morbid musculoskeletal condition which precludes ambulation (n = 19; 3.9%), or patient already participating in 2 studies (n = 5, 1.0%). Other reasons (n = 7, 1.4%) included isolation for infection control, physician who would be aware of cardiac care guidelines, and moving to another province.
Characteristics of participants and non-participants are shown in Table I. There were no significant differences in participant status based on site of recruitment or marital status. Of the patients approached, participants were significantly younger than those who refused or were ineligible to participate (F (2) = 33.59, p < 0.001; post hoc least significant difference (LSD) ps < 0.001). Significantly more males agreed to participate than females (χ2 (2) = 31.44, p < 0.001).
| Table I. Characteristics of participants, refusers, and ineligibles at baseline recruitment. |
| Characteristic | Participants (n = 661) | Refusers (n = 218) | Ineligibles (n = 483) |
| Participants from THC, n (%) | 331 (50.1) | 126 (59.8) | 271 (56.1) |
| PCIa, n (%) | 405 (61.3) | 109 (50.2) | 184 (38.3)* |
| Females, n (%) | 157 (23.8) | 77 (35.6) | 186 (38.6)* |
| Marital status: married, n (%) | 503 (76.1) | 160 (76.2) | 339 (71.5) |
| Age, mean (SD) (years) | 61.22 (11.30) | 65.96(11.96)* | 66.48(11.39)* |
| *p < 0.001. aExtracted from medical charts. THC: Trillium Health Centre with automatic referral; PCI: percutaneous coronary intervention. |
Measures
CR referral, enrollment and participation. Participants self-reported whether they were referred to CR, by whom, whether they attended a CR assessment and at which site, whether or not they participated in CR, and provided an estimate of the percentage of sessions they attended. In addition to these forced choice questions, participants who did not enroll in CR were asked to explain why in open-ended format. Twenty-four CR centers were contacted to verify the receipt of referrals (yes/no, date), participant enrollment or attendance at intake appointment (yes/no; main dependent variable), and program completion (yes/no, date, percentage of program attended).
Independent variables. Sociodemographic data assessed in the baseline survey included age, sex, ethnocultural background, marital status, work status, level of education, and gross annual family income. Two “yes/no” response items were created to assess participants’ past exercise habits (“Did you exercise to the point of getting short of breath on a regular basis (as an adult) prior to your cardiac event?”) and co- morbidities that might interfere with an exercise regime (“Do you have any other medical conditions that would prevent you from exercising?”). Body mass index (BMI) was computed based on self-reported height and weight (kg/m2). Participants were asked if they were current, past or non-smokers. Data were extracted from clinical charts including confirmation of reason for index hospitalization, disease severity (New York Heart Association (NYHA) Class (19)), and presence of selected co-morbid conditions (i.e. diabetes, arthritis).
The Duke Activity Status Index (20) is a brief 12-item self-administered survey to determine functional capacity. This measure was incorporated as a self-report indicator of disease severity. Participants were asked about their ability to perform common activities of daily living, such as personal care, ambulation, household tasks, sexual function and recreational activities, which are each associated with specific metabolic equivalents. This valid and common tool correlates highly with peak oxygen uptake (21).
Statistical analysis
SPSS 12.0 was used for the following analyses. Following data cleaning and screening, a descriptive examination was performed and open-ended responses were coded. Differences between participating, ineligible and refusing patients were tested by Pearson’s χ2 test and analyses of variance, as appropriate. A descriptive and inferential examination of CR referral, enrollment and participation patterns followed, and was compared by type of referral through t-tests and χ2 analyses. Finally, a hierarchical logistic regression analysis predicting verified enrollment was performed. We controlled for variables which may have biased the generalizability of our sample at step 1, and entered the variable type of referral in step 2.
RESULTS
Respondent characteristics
Characteristics of study participants based on site of recruitment are shown in Table II. As displayed, participants did not differ on any variable except index cardiac condition.
| Table II. Descriptive characteristics of the study sample by type of cardiac rehabilitation (CR) referral. |
| Characteristic | UHN Usual (n = 330) | THC Automatic (n = 331) | Total (n = 661) |
| PCI, n (%) | 251 (76.1) | 154 (46.5) | 405 (61.3)** |
| Males, n (%) | 251 (76.1) | 253 (76.4) | 504 (76.2) |
| Ethnocultural background: white, n (%) | 247 (82.6) | 262 (81.1) | 509 (81.8) |
| Marital status: married, n (%) | 246 (74.5) | 257 (77.6) | 503 (76.1) |
| Current daily activity, n (%) Employed full-time Retired | 158 (47.9) 118 (35.8) | 144 (43.8) 140 (42.6) | 302 (45.8) 258 (39.2) |
| Education: some postgraduate, n (%) | 177 (53.6) | 163 (50.6) | 340 (52.1) |
| Family income: ≥ $50 000 CADa, n (%) | 142 (56.3) | 157 (53.2) | 299 (54.7) |
| No regular history of exercise to the point of shortness of breath, n (%) | 224 (70.7) | 230 (71.9) | 454 (71.3) |
| NYHA Class 1, n (%) | 258 (86.9) | 298 (90.9) | 556 (89.0) |
| Diabetes, n (%) | 83 (25.5) | 71 (21.5) | 154 (23.4) |
| Duke Activity Status Index, mean (SD) | 35.88 (16.94) | 32.92 (17.35) | 33.81 (17.38)* |
| Age, mean (SD) (years) | 60.65 (10.6) | 61.78 (11.91) | 61.21 (11.30) |
| Body mass index, mean (SD) | 28.93 (5.23) | 28.25 (.84) | 28.59 (5.05) |
| *p < 0.05; **p < 0.001. aEquivalent to approximately $28,500 USD. UHN: University Health Network; THC: Trillium Health Centre; PCI: percutaneous coronary intervention; NYHA: New York Heart Association; CAD: Canadian dollar. |
Of the 661 consenting participants, 61 were ineligible and 506 were retained at the 9-month assessment (retention rate = 506/600 = 84.3%). Reasons for ineligibility were as follows: unable to reach/incorrect contact information (n = 34; 5.1%), too ill to participate (n = 10; 1.5%), deceased (n = 8; 1.2%); and other reasons (n = 9; 1.4%) included onset of conditions which precluded eligibility for CR.
Characteristics of participants and those who refused or were ineligible at 9 months are summarized in Table III. Retained participants were more likely to have had PCI as their index event, to be married, to be older, to have a lower BMI, to be a non-smoker, to describe their ethnocultural background as white, and to have greater family income than non-participants.
| Table III. Characteristics of participants, ineligibles, and refusers at 9-month follow-up assessment. |
| Characteristic | Participants (n = 506) | Refusers (n = 94) | Ineligibles (n = 61) |
| Participants from THC, n (%) | 241 (47.6) | 57 (60.6) | 33 (54.1) |
| PCI, n (%) | 316 (62.5) | 55 (58.5)** | 31 (50.8)** |
| Female, n (%) | 116 (22.9) | 29 (30.9) | 12 (19.7) |
| Marital status: married or common law, n (%) | 397 (78.5) | 64 (68.1)* | 40 (65.6)* |
| Age, mean (SD) (years) | 62.38 (10.75) | 55.71 (12.35)*** | 60.61 (11.73)*** |
| Body mass index, mean (SD) | 28.31 (4.73) | 29.77 (5.36)* | 29.01 (5.36)* |
| Activity status, mean (SD) | 34.46 (17.18) | 32.65 (18.71) | 29.79 (16.35) |
| NYHAa Class 1, n (%) | 425 (88.7) | 76 (84.4) | 54 (98.2) |
| Diabetes, n (%) | 111 (21.9) | 26 (27.7) | 17 (27.9) |
| Arthritis, n (%) | 116 (22.9) | 22 (23.4) | 17 (27.9) |
| Smoker, n (%) | 73 (14.6) | 24 (25.5)** | 17 (28.3)** |
| Ethnocultural background: white, n (%) | 404 (84.0) | 62 (71.3)* | 42 (79.2)* |
| Education: some postgraduate or greater, n (%) | 258 (51.9) | 50 (53.8) | 31 (50.8) |
| Family income: $50,000CAD, n (%) | 242 (58.3) | 39 (48.8)** | 17 (33.3)** |
| *p < 0.05; **p < 0.01; ***p < 0.001. aExtracted from medical charts. THC: Trillium Health Center; PCI: percutaneous coronary intervention; NYHA: New York Heart Association. |
Self-reported and verified CR referral, enrollment and participation
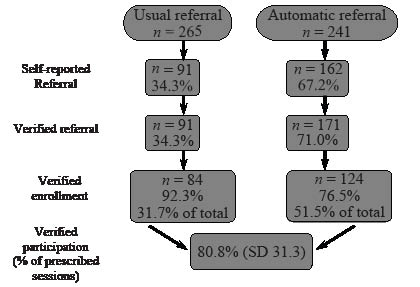
A total of 253 (55.0%) participants self-reported referral to CR. Automatically referred participants were significantly more likely to report referral to CR than were control participants (χ2 = 111.46, p < 0.001; Fig. 1). Thirty (11.3%) control or usual referral participants did not know whether they had been referred, with none unsure following automatic referral. Twenty-eight participants reported that a healthcare provider provided them with a reason why they were not making a CR referral on the patient’s behalf, with no significant differences by site. The most frequent reasons physicians provided to participants were that CR was not needed, travel distance, and that the wait list was too long.
Fig. 1. Referral and enrollment in cardiac rehabilitation (CR) by type of referral.
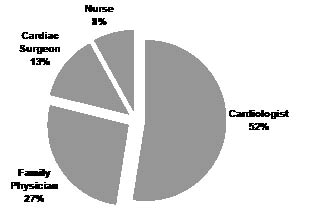
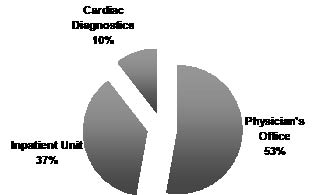
Source of referral is shown in Fig. 2, and other sources included internists and self-referrals. Control participants were significantly more likely to be referred by their family physician than were automatically referred participants (35.0% vs 15.9%; χ2 = 28.03, p < 0.001). Location of referral is shown in Fig. 3. Automatically referred participants were significantly more likely to be referred from an inpatient unit than were control participants (42.9% vs 23.3%; χ2 = 18.84, p = 0.002).
Fig. 3. Location of referral.
A total of 214 participants (46.0%) self-reported attending an intake assessment at 1 of 24 CR centers, with significantly more automatically referred participants (n = 118, 59.9%) self-reporting enrollment than control participants (n = 96, 35.8%; χ2 = 26.50, p < 0.001). Open-ended responses to queries regarding why participants did not attend an assessment were coded. Most participants responded that it was due to lack of referral (n = 59, 30.3%), followed by perception that CR was not needed (n = 36, 18.5%), was too distant or inconvenient (n = 13 6.7%), they had health or mobility issues (n = 13, 6.7%), did not know about CR (n = 11, 5.6%), had time conflicts with paid employment (n = 7, 3.6%), or that they were making lifestyle changes independent of CR services (n = 7, 3.6%). Other responses including not knowing why, not being interested, indirect costs, no capacity for new patients at CR program, and physicians telling patients they did not need CR services.
A total of 199 participants (43.1%) self-reported participating in CR: 181 (94.3%) at a clinic-based program and 11 (5.7%) at a home-based program. Automatically referred participants (n = 109, 55.3%) were significantly more likely to report participation than were control participants (n = 90, 34.0%; χ2 = 21.04, p < 0.001). Participants traveled a mean of 23.9 (SD 18.39) minutes one-way to their CR program (range 2–120 min). Participants reported attending a mean of 79.5 % (SD 27.03) of their CR sessions, with no significant differences by site (p = 0.76).
We contacted all 24 centers to which participants reported CR referral, and also verified receipt of all automatic referrals where Trillium Health Centre participants were referred to CR sites closer to home. We verified 262 referrals (51.8%) for the cohort across these 24 centers, received a mean of 38.19 days (SD 51.60) from hospital admission (median = 30 days). The mean number of days between admission and receipt of referral was significantly shorter following automatic (23.78 (SD 33.9)) vs usual referral (67.63 (SD 67.1); t = 5.15, p < 0.001 equal variances not assumed). Where referrals could not be verified, we conservatively assumed non-enrollment. Attendance at a CR intake assessment was verified for 208 (41.1%) participants, showing that 79.4% of those referred enrolled in CR. Automatically referred participants were significantly more likely to enroll than were control participants (odds ratio = 2.28, 95% confidence interval 1.59–3.38; Fig. 1). The mean number of days between receipt of referral and program completion was 255.26 (SD 105.80) (median = 253 days or approximately 8.4 months). Verified program attendance across all centers was 80.75% (SD 31.27).
Adjusted model predicting CR enrollment
A hierarchical logistic regression analysis was conducted predicting verified CR enrollment (Table IV). Analysis was conducted using SPSS logistic regression. At the first step, variables identified which may bias the sample were entered, and type of referral was entered at step 2. A test of the full model with all variables against a constant-only model was statistically reliable (χ2 (10) = 39.09, p < 0.001), indicating that the variables, as a set, reliably distinguished between those who enrolled in CR and those who did not. Each step of the model reached statistical significance (step 1 χ2 (9) = 28.21, p = 0.001; step 2 χ2 (1) = 10.88, p = 0.001). According to the Wald criterion, type of index event or procedure, family income, and type of referral were significantly associated with verified CR enrollment. Chi-square analyses on the first 2 variables reveal that participants with a family income less than $50,000 Canadian dollars per annum (35.1%) are less likely to enroll than those with higher family income (46.3%; χ2 = 5.21, p = 0.02), and participants with a cardiac event or procedure other than PCI (51.6%) are more likely to enroll than those hospitalized for PCI (34.8%; χ2 = 13.78, p < 0.001). Supporting our hypothesis, type of referral had the greatest odds ratio (2.10) of any variable in the model.
| Table IV. Hierarchical logistic regression predicting cardiac rehabilitation (CR) enrollment, n = 506. |
| Variable | β | Wald | p | OR | 95% CI |
| Index condition / procedure | 0.584 | 6.41 | 0.01 | 1.79 | 1.14–2.82 |
| Activity status | 0.009 | 1.07 | 0.15 | 1.01 | 1.00–1.02 |
| Sex | 0.001 | 0.00 | 0.99 | 1.00 | 0.57–1.77 |
| Age | 0.016 | 2.02 | 0.16 | 1.02 | 0.99–1.04 |
| Marital status | –0.063 | 0.05 | 0.83 | 0.94 | 0.53–1.66 |
| Family income | 0.505 | 4.27 | 0.04 | 1.66 | 1.03–2.67 |
| Ethnocultural background | –0.552 | 2.77 | 0.10 | 0.58 | 0.30–1.10 |
| Body mass index | –0.032 | 1.72 | 0.19 | 0.97 | 0.92–1.02 |
| Smoking status | 0.308 | 1.71 | 0.19 | 1.36 | 0.86–2.16 |
| Type of CR referral | 0.743 | 10.68 | < 0.01 | 2.10 | 1.35–3.28 |
| Β: beta weight; Wald: test statistic; p: significance value; OR: odds ratio; CI: confidence interval. |
DISCUSSION
There is substantial evidence regarding the benefits of CR (4, 5, 22), thus the gross under-utilization of these services (6, 7, 23) is disconcerting. Few studies have examined interventions to increase referral (24), yet automated referral mechanisms show promise (15–17). Results of this prospective controlled study suggest that automatic referral results in significantly greater referral and enrollment in CR, when compared with usual referral at the discretion of the physician. In fact, after controlling for clinical and sociodemographic characteristics, automatic referral resulted in over 2 times greater enrollment than usual referral mechanisms, with over 50% of patients enrolling in these evidence-based programs. The Cardiac Care Network of Ontario recommended a target of 40% CR enrollment (25), a conservative estimate taking into consideration morbidity and mortality, and patient interest, preference, and adherence. Automatic referral can surpass this goal. Given the mortality and morbidity benefits of CR participation, such a health-system-based intervention has the potential to maximize secondary prevention.
Results also point to earlier referral through automated mechanisms, such that participants are more likely to be referred in the inpatient unit prior to discharge rather than at a follow-up physician visit. In fact, CR referral was received in less than half the time following automatic vs usual referral, with a mean of less than one month vs more than 2 months wait, respectively. While this does not reflect the actual intake date into CR, this nevertheless has important ramifications for reducing CR utilization delays and ultimately cardiovascular risk.
Of interest were the findings that verified enrollment also varied based on indication and family income. Given that we controlled for disease severity in our model and found no enrollment differences based on either NYHA class or Duke activity status, this suggests that there may be variability in referral norms or practices on different inpatient wards. It could also suggest that patients with PCI themselves do not perceive that their condition warrants CR when compared with those hospitalized for an MI, UA and/or ACB (26–28). Secondly, even under universal healthcare where there are no costs to enroll in CR (except minimal indirect transportation or parking costs), it is nevertheless less accessible to low income patients with cardiac diseases. The literature shows that those of low socioeconomic status tend to engage in fewer health-promoting behaviors and also have worse prognosis (29–31). Clearly, we need further tailored interventions to increase CR enrollment among cardiac patients of lower socioeconomic status.
Within the context of automatic referral, barriers to CR participation continue to exist. Even where automatically referred, almost 50% of participants chose not to enroll in the program, regardless of disease severity, sex and age. Healthcare provider encouragement to enroll may provide the personalized impetus to attend (8, 32). We must also look to the literature on patient barriers to participation (13) to address these further care gaps. In addition, evidence regarding the acceptability and preferences for home-based CR programs (33) may even further improve the reach of cardiovascular secondary preventive services.
Caution is warranted when interpreting these findings due to self-report and selection biases, and design issues. The self- and CR program-reported enrollment rates were highly concordant around 42%, but self-report of CR referral, enrollment and participation were often discordant. For example, some participants reported participation but no referral, or did not respond to each item. This lead to questions regarding social desirability biases in participant responses. However, by verifying receipt of referrals, enrollment and participation data, we have overcome this limitation. Still, verified enrollment rates in the usual referral condition were higher than what has been reported in the region more generally (15–20% (6, 25)). While our study was presented as investigating cardiac health services generally, the Hawthorne effect may be at play.
Second, our inception cohort of participants was more likely to be male and younger than patients with cardiac diseases in general. While participants at both sites were shown to be equivalent on multiple parameters, they differed with regard to their index condition. The sample of retained participants had better prognostic characteristics (i.e. younger age, lower BMI, less likely to smoke) than those who refused or were ineligible at the 9-month assessment. However, these variables were controlled for in our model. Finally, while both sites offered advanced cardiac services, one was a teaching and the other a community hospital, leading to questions about the appropriateness of our control condition.
This relates to our third limitation of design. For ethical reasons, participants could not be randomized to acute care site, but go to the nearest hospital for timely cardiac care (34). Moreover, for contamination purposes we could not randomize type of referral within site. These issues leave unanswered questions with regard to site-specific factors, other than the referral mechanism, which may have affected the CR process. Future research is needed with a randomized design or multiple sites within each referral condition to address these limitations. Directions for future research also include identifying automatic referral operationalizations at different acute care sites (e.g. pre-authorization of physician signature for referral (35)), and comparing enrollment rates following referral using electronic prompts vs these other systematized referral mechanisms. Continued efforts towards ensuring access to CR services are imperative given the burden of cardiovascular disease (1).
In summary, this presents the first prospective, controlled, multi-center study examining the effect of automatic vs usual referral on verified CR enrollment. Results show that automatic referral indeed increases overall CR utilization by more than 2 times. Automatic referral as operationalized here also results in significantly reduced referral times. Given the significant benefits of CR, the policy implications of automatic referral deserve attention. The extensive implementation of electronic health records broadens the potential reach of such referral processes.
ACKNOWLEDGEMENTS
This study was funded by Canadian Health Services Research Foundation and Ontario Ministry of Health and Long-Term Care, and administered by the Canadian Institutes of Health Research FRN# 73996. Dr Grace is supported by the Ontario Ministry of Health and Long-Term Care. We gratefully acknowledge the efforts of Laura Ewart and Suzan Krepostman in participant recruitment, and the nurses on the wards who facilitated this process
REFERENCES
1. Organization for Economic Cooperation and Development. International mortality data 2001. CACR, Winnipeg, MB, Canada.
2. Law MR, Watt HC, Wald NJ. The underlying risk of death after myocardial infarction in the absence of treatment. Arch Intern Med 2002; 162: 2405–2410.
3. Kannel WB, Sorlie P, McNamara PM. Prognosis after initial myocardial infarction: the Framingham study. Am J Cardiol 1979; 44: 53–59.
4. Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2004; 1: CD001800.
5. Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med 2004; 116: 682–692.
6. Grace SL, Abbey SE, Shnek ZM, Irvine J, Franche RL, Stewart DE. Cardiac rehabilitation II: referral and participation. Gen Hosp Psychiatry 2002; 24: 127–134.
7. Bunker SJ, Goble AJ. Cardiac rehabilitation: under-referral and underutilization. Med J Aust 2003; 179: 332–333.
8. Ades PA, Waldmann ML, Polk DM, Coflesky JT. Referral patterns and exercise response in the rehabilitation of female coronary patients aged greater than or equal to 62 years. Am J Cardiol 1992; 69: 1422–1425.
9. Grace SL, Evindar A, Abramson BL, Stewart DE. Physician management preferences for cardiac patients: factors affecting referral to cardiac rehabilitation. Can J Cardiol 2004; 20: 1101–1107.
10. Grace SL, Krepostman S, Abramson BL, Scholey P, Brooks D, Jaglal S, et al. Referral to and discharge from cardiac rehabilitation: key informant views on continuity of care. J Eval Clin Pract 2006; 12: 155–163.
11. Johnson JE, Weinert C, Richardson JK. Rural residents’ use of cardiac rehabilitation programs. Public Health Nurs 1998; 15: 288–296.
12. King KM, Teo KK. Cardiac rehabilitation referral and attendance: not one and the same. Rehabil Nurs 1998; 23: 246–251.
13. Daly J, Sindone AP, Thompson DR, Hancock K, Chang E, Davidson P. Barriers to participation in and adherence to cardiac rehabilitation programs: a critical literature review. Prog Cardiovasc Nurs 2002; 17: 8–17.
14. Stone JA, editor. Canadian guidelines for cardiac rehabilitation and cardiovascular disease prevention: enhancing the science, refining the art. CACR, Winnipeg, MB, Canada; 2004.
15. Grace SL, Evindar A, Kung T, Scholey P, Stewart DE. Increasing access to cardiac rehabilitation: automatic referral to the program nearest home. J Cardiopulm Rehabil 2004; 24: 171–174.
16. Grace SL, Evindar A, Kung TN, Scholey PE, Stewart DE. Automatic referral to cardiac rehabilitation. Med Care 2004; 42: 661–669.
17. Smith KM, Harkness K, Arthur HM. Predicting cardiac rehabilitation enrolment: the role of automatic physician referral. Eur J Cardiovasc Prev Rehabil 2006; 13: 60–66.
18. American Association of Cardiovascular & Pulmonary Rehabilitation. Guidelines for cardiac rehabilitation and secondary prevention programs: promoting health & preventing disease. 3rd edn. Champaign, Ill: Human Kinetics; 1999.
19. The Criteria Committee of the New York Heart Association editor. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. Boston: Little, Brown & Co.; 1994.
20. Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index). Am J Cardiol 1989; 64: 651–654.
21. Nelson CL, Herndon JE, Mark DB, Pryor DB, Califf RM, Hlatky MA. Relation of clinical and angiographic factors to functional capacity as measured by the Duke Activity Status Index. Am J Cardiol 1991; 68: 973–975.
22. Brown A, Taylor R, Noorani H, Stone J, Skidmore B. Exercise-based cardiac rehabilitation programs for coronary artery disease: a systematic clinical and economic review. Technology Report no. 34. Ottawa, ON: Canadian Coordinating Office for Health Technology Assessment; 2003.
23. Bittner V, Sanderson B, Breland J, Green D. Referral patterns to a University-based cardiac rehabilitation program. Am J Cardiol 1999; 83: 252–255.
24. Beswick AD, Rees K, West RR, Taylor FC, Burke M, Griebsch I, et al. Improving uptake and adherence in cardiac rehabilitation: literature review. J Adv Nurs 2005; 49: 538–555.
25. Cardiac Care Network. The Ontario cardiac rehabilitation pilot project: report and recommendations. Toronto, ON, 2002. Available from: http://www.ccn.on.ca/pdfs/Rehab-pilot-project-sep2002.pdf.
26. French DP, Lewin RJP, Watson N, Thompson DR. Do illness perceptions predict attendance at cardiac rehabilitation and quality of life following myocardial infarction? J Psychosom Res 2005; 59: 315–322.
27. Whitmarsh A, Koutantji M, Sidell K. Illness perceptions, mood and coping in predicting attendance at cardiac rehabilitation. Br J Health Psychol 2003; 8: 209–221.
28. Petrie KJ, Weinman J, Sharpe N, Buckley J. Role of patients’ view of their illness in predicting return to work and functioning after myocardial infarction: longitudinal study. BMJ 1996; 312: 1191–1194.
29. Alter DA, Naylor CD, Austin P, Tu JV. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N Engl J Med 1999; 341: 1359–1367.
30. Salomaa V, Niemela M, Miettinen H, Ketonen M, Immonen-Raiha P, Koskinen S, et al. Relationship of socioeconomic status to the incidence and prehospital, 28-day, and 1-year mortality rates of acute coronary events in the FINMONICA myocardial infarction register study. Circulation 2000; 101: 1913–1918.
31. Morrison C, Woodward M, Leslie W, Tunstall-Pedoe H. Effect of socioeconomic group on incidence of, management of, and survival after myocardial infarction and coronary death: analysis of community coronary event register. BMJ 1997; 314: 541–546.
32. Mitoff PR, Wesolowski M, Abramson BL, Grace SL. Patient- provider communication regarding referral to cardiac rehabilitation. Rehabil Nurs 2005; 30: 140–146.
33. Grace SL, McDonald J, Fishman D, Caruso V. Patient preferences for home-based versus hospital-based cardiac rehabilitation. J Cardiopulm Rehabil 2005; 25: 24–29.
34. Van de Werf F, Gore JM, Avezum A, Gulba DC, Goodman SG, Budaj A, et al. Access to catheterization facilities in patients admitted with acute coronary syndrome: multinational registry study. BMJ 2005; 330: 441.
35. Krepostman S, Scholey P, Stewart DE, Grace, SL. A qualitative pilot study examining automatic referral mechanisms to cardiac rehabilitation. University Health Network Research Day, Toronto, ON, 2005.