Jacek Flicinski1, Marek Brzosko1 and Slawomir Olewniczak2
Departments of 1Rheumatology and 2Pathology, Pomeranian Medical University, Unii Lubelskiej 1, PL-71-252 Szczecin, Poland. E-mail: jacekfl@sci.pam.szczecin.pl
Accepted January 17, 2006.
Sir,
Cyclosporine (CS) is a widely used immunosuppressive drug. Its administration is related to multiple side- effects, most often gastrointestinal, renal impairment, hypertrichosis and hypertension (1). It can also contribute to neoplastic diseases of the skin (2, 3). Only one case of multiple angiomas related to CS has been reported in the literature (4). We describe here a 35-year-old man with psoriatic arthritis who developed haemangiomas on his upper and lower extremities in the course of CS treatment.
CASE Report
A 35-year-old man developed psoriatic arthritis 2 years after the onset of psoriasis. He was primarily treated with sulphasalazine, 1.0 g twice daily. After a flare-up of arthritis sulphasalazine was replaced with methotrexate, 17.5 mg weekly, and methylprednisolone, 5 mg daily. Due to insufficient response, CS was added in gradually increasing doses starting from 2.5mg/kg daily up to 4.0 mg/kg daily when remission of arthritis was achieved and this dose was used as the maintenance dose. During the treatment the patient developed gingival hyperplasia, which resolved after CS dose reduction to 3 mg/kg daily.
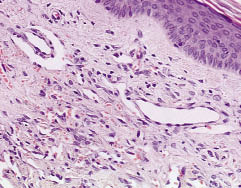
Three years after starting the treatment with CS the patient reported appearance of 2 nodules elevated above the surface of the skin, purple, hard and painless, 5 mm in diameter (Fig. 1). One was localized on his left forearm and the other on the right thigh. The former was surgically removed. Histological examination revealed a vascular lesion without any features of malignancy, consistent of haemangioma (Fig. 2). During the following 2 months another 8 new nodules (5 mm in diameter on average) appeared on the lower and upper extremities, sparing the head and the trunk. The one that was present previously grew to 8 mm. As the appearance of the lesions was supposed to be related to CS, this dose was reduced. It did not affect the growth of the lesion, and CS was finally discontinued. The exacerbation of arthritis was thereafter managed by increasing the dose of methylprednisolone and methotrexate. Within the following 3 months, only one new nodule appeared and the ones previously present did not grow. During the following 4 months the nodules got smaller and finally disappeared, leaving small depigmentation areas. In the meantime chest and abdominal imaging studies were performed showing no pathologies. Complete blood count, urinalysis, aminotransferases, creatinine and erythrocyte sedimentation rate were normal during the follow-up period. Since then the nodules have never reappeared and the patient has been well for over 2 years. He is currently treated with methotrexate, 15 mg weekly and methylprednisolone, 4 mg daily.

Fig. 1. Single nodule on the lateral aspect of the right thigh.
Fig. 2. Numerous blood vessels in the dermis, beneath the epidermis (haematoxylin and eosin, ×200)
DISCUSSION
CS has no mutagenic effect; however, due to its immunosuppressive effect it may allow the growth of neoplastic cells (5). There are studies proving that CS has a significant influence on occurrence of skin malignancies (2, 3). Only one study has countered this (6). CS is known to cause non-malignant dermatological and mucosal side-effects, such as hypertrichosis, sebaceous hyperplasia and gingival hyperplasia (1, 7).
The case reported here presents a benign neoplasia, nodular haemangioma, in a patient treated for psoriatic arthritis with CS and methotrexate. It is possible that both drugs contributed to their formation (2). However, the fact that the haemangiomas started to regress and finally cleared after cessation of CS therapy suggests a probable role of CS in their pathogenesis.
Only one case of multiple angiomas in a patient with psoriasis treated with CS has been reported in the literature (4). In our case the haemangiomas were much bigger and they cleared after CS had been stopped, while in the other case all of them remained unchanged. A common feature of these two cases is their localization, limited only to the extremities. The time from starting the CS therapy to occurrence of haemangiomas (several months) and the doses of CS were also similar. Both cases were free of any coexisting pathologies and all the blood tests were normal.
It seems that the haemangiomas of the patient described here were related to hyperplasia of endothelial cells. This supports the previously presented thesis that CS can induce hyperplasia of different cells present in the skin, resulting in a wide range of dermatological and mucosal pathologies (4).
Careful skin monitoring of patients treated with CS is essential. Discontinuation of CS may cause complete regression of related side-effects to this therapy – skin haemangiomas.
References
1. Dijkmans B, Gerards A. Cyclosporin in rheumatoid arthritis: monitoring for adverse effects and clinically significant drug interactions. BioDrugs 1998; 10: 437–445.
2. Paul CF, Ho VC, McGeown C, Christophers E, Schmidtmann B, Guillaume JC, et al. Risk of malignancies in psoriasis patients treated with cyclosporine: a 5 year cohort study. J Invest Dermatol 2003; 120: 211–216.
3. Arellamo F, Krupp P. Malignancies in rheumatoid arthritis treated with cyclosporin A. Br J Rheumatol 1993; 32 (suppl. 1): 72–75.
4. De Felipe I, Redondo P. Eruptive angiomas after treatment with cyclosporine in a patient with psoriasis. Arch Dermatol 1998; 134: 1487–1488.
5. Ryffel B, Mihatsch MJ, Fisher GL. Immunosuppression and cancer: the cyclosporin case. Drug Chem Toxicol 1992; 15: 95–115.
6. van den Borne BEEN, Landewe RBM, Houkes I, Schild F, van der Heyden PC, Hazes JM, et al.  No increased risk of malignancies and mortality in cyclosporin A-treated patients with rheumatoid arthritis. Arthritis Rheum 1998; 41: 1930–1937.
No increased risk of malignancies and mortality in cyclosporin A-treated patients with rheumatoid arthritis. Arthritis Rheum 1998; 41: 1930–1937.
7. Valicenti JM, Pakula A, Caro WA, Malkinson FD. Papilloma development in cyclosporine-treated patients. Arch Dermatol 1993; 129: 794–795.
