Amy M. Dennett, BPhty(Hons) and Nicholas F. Taylor, PhD
From the Faculty of Health Sciences, La Trobe University and Allied Health Clinical Research Office, Eastern Health, Victoria, Australia
OBJECTIVE: To determine the effectiveness of computer-based electronic devices that provide feedback in improving mobility and balance and reducing falls.
DATA SOURCES: Randomized controlled trials were searched from the earliest available date to August 2013.
DATA EXTRACTION: Standardized mean differences were used to complete meta-analyses, with statistical heterogeneity being described with the I-squared statistic. The GRADE approach was used to summarize the level of evidence for each completed meta-analysis. Risk of bias for individual trials was assessed with the (Physiotherapy Evidence Database) PEDro scale.
DATA SYNTHESIS: Thirty trials were included. There was high-quality evidence that computerized devices can improve dynamic balance in people with a neurological condition compared with no therapy. There was low-to-moderate-quality evidence that computerized devices have no significant effect on mobility, falls efficacy and falls risk in community-dwelling older adults, and people with a neurological condition compared with physiotherapy.
CONCLUSION: There is high-quality evidence that computerized devices that provide feedback may be useful in improving balance in people with neurological conditions compared with no therapy, but there is a lack of evidence supporting more meaningful changes in mobility and falls risk.
Key words: falls; balance; mobility; virtual-reality; meta-analysis.
J Rehabil Med 2014; 46: 00–00
Guarantor’s address: Amy Dennett, Department of Physiotherapy, Peter James Centre, Cnr. Mahoneys Road & Burwood Highway, Burwood East Victoria, 3151, Australia. E-mail: Amy.Dennett@easternhealth.org.au
Accepted Jul 7, 2014; Epub ahead of print Oct 7, 2014
Introduction
Falls are a major issue affecting older people, with one-third of people aged 65 years and over falling at least once each year (1). This has significant implications for the individual in terms of injury, reduced mobility and independence at home and in the community. The impact of falls also has a significant cost for health services, with the annual cost of falls-related injury in Australia expected to rise almost 3-fold to AUD 1.4 billion by 2051 (2).
Poor balance is an important risk factor for falls (3–5). Exercise programmes are often prescribed to improve balance, with the aim of reducing falls. Indeed, it has been shown that up to 42% of falls in older people living in the community can be prevented by well-designed exercise programmes that provide a moderate-to-high challenge to balance, that are undertaken for at least 2 hours per week (6, 7). These exercise programmes may be undertaken within a home or clinical setting (7, 8).
The use of technology through interactive gaming and virtual-reality is becoming increasingly popular with clinicians to create stimulating and challenging environments to improve balance and mobility within therapy sessions. The Nintendo Wii alone has been adapted for rehabilitation across health settings in many countries, with reports of 61% of urban stroke rehabilitation centres owning a console in Australia (9, 10). The advantage of such gaming and other virtual-reality systems is that they provide visual or other forms of feedback through a screen or a head-mounted device, which allows the user to interact with virtual environments to simulate balance and functional tasks at intensities that may be greater than traditional therapies (11–13). This may be important, given that visual and proprioceptive feedback are important components of balance control (14, 15). It is also thought that this technology may be more engaging and fun for patients as they can interact with programmes and may be less likely to focus on their health condition. In turn, this may assist with improved adherence to such therapy programmes.
Current evidence has demonstrated positive effects of virtual-reality rehabilitation in people with upper limb impairments post stroke (16, 17). Less is known about the effectiveness of computer-based technology in other populations due to lack of quality randomized controlled trials (8, 10, 18). To date, there has been no systematic reviews that we are aware of that have synthesized the available evidence on the effectiveness of computer-based interventions in terms of balance and mobility outcomes during rehabilitation.
The purpose of this systematic review was therefore to determine whether the use of computer-based technology that provides feedback is effective in improving balance, and whether any benefits carry over into improved mobility or reduced risk of falls.
Methods
Research design
A systematic review was completed in accordance with PRISMA guidelines (19, 20) and was registered prospectively through PROSPERO (CRD42013005726) (21).
Trials to be included in the review were identified though electronic database searching from the earliest available time until August 2013 through the following databases: MEDLINE, EMBASE and CINAHL. The search strategy used was based around synonyms and MeSH subject headings of the key concepts of: first, electronic devices and computer technology; secondly, balance; and thirdly, rehabilitation, combined with Boolean operators OR within each concept and the operator AND between the concepts (Appendix I). These terms were combined with the relevant filters (22) to identify randomized controlled trials and controlled trials. Studies from the EMBASE database were further limited by date (1990 to present) given the nature of the technology being studied. The search was supplemented by citation tracking and checking the reference lists of included studies.
Inclusion criteria
Title and abstracts of identified trials were assessed by 2 reviewers independently using predetermined inclusion and exclusion criteria (Table I). Full text articles were obtained and examined by both reviewers where inclusion could not clearly be determined by title and abstract alone. To be included in the review, trials were to use computer technology that provided feedback as a therapy tool such that any change could be attributed to the technology. Any device that was assistive or instructive was not included, as the investigation of the use of electronic feedback to improve balance was the primary aim of the current review.
|
Table I. Inclusion/exclusion criteria |
|
|
Inclusion criteria |
Exclusion criteria |
|
• Adults i.e. mean age ≥ 18 years old. • Randomized controlled trials. • Peer-reviewed journal article. • Written in English. • Use of computer technology or other electronic device that provides immediate and interactive visual, auditory or proprioceptive feedback as a therapy tool used for the purpose of improving balance or mobility. Includes virtual-reality and computer simulation. • Computer technology or electronic device should be used as the primary intervention. However, warm-up and cool-down exercises allowed if they do not take up more than 20% of intervention time and client may complete a supplementary home exercise program (HEP). • Use of at least one balance-, mobility- or falls-related outcome measure. |
• Other research designs including: systematic reviews, case studies, opinion articles, editorials, book chapters, clinical guidelines, single group pre-post studies, controlled trials, abstracts, qualitative data. • Computer technology or electronic device that is used as an assessment tool, electronic medical records, tele/video-conferencing, electrical stimulation, computer devices or applications that only provide instructions (e.g. App that provides HEP) or device does not primarily provide direct feedback during balance activities or is assistive, e.g. robots, treadmills, vibration platforms. These devices may only be used if linked with an electronic device that does provide immediate feedback. • Technology intervention used as part of a co-intervention, e.g. combined with “conventional physiotherapy”. • Only uses traditional physiotherapy modalities or equipment that is not computerized or provides electronic feedback, e.g. use of rocker-boards/wobble-board, foam mats, duradisks/bosu ball, balance beam, hydrotherapy, tai chi, etc. • Does not use balance, falls or mobility related outcomes. |
Risk of bias assessment
Risk of bias of the included trials was assessed independently by 2 reviewers using the (Physiotherapy Evidence Database) PEDro scale. The 11 items on the PEDro scale are rated “yes” or “no”, with a maximum score of 10 achieved for internal validity as the first item is not rated. The PEDro scale is a valid measure of methodological quality of clinical trials that has undergone Rasch analysis and has moderate levels of inter-rater reliability (ICC 0.68, 95% CI 0.57, 0.76) (23, 24). Trials were deemed high quality if scores were 6 or above. Trials that scored 4 or less were deemed lesser quality (25).
Data analysis
Meta-analyses were completed using a random effects model for clinically homogeneous data using standardized mean differences for continuous data. Statistical heterogeneity was described with the I-squared statistic. Descriptive analysis was completed for data that could not be analysed with meta-analyses. Data included in the analysis were evaluated according to the population studied and comparing the intervention with no therapy or traditional physiotherapy interventions.
The GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach (26) was used to summarize the level of evidence for each completed meta-analysis. This approach involves downgrading the evidence from high to moderate to low to very low. Downgrading of the evidence would occur based on the following criteria: (1) the PEDro score was < 6 for the majority of trials in the meta-analysis, (2) there was greater than low levels of statistical heterogeneity between the trials (I2 > 25%), and (3) there were large confidence intervals. A 95% confidence interval of > 0.8 in the standardized mean difference of the meta-analysis was regarded as large, since this value could span the difference between an intervention having no effect and a large effect according to Cohen’s criteria (27). If there were serious issues with the methodological quality, such as all trials in the meta-analysis were < 6 PEDro score without allocation concealment and blinded assessors, then a double downgrade would occur (e.g. from high to low quality). Reasons for the grade applied to each meta-analysis were explained using footnotes.
Results
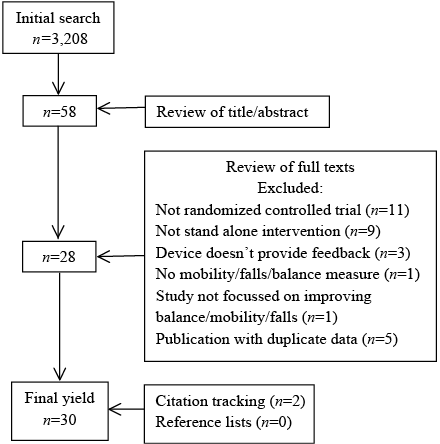
The search of electronic databases resulted in a yield of 3,208 articles, which was reduced to 58 after application of inclusion/exclusion criteria to title and abstracts. After further assessment of full-text articles, this was reduced to 28 trials. No further trials were identified from review of the reference lists of the already included studies. Two relevant trials were identified using citation tracking, resulting in a final library of 30 trials to be included for review (Fig. 1).
Risk of bias
All of the articles included in this review were randomized controlled trials. The median score of the included articles was 5 out of 10 (mean 5.2, range 3–8, mode = 6) on the PEDro scale (Table II). Only one study (28) scored 8 on the scale, which is the highest possible score, given the nature of the intervention being studied, where it would not be expected to be feasible to blind patients or clinicians. The criterion for random allocation of participants was the only criterion met by all of the included trials. Fifteen trials reported assessor blinding (28–41). Concealment of treatment allocation occurred in only 5 trials (28, 35, 37, 39, 40) and intention to treat analyses was completed in 7 trials (28, 30, 33, 41–44).
Summary of data
The results of a total of 1240 people were included in the review. The majority of participants were women (60%) with a mean age of 61 years (SD 19 years). The main health conditions represented by participants included: acquired brain injury (6 trials (30–34, 40), multiple sclerosis (3 trials (29, 35, 36)), acute and chronic peripheral vestibular dysfunction (3 trials (42, 45, 46)), Parkinson’s disease (2 trials (41, 47)), and type 2 diabetes in 1 trial (48). Three trials investigated a healthy young adult population (49–51) and 11 trials investigated community-dwelling older adults (37–39, 43, 44, 52–57).
Interventions
All trials included in the review used computer-based technology to improve balance or mobility using electronic feedback. The most popular device was the Nintendo Wii, which was used in 15 trials (28–30, 35, 36, 38, 43, 44, 46, 49, 51–53, 55, 56). Other commercial video-game based devices were used in 4 trials (30, 37, 48, 49). Nine trials used customized electronic balance devices, where games could be individually tailored by the therapists (31, 39, 41, 42, 45, 47, 50, 54, 57). Two trials used virtual-reality based treadmill training (32, 40) and 2 trials used virtual-reality based robot training (33, 34). Most interventions were conducted in an outpatient clinic or laboratory setting, with two trials using a home-based setting (36, 37) and one completed in an acute hospital (28). The duration of each intervention varied from 10–60 min. Typically, sessions were completed 2–3 times per week for, on average, 6 weeks (range 1–20 weeks). The computerized intervention was compared with conventional physiotherapy interventions (termed physiotherapy for the purpose of this review) in 17 trials (28, 29, 31, 38, 39, 41, 44, 45, 47, 49–56). Physiotherapy interventions included traditional balance, seated exercise and home exercise programmes, which included functional mobility, static and dynamic balance, strength and flexibility exercises. Two studies included ocular mobility and optokinetic stimulation as part of the physiotherapy intervention (45, 46). Two trials compared the intervention with tai chi (55, 57). Two trials compared treadmill training with and without virtual-reality (32, 40) and 2 trials compared a robotic ankle device with and without virtual-reality (33, 34). Thirteen trials had a control group with no exercise intervention (30, 35–37, 41–44, 46, 48, 52, 54, 57) (Table II). However, 2 of these trials received education (48, 57).
|
Table II. Characteristics of included trials |
||||||||
|
Study PEDro Score (/10) |
Subjects, n Females, % Age, mean (SD) |
Health condition |
Intervention |
Comparison |
Dosage |
Setting |
Outcome measures |
|
|
Brumels et al., 2008 (49) 3 |
25 52% 19.6 (1.7) |
Healthy young adults |
Dance Dance Revolution Nintendo Wii Fit |
Traditional balance programme |
12–15 min 3 × /week 4 weeks |
Laboratory |
Static balance Dynamic balance |
Single leg postural sway using force plate SEBT |
|
Brichetto et al., 2013 (29) 6 |
36 61% 42 (11) |
Multiple sclerosis |
Nintendo Wii Fit |
Traditional balance programme |
60 min 3 × /week 4 weeks |
Outpatient clinic |
Static Balance Dynamic balance |
Postural sway (BPEX platform) BBS |
|
Daniel, 2012 (52) 3 |
23 40% 77 (5.3) |
Community-dwelling older adults |
Nintendo Wii Sports + weight vest |
Seated exercise No therapy |
45 min 3 × /week 15 weeks |
Laboratory |
Activity limitation Balance confidence |
Senior Fitness Test: 30 s STS 30 s arm curls no. of steps in 2 min chair sit & reach 8 ft up & go 15 ft WT CHAMPS LLFDS ABC scale |
|
Fitzgerald et al., 2010 (50) 4 |
28 55% 26.2 (2.7) |
Healthy young adults |
Exergaming using Dell Computers & Concept Wobbler |
Traditional balance programme |
15 min 3 × /week 4 weeks |
Laboratory |
Dynamic balance |
SEBT DPSI |
|
Franco et al., 2011 (53) 5 |
32 78% 78.27 (6) |
Community dwelling older adults |
Nintendo Wii Fit |
Traditional balance programme |
10–15 min 2 × /week 3weeks |
Laboratory |
Dynamic balance |
BBS Tinetti Gait & Balance assessment |
|
Fritz et al., 2013 (30) 7 |
30 Unknown 66.1 (9.7) |
Chronic stroke |
Nintendo Wii Fit & Sports PlayStation EyeToy2 & Kinetic |
No therapy |
50–60 min 4 × /week 5 weeks |
Laboratory |
Dynamic balance Activity limitation |
Fugl-Meyer Assessment BBS DGI 6 min WT 3 m WT TUGT |

|
Table II. Contd. |
||||||||
|
Study PEDro Score (/10) |
Subjects, n Females, % Age, mean (SD) |
Health condition |
Intervention |
Comparison |
Dosage |
Setting |
Outcome measures |
|
|
Gil-Gomez et al., 2011 (31) 6 |
17 35% 47.3 (17.8) |
Chronic stroke TBI Cerebral neoplasm |
eBaViR (modified WBB) |
Traditional balance programme |
60 min 3–5 × /week 4–6 weeks |
Outpatient clinic |
Dynamic balance Activity limitation |
BBS BBA Anterior Reach Test Stepping Test Timed Stair Test 1 min WT 10 m WT TUGT 30 s STS |
|
Hinman, 2002 (54) 4 |
88 63% 72 |
Community dwelling older adults |
Biodex Balance System |
Home exercise programme No therapy |
20 min 3 × /week 4 weeks |
Laboratory |
Dynamic Balance Activity Limitation Falls Efficacy |
BBS Timed 50 ft WT Modified FES |
|
Jung et al., 2012 (32) 6 |
21 38% 62.1 (6.9) |
Chronic stroke |
Virtual-reality Treadmill Training (Mybud, Accupix, Gyeonggi-do) |
Usual treadmill training |
30 min 5 × /week 3 weeks |
Laboratory |
Activity limitation Balance confidence |
TUGT ABC Scale |
|
Laver et al., 2012 (28) 8 |
44 80% 84.9 (4.5) |
Hospitalized older adults (mix of fractures, falls, medical and surgical) |
Nintendo Wii Fit |
Conventional physiotherapy |
25 min 5 × /week duration of IP admission (usually 6 sessions ± 2) |
Acute hospital |
Dynamic Balance Balance Confidence Activity Limitation |
Modified BBS ABC Scale TUGT FIM SPPB Timed IADL |
|
Marioni et al., 2013 (42) 5 |
30 40% 45 (7) |
Acute vestibular |
VRS system (computerized posturography) |
No therapy |
30 min 1 × /week 5 weeks |
Laboratory |
Static Balance |
Modified CTSIB LOS (computerized) |
|
Melong & Keats, 2013 (51) 4 |
20 60% 19.7 (1.2) |
Healthy young adults |
Nintendo Wii Fit |
Traditional balance programme |
20min 3 × /week 4 weeks |
Laboratory |
Static Balance |
Stabilometer |
|
Mirelman et al., 2009 (33) 7 |
18 17% 61.4 (9.1) |
Chronic Stroke |
Rutgers Ankle Rehabilitation system |
Rutgers ankle rehabilitation system without virtual-reality |
60 min 3 × /week 4 weeks |
Laboratory |
Dynamic Balance Activity limitation |
BBS Patient Activity Monitor Lower Extremity Fugl-Meyer Scale 6 min WT 7 m WT |
|
Mirelman et al., 2010 (34) 6 |
18 17% 61.4 (9.1) |
Chronic Stroke |
Rutgers Ankle Rehabilitation system |
Rutgers ankle rehabilitation system without virtual-reality |
60 min 3 × /week 4 weeks |
Laboratory |
Activity limitation |
Gait speed and kinematics (VICON) |
|
Nilsagard et al., 2013 (35) 7 |
84 76% 49.7 (11.3) |
Multiple sclerosis |
Nintendo Wii Fit |
No Therapy |
30 min 2 × /week 6–7 weeks |
Laboratory |
Dynamic balance Activity limitation Balance confidence |
FSST Dynamic Gait Index TUGT TUGT + cognitive task 25 ft WT Timed Chair Stand ABC Scale |

|
Table II. Contd. |
||||||||
|
Study PEDro Score (/10) |
Subjects, n Females, % Age, mean (SD) |
Health condition |
Intervention |
Comparison |
Dosage |
Setting |
Outcome measures |
|
|
Pluchino et al., 2012 (55) 4 |
40 63% 72.5 (8.4) |
Community dwelling older adults |
Nintendo Wii Fit |
Tai chi Traditional balance programme |
60 min 2 × /week 8 weeks |
Laboratory |
Static balance Dynamic balance Activity limitation Balance confidence Falls efficacy Falls risk |
One-Leg Stance Force plate COP Dynamic posturography Functional reach test TUGT Tinetti POMA ABC Scale FES FROP-COM |
|
Prosperini et al., 2013 (36) 6 |
36 69% 36.2 (8.7) |
Multiple sclerosis |
Nintendo Wii Fit |
No therapy |
30 min daily 12 weeks |
Home |
Static balance Dynamic balance Activity limitation Falls frequency |
Force plate COP (ProKin) FSST 25 ft WT Number of falls (reported) |
|
Qutubuddin et al., 2007 (47) 3 |
15 0% 72.8 (6.8) |
Parkinson’s Disease |
Smart BalanceMaster |
Conventional physiotherapy |
30 min 2 × /week 4 weeks |
Outpatient clinic |
Static balance Dynamic balance |
SOT Adaption test LOS (BalanceMaster) BBS |
|
Rendon et al., 2012 (43) 6 |
40 39% 84.4 (5.2) |
Community dwelling older adults |
Nintendo Wii Fit |
No therapy |
35–45 min 3 × /week 6 weeks |
Outpatient clinic |
Activity limitation Balance confidence |
8 ft Up & Go ABC scale |
|
Rossi-Izquierdo et al., 2011 (45) 4 |
24 67% 51.7 |
Chronic Vestibular |
Smart BalanceMaster |
Optokinetic stimulation |
15–20 min daily 5 days |
Outpatient clinic |
Static balance |
SOT LOS (BalanceMaster) |
|
Schoene et al., 2013 (37) 7 |
37 unknown 78 (5) |
Community dwelling older adults |
Dance Dance Revolution Stepmania |
No therapy |
15–20 min 2–3 × /week 8 weeks |
Home |
Dynamic balance Activity limitation Falls efficacy Falls risk |
Choice Stepping Reaction Time Alternate Step Test INHIB stepping task TUGT TUGT Cognitive 5 × Sit to Stand FES PPA |
|
Singh et al., 2012 (38) 6 |
38 100% 62.6 (4.8) |
Community dwelling older adults |
Nintendo Wii Fit |
Traditional balance programme |
40 min 2 × /week 6 weeks |
Laboratory |
Balance confidence Falls risk |
ABC scale FallsScreen PPA |
|
Singh et al., 2013 (56) 5 |
38 100% 62.6 (4.8) |
Community dwelling older adults |
Nintendo Wii Fit |
Traditional balance programme |
30 min 2 × /week 6 weeks |
Laboratory |
Static balance Dynamic balance Activity limitation |
Postural sway (ProBalance) Ten Step Test TUGT |
|
Sparrer et al., 2013 (46) 3 |
71 62% 43.5 (3.5) |
Acute vestibular |
Nintendo Wii Fit |
No therapy |
45 min daily 5 days |
Laboratory |
Static balance |
SOT (EquiTest) One-leg stance (Wii) |

|
Table II. Contd. |
||||||||
|
Study PEDro Score (/10) |
Subjects, n Females, % Age, mean (SD) |
Health condition |
Intervention |
Comparison |
Dosage |
Setting |
Outcome measures |
|
|
Sun Woo et al., 2012 (48) 5 |
55 71% 74.1 (5) |
Type 2 Diabetes |
PlayStation Eye Toy |
Education only |
50 min 2 × /week |
Laboratory |
Static balance |
Postural sway (PDM Forceplate) |
|
Szturm et al., 2011 (39) 7 |
30 63% 80.8 (7.5) |
Community dwelling older adults |
Exergaming using FSA Pressure Mat |
Traditional balance programme |
45 min 2 × /week |
Outpatient clinic |
Static balance Dynamic balance Activity limitation Balance confidence |
Modified CTSIB BBS GaitRite TUGT ABC scale |
|
Toulotte et al., 2012 (44) 4 |
36 61% 75.1 (10.3) |
Community dwelling older adults |
NintendoWii Fit |
No therapy Conventional physiotherapy Wii + Conventional PT |
60 min 1 × /week |
Laboratory |
Static balance Activity limitation |
COG (Wii) Unipedal test Tinnetti questionnaire |
|
Wolf et al., 1996 (57) 4 |
200 81% 76.2 (8) |
Community dwelling older adults |
Computerized Balance Training using Chattecx |
Education only tai chi |
45 min 1 × /week |
Laboratory |
Falls risk Falls efficacy Activity limitation |
Time to falls occurrence Number of falls Fear of falls 12 min WT IADL Scale |
|
Yang et al., 2008 (40) 6 |
24 42% 61 (9.8) |
Chronic Stroke |
Virtual-reality Treadmill Training (Fastrack, Pohlemus) |
Standard treadmill training |
20 min 3 × /week |
Laboratory |
Activity limitation Balance confidence |
10 m WT Community walk test (400 m) WAQ ABC Scale |
|
Yen et al., 2011 (41) 7 |
42 21% 78 (5) |
Parkinson’s Disease |
Computerized Balance Board (+Virtools) |
No therapy Traditional balance programme |
30 min 2 × /week |
Laboratory |
Static balance |
SOT SOT + cognitive task reaction time (SMART Balance System) |
|
SEBT: Star Excursion Balance Test; BBS: Berg Balance Scale; STS: Sit to Stand; WT: walk test; CHAMPS: Community Healthy Activities Model Program for Seniors Physical Activity Questionnaire; LLFDS: Late Life Function & Disability Scale; ABC scale: Activities Balance Confidence Scale; DPSI: Dynamic Postural Stability Index; DGI: Dynamic Gait Index; TUGT: Timed Up & Go Test; BBA: Brunel Balance Assessment; FES: Falls Efficacy Scale; SPPB: Short Physical Performance Battery; IADL: instrumental activities of daily living; CTSIB: Clinical Test of Sensory Integration of Balance; LOS: Limits of Stability; FSST: Four Square Step Test; COP: centre of pressure; POMA: Performance Orientated Mobility Assessment; FROP-COM: Falls Risk for Older People in the Community; SOT: Sensory Organisation Test; PPA: Physical Profile Assessment Score; COG: centre of gravity; WAQ: walking ability questionnaire. |
||||||||
Adverse events and adherence
Three trials reported that there were no adverse events attributed to the use of the computerized intervention (35, 42, 46). One trial (36) of the 30, reported adverse events attributed to the use of the intervention. In this trial, 3 participants developed low-back pain and 2 participants developed knee pain from the use of the computer-based intervention. The other 26 trials failed to report whether any adverse events occurred.
Four trials reported increased levels of enjoyment and motivation when using the computerized intervention (31, 49–51). However, 3 trials reported no significant difference in compliance with the computerized intervention compared with physiotherapy (28, 47, 51).
Effect of computer-based intervention vs physiotherapy in people without a primary health condition
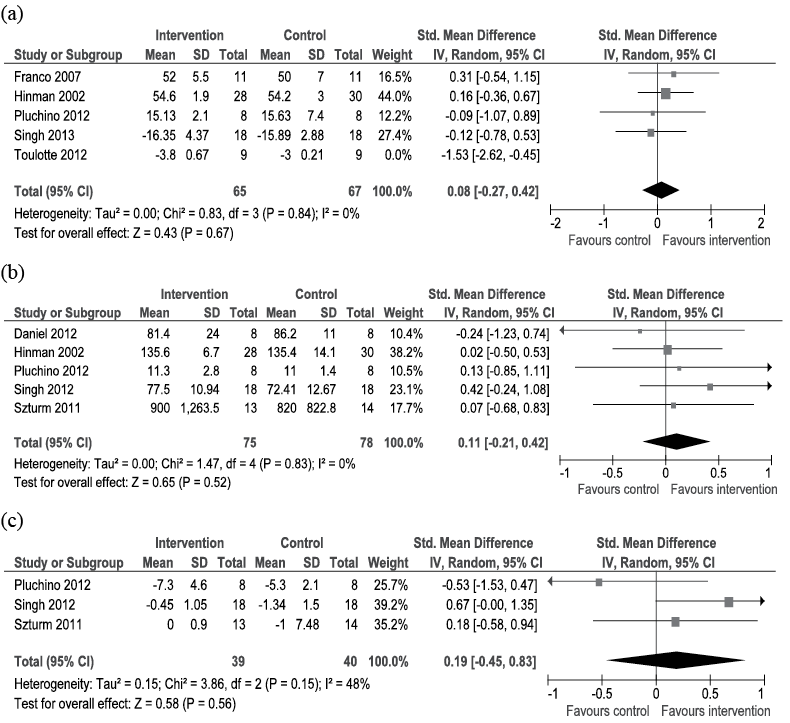
For older community-dwelling people, meta-analysis of 4 trials with 132 participants provided low-quality evidence that there was no difference in dynamic balance (Fig. 2a) compared with physiotherapy. Meta-analysis of 5 trials with 153 participants provided low-quality evidence that there was no difference in falls efficacy or balance confidence (Fig. 2b). Furthermore, 3 trials with 79 participants demonstrated low-quality evidence that there was no difference in falls risk (Fig. 2c).
Trials on community-dwelling older adults that could not be included in the meta-analysis due to clinical heterogeneity also found no difference in static or dynamic balance, balance confidence or falls efficacy, or mobility compared with physiotherapy.
The 3 trials investigating use of computer-based balance training in young healthy adults could not be included in meta-analysis as there was insufficient data. Two of these studies did not show any significant differences in postural stability compared with traditional therapies (50, 51). One trial (49) did demonstrate significant improvement in reduction of postural sway compared with physiotherapy.
Effect of computer-based intervention vs physiotherapy in people with a primary health condition
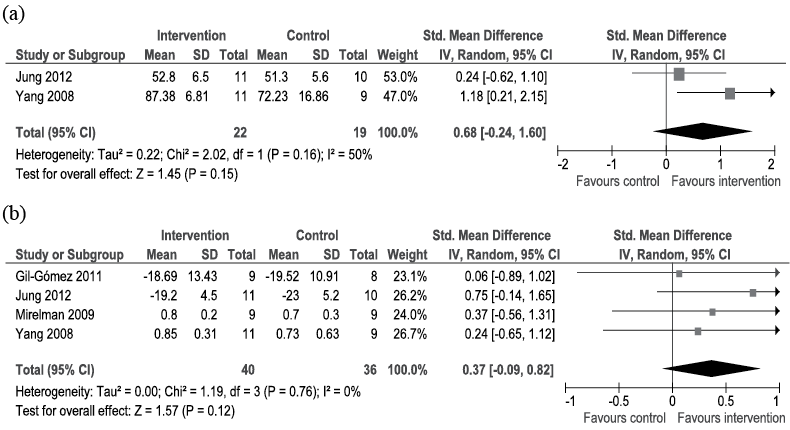
Meta-analysis of 2 trials on 41 participants with a neurological condition demonstrated low-quality evidence that there was no difference for balance confidence (Fig. 3a) compared with physiotherapy. Meta-analysis of 4 trials with 76 participants demonstrated moderate-quality evidence that there was no difference for mobility (Fig. 3b) compared with physiotherapy.
Individual trials on participants with a neurological population that could not be combined in meta-analysis due to heterogeneity found no difference in static or dynamic balance.
One high-quality study investigating computer-based balance training on a sample of people with a variety of medical conditions on an acute hospital ward (28) also did not find any differences in mobility, dynamic balance or balance confidence after 6 sessions of therapy for the duration of their inpatient admission compared with physiotherapy.
Effect of computer-based intervention vs no therapy in people without a primary health condition
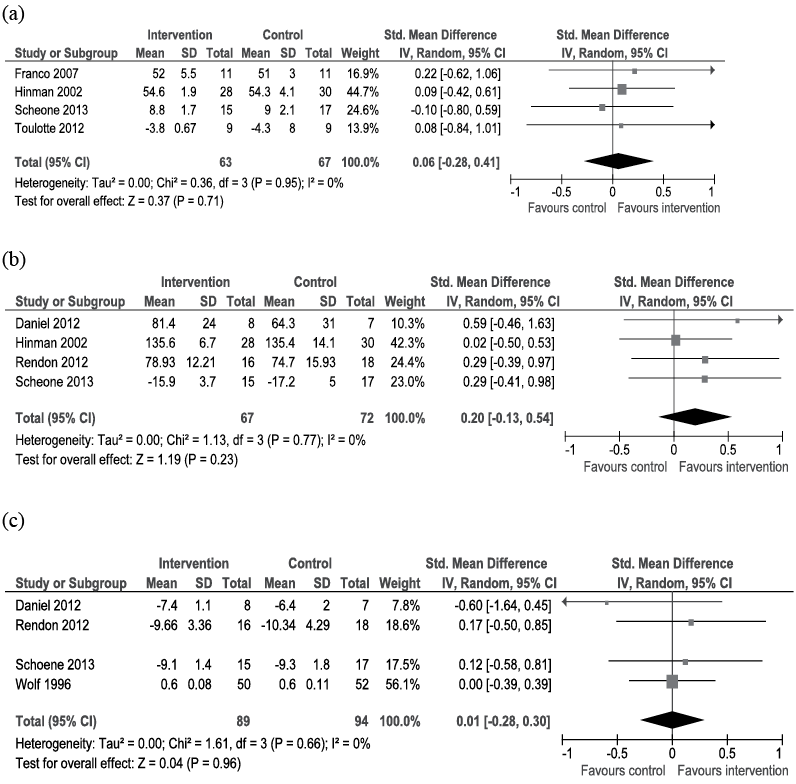
Meta-analysis of 4 trials with 130 community-dwelling older adults demonstrated low-quality evidence that there were no differences for dynamic balance (Fig. 4a) compared with no therapy. Meta-analysis of 4 trials with 139 participants also demonstrated low-quality evidence that there were no differences for falls efficacy and balance confidence (Fig. 4b) compared with no therapy. Meta-analysis of 4 trials with 183 participants also demonstrated low-quality evidence that there was no difference for mobility (Fig. 4c) compared with no therapy.
Individual trials that could not be included in the meta-analysis due to clinical heterogeneity found no difference in static or dynamic balance, or falls risk compared with no therapy.
No included trials compared the computer-based intervention with no therapy in young healthy adults.
Effect of computer-based intervention vs no therapy in people with a primary health condition
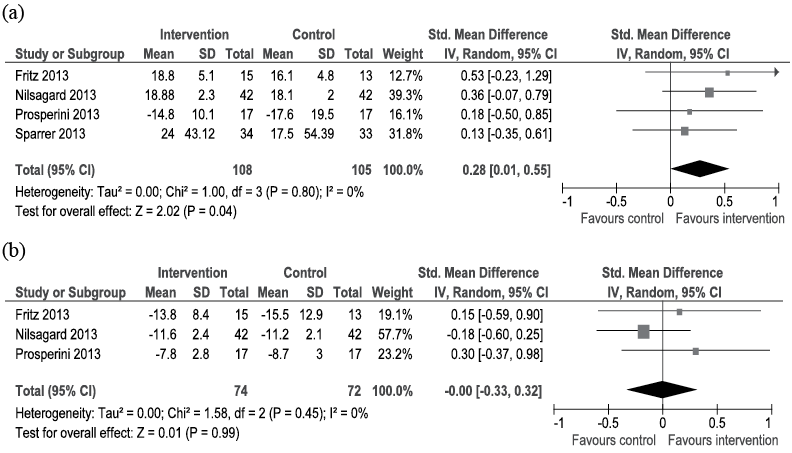
Meta-analysis of 4 trials with 213 participants with a neurological condition demonstrated high-quality evidence for improved dynamic balance immediately post intervention (Fig. 5a) compared with no therapy. Meta-analysis of 3 trials with 146 participants demonstrated high-quality evidence that there was no significant difference in mobility (Fig. 5b) compared with no therapy.
Individual trials that could not be included in meta-analysis due to heterogeneity demonstrated no difference in static balance or balance confidence in participants with acquired brain injury and multiple sclerosis (35, 36, 40) One trial on a vestibular population showed moderate effect in favour of the computer-based intervention for single-leg stance immediately post intervention, which was not sustained at 10 weeks (46). Another trial with a vestibular population demonstrated large effect in favour of the computer-based intervention for standing balance on foam with eyes open and closed immediately post and at 6 weeks post intervention (42).
One low-quality study investigating the computer-based intervention on a sample of older people with type 2 diabetes demonstrated a large effect in favour of the intervention for reducing postural sway after 10 weeks of training (48).
Discussion
The results of this systematic review of 30 randomized controlled trials provides high-quality evidence that computerized balance interventions that provide feedback improve dynamic balance in people with a neurological condition, and low-quality evidence that these devices improve static balance in people with vestibular conditions compared with no therapy. However, there was low-quality evidence that computerized balance interventions resulted in no difference in falls risk, falls and balance confidence or mobility in people who have a neurological condition compared with no therapy. In community-dwelling older adults and healthy young adults, there was low-quality evidence that computerized balance interventions resulted in no difference in balance, mobility or reduce falls risk compared with no intervention. Furthermore, compared with physiotherapy interventions used to improve balance, such as balance exercise programmes and tai chi, there was low-to-moderate-quality evidence that computerized balance interventions resulted in no difference in improving balance, falls or mobility in people regardless of age or whether a health condition was present.
Overall, these results question the usefulness of the use of computerized feedback interventions in training balance for people at risk of falling. One explanation for the lack of effect may be because of the uni-dimensional nature of the intervention. Exercise prescription, particularly in the complex area of falls and balance rehabilitation, needs to be multi-faceted and specific to the needs of individuals. Balance is a multi-system function that relies on the interaction of tactile, proprioceptive, visual and vestibular feedback in order to maintain the body’s centre of mass within the limits of our base of support during functional tasks (14, 15). It also relies on other factors, such as strength, pain, cognition and falls efficacy, to allow safe mobility (58, 59). Many of the devices included in this review predominantly focus on a single component of standing balance; the centre of pressure (18).
The results of this review may also be explained by the principle of specificity of practice; that is, the idea that you gain what you train (60, 61). Static and dynamic balance were the only outcomes that demonstrated improvement in our meta-analyses. Regardless of the type of device, their main objective is to improve balance. They do not necessarily provide a functional environment to improve other aspects of balance.
One interpretation of the results of this review is that it may not be the type of electronic device that is important, but more so the content of rehabilitation programmes that is most valuable in improving mobility and preventing falls. It appears that in this evolving world of technology, there may be too much focus on the marketing of these products for rehabilitation, with clinicians getting caught up in their popularity and not considering the evidence base for applying their use for therapy sessions. It is possible that getting back to basics and using well-designed exercise programmes and physiotherapy interventions may be more clinically effective at improving balance, mobility and reducing falls than relying on uni-dimensional computer-based interventions.
Previous research has demonstrated that, in order for exercise to be effective at reducing falls risk, it must be sufficiently challenging to balance and of high intensity (7). At least 50 hours of balance training is required to reduce falls, which equates to a twice weekly programme over 25 weeks (62). Of the trials included in this review, only 1 of 30 trials achieved this recommendation (36). The importance of exercise intensity using virtual-reality has been reported elsewhere (16). It is also possible that the interventions included in this review did not provide sufficient challenge to balance or mobility, particularly as many of the devices are designed predominantly for entertainment purposes and not for the purpose of rehabilitation (10). Furthermore, physiotherapy interventions are often multi-faceted and include falls education and environment modification, which are also important aspects for reducing falls risk (6, 63).
Our primary analysis did not consider the importance of novelty and enjoyment of using these computerized balance devices. Often balance training can become repetitive and mundane, but using these electronic devices provides a new and potentially exciting modality for therapy. It has been reported that in older, healthy populations found using computerized training was easy and enjoyable (54, 64). Three other studies on a young, university population also found higher levels of enjoyment in those who used the gaming device and subsequently found improved levels of adherence (49–51). This has important implications for adherence of balance exercise programmes in order to achieve the exercise dosage required for positive balance outcomes and maintaining these changes in clinical practice. A recent systematic review of the use of home-based virtual-reality and gaming systems demonstrated strong retention and adherence to these programmes (65). Despite this, the 3 trials in our review reporting adherence data reported no significant difference with the computerized intervention compared with physiotherapy (28, 47, 51).
The cost of purchasing these devices should also be considered when prescribing exercise for rehabilitation purposes. There is potential that their use may allow improved independence with therapy programmes and reduce need for therapist supervision, particularly in low-risk clients living in the community, as commercial gaming devices become more affordable and readily available. However, given the current lack of evidence to support the clinical advantages in using of computer-based devices for improving health outcomes compared with physiotherapy, a health economic analysis may be required.
Our findings are similar to that of previous reviews that focussed on a single intervention or single population (10, 16, 18). Our review added to the previous literature by including all computerized interventions that use feedback to potentially improve balance and did not limit the target population. Given the increasing frequency of use and development of this new technology, we were able to include 16 trials that have been published since 2011. This allowed us to conduct meta-analyses for our outcomes.
Our review followed PRISMA Guidelines (19, 20), which is the preferred reporting method for systematic reviews and meta-analysis. The GRADE approach (26) was also applied to the meta-analyses to help determine the level of confidence in the results for clinicians and policymakers. All of the studies included in the review were randomized controlled trials, which reduces risk of selection bias in increases confidence in our results.
Limitations
Limitations of this review include our search strategy, which did not include languages other than English and did not include all available databases. However, our search strategy was thorough as only 2 trials were identified with citation tracking. Another limitation is the quality of the available evidence. Much of the evidence in the meta-analyses was downgraded to low or moderate, due in part to the low-to-moderate quality of the individual trials in this review, as judged on the PEDro scale, and small sample sizes of the included trials contributing to relatively large confidence intervals around the estimated standardized mean differences. It should also be considered whether heterogeneity within subgroups of the meta-analysis as well as a variety of outcome measures that were used affected the results of the meta-analyses. For example, patients with a variety of neurological diagnoses were combined in the meta-analyses. However, the findings of individual trials in our review were consistent with the results of the meta-analyses.
Conclusion
There is high-quality evidence from 4 trials that computer-based interventions that provide feedback improve dynamic balance in people with a neurological condition compared with no therapy. There is low-quality evidence from 3 trials that computer interventions improve postural sway in people with a vestibular condition and in people with type 2 diabetes. However, there is high- to low-quality evidence that demonstrates no significant benefits for mobility, falls and balance efficacy and falls risk when using computerized interventions that provide feedback in young or community-dwelling older people, or people with other health conditions. There is low-to-moderate-quality evidence that demonstrates no significant benefits for the use of computerized interventions over traditional physiotherapy. Given the complex and multi-factorial nature of balance and falls, these results suggest that physiotherapy interventions should not be overlooked when considering the use of this emerging technology.
The authors declare no conflicts of interest.
References
Appendix I. Example of search strategy: MEDLINE n = 210 | |
Search ID# | Search terms |
S44 | S35 AND S43 |
S43 | S36 OR S37 OR S38 OR S39 OR S42 |
S42 | (MH “Placebos”) |
S41 | “(clinical adj trial$).tw |
S40 | (MH “Multicenter Study”) |
S39 | (MH “Clinical Trial”) OR (MH “Clinical Trial, Phase I”) OR (MH “Clinical Trial, Phase II”) OR (MH “Clinical Trial, Phase III”) OR (MH “Clinical Trial, Phase IV”) OR (MH “Controlled Clinical Trial”) |
S38 | (MH “Double-Blind Method”) OR (MH “Single-Blind Method”) |
S37 | (MH “Random Allocation”) OR “random allocation” |
S36 | (MH “Randomized Controlled Trials as Topic”) OR “Randomized Controlled Trials” |
S35 | S31 AND S34 |
S34 | S30 OR S33 |
S33 | (MH “Postural Balance”) OR “postur* train* OR propriocept* train*” |
S32 | S30 AND S31 |
S31 | S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S19 OR S20 OR S21 OR S22 OR S29 |
S30 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 |
S29 | “wii” |
S28 | “proprioceptive rehabilit*” |
S27 | “vestibular exerci*” |
S26 | “vestibular rehabilitat*” |
S25 | (MH “Therapeutic Exercise”) OR “exercise therap*” |
S24 | (MH “Physical Therapy”) OR “physical therap*” |
S23 | “physiotherap*” |
S22 | “equitest” |
S21 | “balance master” |
S20 | “e-rehabilitation” |
S19 | “telerehabilitat*” |
S18 | S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 |
S17 | (MH “Computer Simulation”) OR “computer simulation” |
S16 | (MH “Virtual Reality”) OR “virtual realit” |
S15 | (MH “Information Technology”) OR “information technology” |
S14 | “computer*” |
S13 | “video consol*” |
S12 | (MH “Video Games”) OR “video gam*” |
S11 | “balance machin*” |
S10 | “balance platform *” |
S9 | “e-health” |
S8 | “e-technology” |
S7 | “electronic devic*” OR (MH “Games”) |
S6 | “balance activit*” |
S5 | “balance program*” |
S4 | “balance rehabilitat*” |
S3 | “balance exerci*” |
S2 | “balance rehabilitat*” |
S1 | “balance train*” |
