Shown Tokoro, Takahiro Satoh, Yoshiko Okubo, Ken Igawa and Hiroo Yokozeki
Department of Dermatology, Graduate School, Tokyo Medical and Dental University, Tokyo, Japan
Shown Tokoro, Takahiro Satoh, Yoshiko Okubo, Ken Igawa and Hiroo Yokozeki
Department of Dermatology, Graduate School, Tokyo Medical and Dental University, Tokyo, Japan
Dystrophic calcification in the skin occurs in association with a variety of disorders. To determine the association between subcutaneous calcification and chronic venous insufficiency, X-ray examinations were performed in 20 patients with chronic venous insufficiency and in 20 control subjects to detect latent calcification in their lower legs. Of the 20 patients, 13 (65%) had subcutaneous calcification, and the prevalence appeared to increase with disease duration, while only 4 control subjects (20%) had minimal calcification. Two types of calcification were identified based on their radiographic features: punctate and trabecular/reticular types. Patients with trabecular/reticular calcification had longer disease duration and more severe clinical scores than patients with punctate calcification. None of the control subjects had trabecular/reticular types of calcification. The identification of the presence and progression of latent calcification in the lower legs is useful, and may be necessary for the long-term management of chronic venous insufficiency, since calcification of skin tissues impedes wound healing and can be a risk factor for refractory ulcers. Key words: calcification; CEAP score; chronic venous insufficiency; ulcer.
(Accepted April 6, 2009.)
Acta Derm Venereol 2009; 89: 505–508.
Takahiro Satoh, Department of Dermatology, Graduate School, Tokyo Medical and Dental University, 1-5-45 Yushima, Bunkyo-ku, 113-8519, Japan. E-mail: tasa-1688.derm@tmd.ac.jp
Dystrophic calcinosis is the aberrant deposition of calcium salt in the skin of patients who do not have a systemic dysfunction of calcium metabolism. Local tissue damage, such as degeneration of collagen fibres, elastic fibres, fat cell necrosis caused by trauma, infections, neoplasms, and many other conditions, are considered to be precipitating factors (1). Chronic venous insufficiency (CVI) has also been suggested as a factor that promotes the deposition of calcium phosphate in the tissues (2–6).
CVI presents with various cutaneous symptoms, such as oedema, pigmentation, and lipodermatosclerosis. Ulcerations make the management of CVI difficult. Prior studies have suggested that calcified deposits in the skin impede wound healing and cause refractory ulceration of the lower legs (6–9). However, unless calcified nodules extrude from ulcers, subcutaneous calcification may easily be overlooked. Thus, it is important to identify latent calcinosis during the management of CVI. A case of a patient with numerous calcified nodules that extruded from refractory leg ulcers encouraged us to examine the incidence of latent calcification in CVI and its relationship to disease duration and clinical severity. The aims of the present study were to detect subcutaneous calcification of the lower legs by X-ray examination and/or skin biopsy, and to examine the patterns of calcification among patients with different clinical profiles.
Materials and Methods
Patients
Twenty patients with CVI (8 men, 12 women; mean age 66.6 years) who visited our dermatology and/or vascular surgery department complaining of skin changes in the lower legs were examined. Underlying diseases included rheumatoid arthritis (2 cases) and type II diabetes mellitus (2 cases).
Clinical evaluation
Diagnosis of CVI was based on the characteristic clinical manifestations and ultrasound features of the superficial and deep veins, such as luminal thrombus, vein reflux with valve insufficiency, incompetent perforating veins, and dilatation of superficial veins. The classification of clinical manifestations associated with CVI was based on the objective scoring system of C criteria in the CEAP (Clinical-Etiology-Anatomy-Pathophysiology) classification (10, 11) as follows:
Detection of subcutaneous calcification
X-ray examinations of the lower legs were performed in all patients.
X-ray films of 20 age-matched control subjects who underwent X-ray examination for diseases such as osteoarthrosis of the knee joints (n = 17) and accidental trauma (n = 3) (9 men, 11 women; mean age 67.3 years) treated at the orthopaedic surgery department in our institute were also examined retrospectively.
Statistical analyses
The Mann-Whitney U test was used to assess the statistical significance of differences between mean values. p-values less than 0.05 were considered statistically significant.
Results
The median age of patients with CVI was 70 years, and their median disease duration was 6 years. These patients’ overall clinical severity class was 5.1 ± 1.21, with 1 C2 patient, 7 C4 patients, and 12 C6 patients (Fig. 1A). The 20 patients’ profiles are summarized in Table I according to the presence of calcification. Of the 20 patients, 13 (65%) had subcutaneous calcification on X-ray examination of the lower legs. In contrast, calcification was found in 4 of 20 control subjects (20%). The patients with CVI with calcification had longer disease duration than those without calcification. Skin biopsy specimens were obtained from 5 patients. Ossified small nodules and/or nodular/granular basophilic calcium deposits were found in the deep dermis and subcutaneous tissues with fibrotic changes (Fig. 1B). None of the specimens had calcification on the vascular walls. None of the patients had increased serum calcium, phosphate, or parathyroid hormone levels. Fig. 1C shows the most severe case (C6), in which a number of large ossified nodules extruded from the bases of ulcers.

Fig. 1. Clinical manifestations of chronic venous insufficiency. (A) Representative features of patients with Clinical-Etiology-Anatomy-Pathophysiology (CEAP) classes 2, 4, and 6, respectively. (B) Representative pictures of biopsy specimens. Left: ossified nodules. Right: Nodular (arrow) and granular (arrow heads) basophilic calcium deposits (haematoxlyin and eosin (H&E) ×400). (C) The most severe case (C6), in which a number of large calcified nodules can be seen to extrude from the ulcers.
Table I. Profiles of patients with chronic venous insufficiency
| X-ray findings | Number of cases (male/female) | Median age (years) (IQR) | Clinical severity (CEAP class) Mean ± SD | Median disease duration (years) (IQR) |
| Calcification (+) | 13 (6/7) | 77 (23) | 5.5 ± 0.9 | 7a (20) |
| Calcification (–) | 7 (2/5) | 67 (17) | 4.3 ± 1.4 | 2 (7) |
ap < 0.05 (Mann-Whitney U test).
IQR: interquartile range; SD: standard deviation; CEAP: Clinical-Etiology-Anatomy-Pathophysiology.
The prevalence of calcification generally appeared to increase with disease duration (Fig. 2A). Based on their radiographic features, several patterns of calcification were identified: punctate (n = 9), trabecular (n = 1), and reticular types (n = 3) (Fig. 3). The trabecular/reticular types were more common in patients with longer disease duration than the punctate type (p < 0.05) (Fig. 2B) and in patients with a clinical score of C6 (Fig. 4). The calcification pattern found in four control subjects was the punctate type.
Fig. 2. (A) Prevalence and (B) patterns of calcification by disease duration.
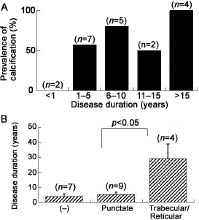
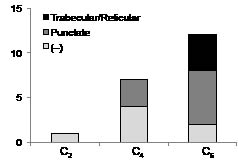
Fig. 4. Correlation of calcification patterns and clinical severity class (Clinical-Etiology-Anatomy-Pathophysiology: CEAP).
Discussion
In the present study, a high prevalence of latent dystrophic calcification of the lower legs was found among 20 patients with CVI. The calcification did not involve the venous walls, as assessed by the features on ultrasound (data not shown) and the histological examinations performed in some patients, which is consistent with a previous report (3).

Fig. 3. Radiographic features of subcutaneous calcification.
The incidence of calcification appeared to be correlated with disease duration and clinical severity. In general, two patterns of calcification were observed on X-ray examination: punctate and trabecular/reticular types. The calcification probably started with the punctate type and then progressed to the trabecular/reticulate type, since the trabecular/reticular type was found mostly in patients with long disease duration and/or with a high clinical severity class (Figs 2B and 4).
The prevalence of latent dystrophic calcification in CVI in this study was higher (65%) than generally thought; approximately 10% of CVI patients were reported to have dystrophic calcification in an earlier, extensive review (3). In addition, four control subjects (20%) had minimal punctate-type calcification, although the presence of CVI could not be completely ruled out in the control subjects. The high prevalence of calcification in the present study might be due to the small sample sizes. In addition, more than half of the patients (12 patients, 60%) examined were classified as the most severe type of CVI by clinical class (C6). Further study with a larger series of patients with varying clinical severities together with healthy controls is needed.
The pathogenesis of dystrophic calcification in venous insufficiency is obscure, but it may result either from venous leakage caused by stasis and/or persistent inflammation, leading to phosphate binding to denatured proteins, or from a dysregulation of intracellular Ca2+ concentration of mitochondria in dying cells (7, 8).
Therapies for dystrophic calcinosis have not been well established. Surgical debridement of calcified masses would be the most effective treatment (4, 6). A recent report demonstrated successful conservative treatment with topical sodium thiosulphate, which chelates calcium into calcium thiosulphate salts, which are more soluble than calcium phosphate (8). Systemic administration of disodium etidronate may inhibit the progression of dystrophic calcification (12).
Dystrophic calcification could be a risk factor for the failure of leg ulcer treatment in CVI patients. Calcium deposits impair normal epithelial growth and cause persistent inflammation with a foreign body reaction, resulting in delayed wound healing (6–9). Formation of calcified and/or ossified nodules probably leads to a high recurrence rate of leg ulcers, which, in turn, increases the risk of further calcium salt deposition. The identification of latent calcification and the course of its progression in the lower legs by periodic X-ray examination is important for the long-term management of patients with CVI, particularly those with treatment-resistant leg ulcers, since the removal of calcium deposits underneath and/or around ulcers is necessary. Furthermore, early detection of latent calcinosis would be useful if a potent and prophylactic therapy capable of inhibiting the progression of calcinosis could be provided
The authors declare no conflict of interest.
REFERENCES
