David M. Simpson, MD, FAAN1, James Goldenberg, MD2, Scott Kasner, MD3, Marshall Nash, MD4, Michael J. Reding, MD5, Richard M. Zweifler, MD6, Gustavo Suarez, MD7, Ping Zhao, PhD7, Herbert R. Henney III, PharmD7, Adrian L. Rabinowicz, MD7 and Enrique Carrazana, MD7
From the 1Department of Neurology, Icahn School of Medicine at Mount Sinai, New York, NY, 2JFK Hospital, Atlantis, FL, 3Department of Neurology, University of Pennsylvania Hospital, Philadelphia, PA, 4NeuroStudies.net, Decatur, GA, 5Department of Neurology, Weill Cornell Medical College, New York, NY, 6Neurology, Sentara Neurosciences Institute and Eastern Virginia Medical School, Norfolk, VA and 7Acorda Therapeutics, Inc., Ardsley, NY, USA
OBJECTIVE: To evaluate the safety and tolerability of dalfampridine extended release (D-ER) in participants with chronic post-ischemic stroke deficits, and to assess for potential drug activity on sensorimotor function.
METHODS: Using a double-blind, placebo-controlled, crossover design, participants were randomized to placebo/ D-ER or D-ER/placebo sequences and given D-ER 10 mg or placebo twice daily. Key inclusion criteria were: ischemic stroke ≥ 6 months, Fugl-Meyer Assessment lower extremity motor score ≤ 28, ability to complete Timed 25-Foot Walk (T25FW). The primary outcome was safety and tolerability. The key exploratory measure was walking speed (T25FW). Other assessments were: Box and Block, and Grip and Pinch tests; Functional Independence Measure. Full-crossover data were analyzed using mixed-effects model.
RESULTS: A total of 83 participants were randomized: 70 completed and 13 discontinued the study. Adverse events were consistent with previous D-ER trials; no new safety signals were observed. Four participants experienced serious adverse events: 3 seizures (1 placebo, 2 D-ER), 1 was secondary to intentional overdose. Most common treatment-emergent adverse events were: dizziness, nausea, arthralgia and fatigue. Mixed-effects analysis showed an effect for D-ER vs placebo in improving walking speed (0.21 vs 0.10 ft/s; p = 0.027).
CONCLUSIONS: D-ER was generally well tolerated in participants with chronic stroke deficits. Potential drug activity on lower extremity sensorimotor function, with an improvement in walking speed, was seen.
Key words: chronic post-stroke; walking; clinical trial; humans; dalfampridine.
J Rehabil Med 2015; 47: 924–931
Correspondence address: David M. Simpson, Mount Sinai Medical Center, Department of Neurology, Box 1052, New York, NY 10029, USA. E-mail: david.simpson@mssm.edu
Accepted Oct 14, 2015; Epub ahead of print Nov 5, 2015
INTRODUCTION
Stroke is associated with persistent neurological impairment and is one of the leading causes of long-term disability (1). Although significant spontaneous neurological improvement can be expected within the first 6 months after a stroke, in general, further improvement after 6 months is limited, as impairments in limb function and abnormal gait patterns often persist (2). Since 30% of stroke survivors experience impaired ambulation by 6 months (3), a major rehabilitation goal for these patients is to improve their ambulatory ability and physical activity (4).
Walking impairment is one of the physical limitations contributing to stroke-related disability. Most stroke survivors have reduced walking speed and endurance, associated with residual spatial and temporal asymmetry (5). Reduced walking speed and capacity are major limitations for community participation, as after stroke many individuals cannot walk fast enough to cross the road safely or far enough to do the shopping (6, 7). Thus, it is not surprising that stroke survivors spend a greater part of their rehabilitation time practicing walking compared with all other activities (8).
There is currently no proven pharmacotherapy for the treatment of chronic sensorimotor deficits in patients following ischemic stroke. In a rat model of chronic stroke following permanent middle cerebral artery occlusion (pMCAO), dalfampridine, a potassium channel blocker, improved fore- and hind-limb placement and body swing in a dose-dependent manner compared with placebo (9). Dalfampridine extended release, 10 mg twice daily (D-ER; known as prolonged-release fampridine in Europe; fampridine sustained- or modified-release elsewhere), improves walking in people with multiple sclerosis (MS) (10–12).
Results from the rat pMCAO model led to the suggestion that D-ER may positively affect the sensorimotor function in patients with chronic post-stroke deficits. Thus, the primary objective of this proof-of-concept study was to evaluate the safety and tolerability of D-ER, 10 mg, administered twice daily to participants with chronic sensorimotor deficits following ischemic stroke. The study also explored the potential drug activity of D-ER relative to placebo in improving sensorimotor function in this study participant population.
METHODS
Study design
This was a multicenter, double-blind, placebo-controlled, 2-period crossover study. This early-phase proof-of-concept study was designed primarily to assess safety and tolerability of D-ER in a new patient population; based on previous MS studies, a 10-mg twice-daily dosing was tested (10, 11). A crossover design was chosen as it requires fewer participants than a parallel-arm study, and each participant serves as his or her own control to increase comparability. The study duration of 8 weeks included: 2 weeks screening, a 2-week treatment Period 1, a 1-week placebo washout, a 2-week treatment Period 2, and follow-up call at 1-week post-treatment (Fig. 1). After determining eligibility at screening, participants were randomized at Visit 2 to 1 of 2 blinded crossover treatment sequences (A or B) in a 2:1 ratio, respectively, according to a randomization schedule created prior to the start of the study; placebo followed by D-ER (Sequence A) or D-ER followed by placebo (Sequence B; Fig. 2). In previous D-ER studies in patients with MS (10, 11), a population effect size of 0.5 for any efficacy parameter provides 90% confidence to detect a signal indicative of drug effect in patients treated with placebo vs D-ER. Based on these effect size assumptions from MS studies (10, 11), the current sample size was considered adequate to show potential drug effect on sensorimotor function in participants randomized to Sequence A. The second sequence (Sequence B) was primarily included to maintain the blind for those in Sequence A.
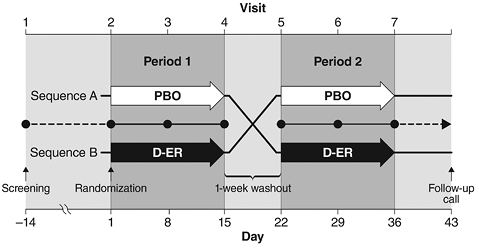
Fig. 1. Study design. Following a 2-week screening period, eligible participants were randomized in a 2:1 ratio to Sequence A or Sequence B. In Sequence A, participants received placebo (PBO) for 2 weeks in Period 1 and dalfampridine extended release (D-ER), 10 mg twice daily at 12-h intervals for 2 weeks, in Period 2; in Sequence B, participants received D-ER in Period 1 followed by PBO in Period 2. For each sequence, treatments were separated by a 1-week washout period.
The study was conducted in accordance with the principles of Good Clinical Practice and was registered at the ClinicalTrials.gov (Trial Registration Identifier: NCT01605825). The protocol was approved by each site’s institutional review board, and all participants provided written informed consent.
Study participants
Inclusion criteria were: men or women aged 18–85 years with a body mass index of 18–35 kg/m2 (13), history of ischemic stroke occurring ≥ 6 months earlier, with stable sensorimotor deficits due to stroke, as confirmed by the investigator with supportive prior imaging (magnetic resonance imaging/computed tomography); no previous use of dalfampridine or 4-aminopyridine; sufficient ambulatory ability to complete Timed 25-Foot Walk (T25FW); Fugl-Meyer Assessment (FMA) lower extremity motor score ≤ 28; and adequate cognitive ability to provide informed consent, as determined by the investigator. Exclusion criteria were: pregnant or breastfeeding participants; history of non-febrile seizures; moderate or severe renal impairment (creatinine clearance ≤ 50 ml/min using the Cockcroft-Gault Equation), or cardiovascular abnormality; urinary tract infection at screening or within prior 2 weeks, or any medical condition that could have interfered with the study; start or change of prescription or concomitant medications within 1–3 months prior to screening, or expectation of a change in concomitant therapy during the course of the study; severe depression, as indicated by a score of ≥ 30 on the Beck Depression Inventory; diagnosis of MS; history of orthopedic procedure in the extremities in the previous 6 months; or history of drug or alcohol abuse within the past year.
Outcome measures
The primary outcome measure was safety and tolerability in a sample (referred to as the safety population), defined as all randomized participants treated with ≥ 1 dose of study drug. Safety and tolerability were assessed primarily by monitoring for adverse events (AEs), including treatment-emergent AEs (TEAEs) and serious AEs (SAEs), reported at each study visit and follow-up. There were 6 study visits at weekly intervals, starting at Day 1 of treatment through Day 36 ± 1; a follow-up call was placed 1 week after the last study visit, i.e. Day 43 ± 1, to evaluate for AEs and to review concomitant medications and therapies. Severity of AEs was assessed as mild (no limitation to usual activities), moderate (some limitation to usual activities), or severe (inability to carry out usual activities). All AEs were coded using the Medical Dictionary for Regulatory Activities, version 13.1, and were classified by preferred term (14). Other safety assessments included physical examination and vital signs at each study visit, and standard laboratory assessments at the last visit of each treatment period.
Several functional exploratory endpoints were used to examine upper and lower extremity sensorimotor function. The key functional exploratory assessment defined a priori was change in walking speed, as measured by the T25FW (15). Participants were instructed to walk as fast as possible and, if needed, assistive devices were permitted, provided the same device was used at every visit. Walking speed was calculated as a mean speed of 2 trials of T25FW from a given visit; trials were separated by a 5-min interval. Other functional exploratory assessments included Functional Independence Measure (FIM) for activities of daily living (16, 17), FMA for motor and sensory function (18, 19), Box and Block test for manual dexterity, and Grip and Pinch test for hand strength (20). Grip strength was assessed using a dynamometer. The Pinch test was measured using a pinch gauge and included 3 components: Tip pinch, Key pinch, and Palmar pinch (20). In addition, Subject Global Impression (SGI) and Clinician Global Impression (CGI) scores were collected. All exploratory measures were analyzed based on the intention-to-treat principle using a sample (referred to as the full-analysis population), which included all randomized participants who took ≥ 1 dose of study medication and had a baseline assessment with ≥ 1 corresponding post-baseline assessment. Assessments were performed at every visit with the following exceptions: SGI and CGI were not assessed at Visit 1 or 2; FIM, Box and Block, Pinch and Grip tests were not assessed at Visit 1.
Analysis
The safety analysis compared the rate of overall AEs between treatments and was summarized using counts and percentages. To measure changes in exploratory endpoints, the mean change from baseline was calculated for each treatment period: the mean of Visits 3 and 4 minus Visit 2 (baseline) for Period 1 and the mean of Visits 6 and 7 minus Visit 5 (baseline) for Period 2. For this analysis, if Visit 4 assessment was missing, it was imputed using Visit 3 assessment for Period 1; likewise, if Visit 7 assessment was missing, it was imputed using Visit 6 assessment for Period 2. To compare changes within a sequence (intra-participant: Period 1 vs Period 2), paired t-tests were used. To compare changes between treatment groups (inter-participant: Sequence A vs Sequence B at each period), 2 sample t-tests were used. Analysis of full-crossover data was based on a mixed-effects model with sequence, period, visit, and treatment as fixed effects, and participants as random effect. Sensitivity analyses were performed separately with age and baseline walking speed as covariates. No missing data imputation was performed for the mixed-effects model analysis. The overall type I error rate was not protected for this study; nominal p-values were reported. Treatment differences were considered statistically significant at p < 0.05.
Assessment of community ambulation: post-hoc analysis
Community ambulation is the ability to integrate walking with other tasks in a complex environment (21). Using normal walking speeds as an indicator of impaired mobility in stroke survivors, previous studies have stratified ambulatory ability into 3 distinct clinically meaningful categories based on walking speed using the 10-meter walk test: full community ambulation (mild impairment) at > 2.62 ft/s (> 0.8 m/s), limited community ambulation (moderate impairment) at 1.31−2.62 ft/s (0.4–0.8 m/s), and household ambulation (severe gait impairment) at < 1.31 ft/s (< 0.4 m/s) (22, 23).
To determine changes in the projected community ambulation categories, a descriptive post-hoc analysis was performed by mapping walking speeds from T25FW to the established 10-meter walk ambulatory category speed thresholds (17, 18); because of the small sample size, statistical comparisons were not done. Participants were categorized at baseline of Period 1 and at last visit in Period 1 (Visit 4) to determine whether a projected shift in ambulatory category occurred, based on walking speed. The percent of participants in each ambulation category who exhibited a ≥ 20% increase in walking speed was also determined, regardless of whether this resulted in a shift in ambulation category.
RESULTS
Study participant disposition, demographics, and baseline characteristics
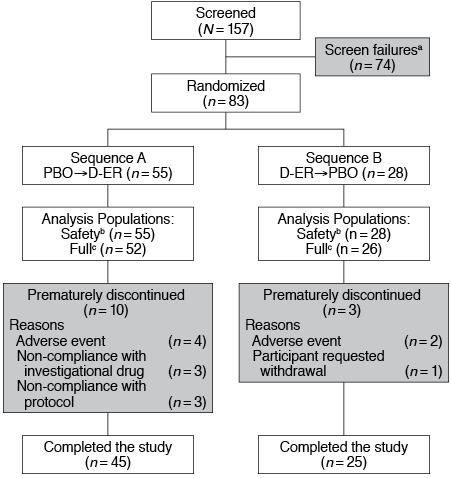
A total of 157 participants were screened at 20 centers in the USA and 83 were randomized: 55 into Sequence A and 28 into Sequence B (Fig. 2). Of those randomized, 84.3% completed the study, with similar percentages of completers in each treatment sequence. Thirteen (15.7%) participants discontinued, most frequently due to an AE: 5 (6.5%) on D-ER; 1 (1.2%) on placebo. Study participant demographics and baseline characteristics are summarized in Table I. Nearly twice as many men were enrolled compared with women; age ranged from 40 to 80 years. Groups were similar, except that the mean age of participants randomized to Sequence A was lower (57.5 years) than those randomized to Sequence B (63.5 years; p = 0.008). Of those randomized, 78.3% experienced a single ischemic stroke of the middle cerebral artery at a mean of 50 months prior to screening. The most frequent concomitant medications included anti-thrombotic agents, lipid-modifying agents, ace inhibitors, beta blockers, anti-depressants, drugs for peptic ulcers and gastroesophageal reflux, and muscle relaxants.
|
Table I. Study participant disposition and baseline characteristics |
||||
|
Variable |
Sequence A (Placebo→ D-ER) |
Sequence B (D-ER→ Placebo) |
Combined |
p-valuea |
|
Analysis populations, n (%) |
||||
|
Randomized |
55 |
28 |
83 |
|
|
Safety |
55 (100) |
28 (100) |
83 (100) |
|
|
Full |
52 (94.5) |
26 (92.9) |
78 (94.0) |
|
|
Completed study |
45 (81.8) |
25 (89.3) |
70 (84.3) |
|
|
Sex, n (%) Female Male |
18 (32.7) 37 (67.3) |
10 (35.7) 18 (64.3) |
28 (33.7) 65 (66.3) |
0.810 |
|
Age, years, mean (SE) |
57.5 (1.31) |
63.5 (1.68) |
59.5 (1.08) |
0.008 |
|
No. of ischemic strokes, n (%) |
||||
|
1 > 1 |
45 (81.8) 10 (18.2) |
20 (71.4) 8 (28.6) |
65 (78.3) 18 (21.7) |
0.388 |
|
Months since last strokeb |
||||
|
Mean (SE) (min, max) |
53.1 (9.22) (5, 417.5) |
43.1 (6.42) (7, 130) |
49.7 (6.48) (5, 417.5) |
0.467 |
|
Location of last strokec, n (%) |
||||
|
Middle cerebral artery Basilar artery Other |
30 (54.5) 9 (16.4) 17 (30.9) |
14 (50.0) 7 (25.0) 8 (28.6) |
44 (53.0) 16 (19.3) 25 (30.1) |
|
|
Baseline walking speed, mean (SE) |
||||
|
ft/s |
2.5 (0.17) |
2.1 (0.23) |
2.4 (0.14) |
0.104 |
|
m/s |
0.76 (0.05) |
0.64 (0.07) |
0.73 (0.04) |
|
|
aObtained from an analysis of variance (ANOVA) model with an effect for sequence for both duration variables, a Fisher’s exact test for type of last stroke, and a Wilcoxon signed-rank test for number of strokes. bOne participant had a missing date for their stroke prior to enrollment. Based on the imputation rules from the Statistical Analysis Plan, this participant had a time since last stroke of approximately 5 months, which is in violation of the inclusion criterion of stroke occurring ≥ 6 months. cTwo participants experienced stroke in more than one location and were counted twice. PBO: placebo; D-ER: dalfampridine extended release; SE: standard error. |
||||
Primary outcome measure: safety and tolerability
Of those assessed for safety and tolerability (n = 83), 54.5% reported ≥ 1 TEAE while on D-ER (n = 42) compared with 37% on placebo (n = 30). Most TEAEs were mild (38% vs 20%, D-ER vs placebo, respectively) or moderate (13% vs 16%, D-ER vs placebo, respectively). Two participants discontinued prematurely during treatment with D-ER because of general malaise and lower extremity weakness, which were considered as TEAEs. Overall, the most common TEAEs reported by ≥ 5% of all participants were dizziness, nausea, fatigue, insomnia, and arthralgia (Table II). Nine SAEs were reported by 4 participants, and they were withdrawn from the study (Table III). These events included 3 participants experiencing seizure, all of whom fully recovered; full work-up, i.e. brain computerized tomography scan showed no changes and they were treated and discharged without further sequelae.
|
Table II. Summary of treatment-emergent adverse events reported by ≥ 5% combined |
|||
|
MedDRA preferred term (14) |
Placebo (n = 81)a n (%) |
D-ER (n = 77)b n (%) |
All participants (n = 83) n (%) |
|
Dizziness |
2 (2.5) |
8 (10.4) |
10 (12.0) |
|
Nausea |
5 (6.2) |
3 (3.9) |
8 (9.6) |
|
Fatigue |
3 (3.7) |
4 (5.2) |
7 (8.4) |
|
Insomnia |
2 (2.5) |
4 (5.2) |
6 (7.2) |
|
Arthralgia |
3 (3.7) |
2 (2.6) |
5 (6.0) |
|
aNumber of study participants who received at least 1 dose of placebo at any time throughout the course of this crossover study. bNumber of study participants who received at least 1 dose of D-ER at any time throughout the course of this crossover study. MedDRA: Medical Dictionary for Regulatory Activities; D-ER: dalfampridine extended release. |
|||
|
Table III. Serious adverse events (SAEs) |
||
|
Treatment (sequence/period) |
SAEs MedDRA preferred term (14) |
Seizure follow-up |
|
D-ER (A/2) |
Convulsion (8 days into active treatment and following intentional overdose) Intentional overdose Suicide attempt |
Seizure, but not the intentional overdose, was assessed as possibly related to investigational drug. CT scan showed large unchanged right middle cerebral artery infarct with encephalomalacia. Participant was given levetiracetam and was weaned off before discharge; no further seizures reported. |
|
D-ER (A/2) |
Convulsion (6 days into active treatment) Microcytic anemia |
Seizure was assessed as possibly related to investigational drug. Participant was given 1 dose of lorazepam on route to the emergency department. CT scan showed a chronic right hemispheric infarct. Participant was stabilized and discharged; no further seizures reported. |
|
PBO (A/1) |
Convulsion (5 days on placebo, no prior D-ER exposure) |
Partial onset seizure. CT scan showed chronic areas of encephalomalacia in the right frontal and right occipital lobes. Participant discharged in stable condition; no further seizures reported. |
|
PBO (A/1) |
Nausea Vomiting Dehydration |
|
|
MedDRA: Medical Dictionary for Regulatory Activities; D-ER: dalfampridine extended release; PBO: placebo; CT: computerized tomography. |
||
Other safety assessments for vital signs and laboratory values did not show any clinically meaningful changes or significant differences between treatment groups.
Exploratory analysis
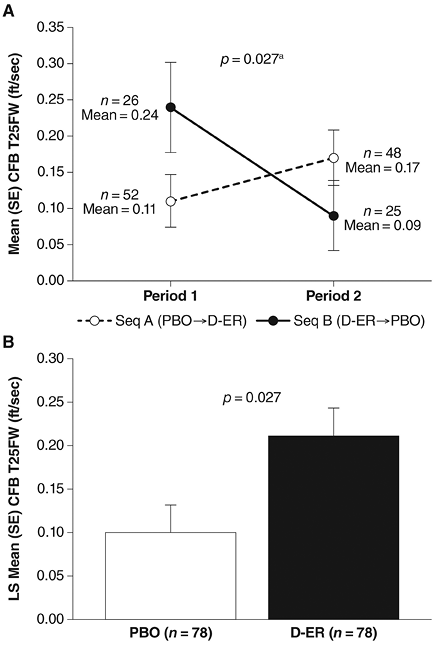
Key exploratory endpoint: change in walking speed by T25FW. Mean baseline walking speed (and standard deviation (SD)) between sequences were slightly imbalanced both periods: Period 1: 2.5 (SD 1.27) and 2.1 (SD 1.23) ft/s for Sequence A and Sequence B, respectively (p = 0.104); Period 2: 2.6 (SD 1.26) and 2.4 (SD 1.34) ft/s for Sequence A and Sequence B, respectively (p = 0.384). The mixed-effects model analysis, which took into account the effects of sequence, period, visit, and treatment, indicated an overall change in walking speed in favor of D-ER over placebo, suggestive of drug activity (p = 0.027; Figs. 3A and 3B). Sensitivity analyses performed for imbalance in age and baseline walking speeds between sequences did not alter the statistical significance of drug effect of D-ER over placebo, with p-values of 0.027 and 0.029, respectively. Individual period analysis (Fig. 3A) also showed that the mean change from baseline ± standard error trended in favor of D-ER over placebo in Period 1: 0.11 ± 0.036 vs 0.24 ± 0.062 ft/s for Sequence A (placebo) vs Sequence B (D-ER), respectively. A similar trend was observed in Period 2, but was less pronounced: 0.17 ± 0.038 vs 0.09 ± 0.048 ft/s for Sequence A (D-ER) vs Sequence B (placebo), respectively.
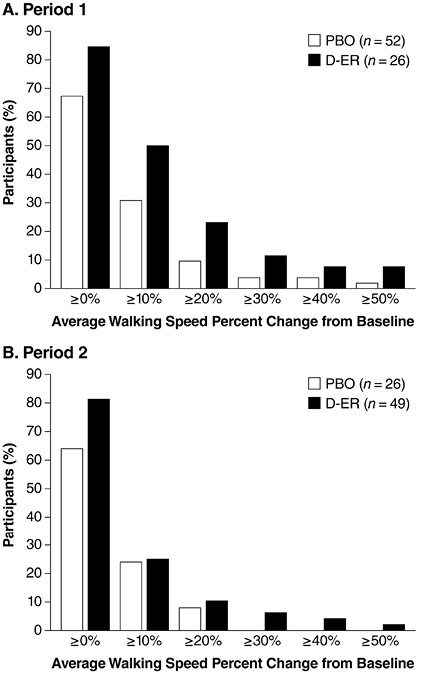
Using threshold analysis, the mean percent increase in walking speed from baseline was analyzed (Fig. 4). Although there was a numerical trend in favor of D-ER for all thresholds in both periods, the difference was more pronounced in Period 1, consistent with the result described above. Threshold analysis showed that 23% of participants treated with D-ER had ≥ 20% increase in walking speed in Period 1 compared with 9.6% in participants receiving placebo (Fig. 4). A similar trend was noted in Period 2, but less was pronounced.
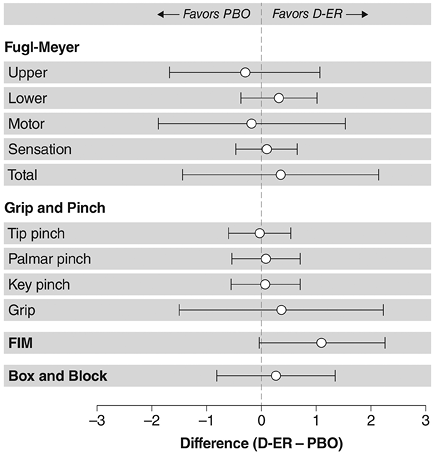
Assessment of other exploratory endpoints, including FMA (upper extremity, lower extremity, total motor functions, and sensation), Pinch and Grip, and Box and Block, showed similar baseline values between sequences (Table IV) with no significant treatment effect observed in the full-crossover model (Fig. 5). In addition, there were no significant treatment effects on the SGI and CGI scores. The FIM total score at baseline was higher in Sequence A relative to Sequence B, mean ± SE 111.4 ± 10.3 and 103.2 ± 24.1, respectively (p = 0.033). Although comparison of change from baseline for total scores revealed that D-ER was marginally higher relative to placebo in Period 1, the full-crossover model did not show significance (p = 0.059).
|
Table IV. Baseline values for other exploratory efficacy measuresa |
||||
|
Measure |
Sequence A (Placebo→D-ER) (n = 55) |
Sequence B (D-ER→Placebo) (n = 28) |
Combined (n = 83) |
p-valueb |
|
Fugl-Meyer scale, mean (SE) Upper extremity Lower extremity Motor total Sensation Motor and sensation total |
34.5 (2.73) 22.1 (0.70) 56.5 (3.22) 20.5 (0.62) 77.0 (3.47) |
35.5 (3.70) 21.1 (0.98) 56.8 (4.41) 22.0 (0.65) 78.6 (4.54) |
34.8 (2.19) 21.8 (0.57) 56.6 (2.58) 21.0 (0.47) 77.5 (2.75) |
0.838 0.375 0.955 0.127 0.784 |
|
Grip and pinch, n [mean] (SE) Tip pinch Palmar pinch Key pinch Grip |
46 [5.3] (0.71) 46 [7.0] (0.88) 50 [8.7] (1.02) 50 [25.4] (3.50) |
27 [5.5] (0.88) 26 [7.6] (1.34) 27 [9.0] (1.27) 27 [24.5] (4.14) |
73 [5.4] (0.55) 72 [7.2] (0.74) 77 [8.8 ] (0.79) 77 [25.1] (2.68) |
0.844 0.710 0.783 0.883 |
|
FIM, mean (SE) |
111.4 (1.39) |
103.2 (4.55) |
108.6 (1.83) |
0.033 |
|
Box and block, n [mean] (SE) |
47 [16.9] (2.46) |
27 [17.5] (3.20) |
74 [17.1] (1.94) |
0.885 |
|
aSafety population was used for this baseline assessment. bObtained from an analysis of variance (ANOVA) model with an effect for sequence for both duration variables, a Fisher’s exact test for type of last stroke, and a Wilcoxon signed-rank test for number of strokes. D-ER: dalfampridine extended release; SE: standard error; FIM: Functional Independence Measure. |
||||
Assessment of community ambulation: descriptive post-hoc analysis. Based on baseline speeds of Period 1, 78 participants were stratified into the projected ambulatory categories of household (mean walking speed: 0.81 ft/s [0.25 m/s]; D-ER = 9, placebo, = 10), limited community (mean walking speed: 2.02 ft/s [0.62 m/s]; D-ER, = 10, placebo = 16), and full community (mean walking speed: 3.55 ft/s [1.08 m/s]; D-ER = 7, placebo = 26). Analysis showed more participants had a positive shift from household to limited community ambulation (11.1% D-ER vs 10% placebo) and from limited community to full community ambulation (30% D-ER vs 18.8% placebo). One participant in the placebo group showed a negative shift from full community to limited community category (3.8%). There were no shifts observed from household to full community, full community to household, or limited community to household. Overall, despite the small sample size, a net positive shift in projected community ambulation was observed in favor of D-ER compared with placebo, 41.1% vs 25%, respectively.
An analysis was done of those who showed ≥ 20% increase in walking speed in Period 1 in each ambulatory category. Of those with limited community ambulation, 40% treated with D-ER had ≥ 20% increase in walking speed compared with 6.3% in participants receiving placebo. The improvement in walking speed between groups in the household category was 22.2% for D-ER vs 30% for placebo and in the full community the change was 0% for D-ER vs 3.8% for placebo.
DISCUSSION
Walking is the most affected activity in stroke. Although a major rehabilitation goal for those with chronic post-stroke deficits is to regain their ambulatory ability, currently there is no approved pharmacotherapy that improves sensorimotor deficits. Previous studies have shown that D-ER improves walking in people with MS (10, 11). In an animal model of chronic stroke, treatment with D-ER improved sensorimotor function (9). These pre-clinical data provided a strong rationale for examining the potential of D-ER in participants with chronic stroke deficits. This study determined that the safety and tolerability of D-ER 10-mg tablets administered twice daily for up to 14 days in those with a history of chronic post-stroke deficits were consistent with previous clinical trials and post-market experience in MS (10, 11, 24). There were no new safety signals identified in this sample of stroke survivors, and the reported TEAEs were comparable with Food and Drug Administration-approved product labeling for D-ER (12). In addition, this served as an exploratory study to identify evidence of activity of D-ER on measures of sensorimotor function.
Stroke is a risk factor for seizures and subsequent development of epilepsy (25, 26). The risk of late-onset seizures is high among those with a history of early-onset seizures and hemorrhagic stroke. The cumulative risk of late-onset seizures occurring at 1- and 4-year time-points after the initial stroke is 3.1% and 5.5%, respectively (27, 28). D-ER is contraindicated in patients with a history of seizure (12). Thus, patients with hemorrhagic stroke and those with a seizure history, except for febrile seizures, were excluded from the current study. In addition, by including only those with ≥ 6 months of post-stroke deficits, the study recruited a sample beyond the period of early-onset seizure risk. Despite these prospective measures, 3 participants experienced a seizure during the study: 1 during treatment with placebo prior to D-ER exposure, 1 during treatment with D-ER, and 1 following an intentional overdose of D-ER. The overdose was determined by the study investigator to be a suicide attempt that was unrelated to investigational drug. Thus, in this small study, the incidence of seizure was not greater with D-ER at the appropriate dose of 10 mg twice daily, compared with placebo. However, higher doses have been shown to increase the risk of seizure in the MS population (12).
Although this study was not designed to assess efficacy of D-ER in improving sensorimotor function, exploratory assessment for walking speed in the full-crossover model, which took into account the confounding effects of sequence, period, and visits, showed a signal favoring D-ER relative to placebo on walking in study participants. This treatment effect was consistent regardless of imbalance in age or baseline walking speed, as confirmed by sensitivity analyses. The overall change from baseline in walking speed was significant and, on average, participants in both sequences had numerically larger improvements in T25FW with D-ER than with placebo.
Minimal clinically important difference (MCID) represents the smallest change in score in an outcome measure that a patient would perceive as beneficial. Currently, the minimal change in walking speed, as measured by T25FW, that is clinically meaningful and associated with an important difference has not been determined in chronic stroke survivors. Using 10-m walk data (29) from a sub-acute stoke population (stroke onset of 30–150 days), Perera et al. (30) estimated that the gait speed in the range of 0.04–0.06 m/s would constitute a small meaningful change, corresponding to 6–9% change from baseline speed; 0.08–0.14 m/s was estimated as a substantial meaningful change, corresponding to 12–22% change from baseline gait speed. In the current study, given the lack of such reference values for T25FW walking speed in chronic stroke participants, ≥ 20% increase from baseline walking speed was considered as a clinically meaningful change. This threshold is also consistent with studies of the MCID in MS (31). At this threshold, in the current study, a higher proportion of participants showed improvement with D-ER relative to placebo (23% vs 9.6%, respectively).
An increase in walking speed may improve the community ambulation category in patients with stroke (23). Although descriptive and preliminary, a post-hoc analysis that inferred projected community ambulation categories from walking speeds suggested a positive shift in favor of D-ER over placebo, with shifts to higher categories of ambulation. Limitations of this post-hoc analysis include small sample size and that walking speeds were measured as fastest safe walking speed, whereas speeds for ambulation category thresholds were established using a normal comfortable pace. There were higher proportions of participants who had ≥ 20% improvement in walking speed within the household and limited community ambulatory categories relative to those that shifted categories, suggesting that some participants may have had meaningful improvements without having crossed the threshold speeds defining the ambulatory categories. However, because of the small sample size, an assessment of the clinical significance of this within-category improvement or shift between categories was beyond the scope of the study.
The lack of signal indicating activity of D-ER in upper extremity motor measures may have been influenced, at least in part, by the fact that the study inclusion criteria did not require upper extremity deficits at baseline. In addition, it is possible that some effects may take longer to be expressed and that the duration of the study may not have been sufficiently long for improvements to be detected; however, the long-term effects of D-ER have not been determined.
In conclusion, this short-term study with a 14-day treatment period showed safety findings that were consistent with previous safety data (10, 11, 24), indicating that there were no new safety concerns for use of D-ER in participants with a history of stroke. Despite the lack of evidence to suggest that potassium channel blockade by dalfampridine improves post-stroke sensorimotor deficits, exploratory functional assessments together with the previously reported animal model findings suggest that D-ER may have an effect on sensorimotor deficits, specifically on walking speed (9). Future studies are planned to evaluate the clinical development of D-ER in patients with chronic post-stroke deficits.
ACKNOWLEDGMENTS
This research was funded by Acorda Therapeutics, Inc., Ardsley, NY, USA.
The authors would like to thank Bagi Ravishankar, PhD, Risa Torkin, PhD, Mike Klingler, and Holly Roberts, MD, of Acorda Therapeutics, Inc., for their assistance with manuscript development. A full listing of study investigators is provided below under Collaborators. Editorial assistance was provided by The Curry Rockefeller Group, LLC, Tarrytown, NY, and was funded by Acorda Therapeutics, Inc.
Collaborators. Pasquale Fonzetti, MD, PhD, The Burke Rehabilitation Hospital, White Plains, NY; Srinath Kadmi, MD, FRCS, Associated Neurologists of Southern CT, PC, Fairfield, CT; Jason Greenberg, MD, Helen Hayes Hospital, West Haverstraw, NY; Aleksandra Pikula, MD, Boston Medical Center, Boston, MA; Rodney Johnson, MD, Neurological Associates of Washington/Clinical Trials of America, Inc, Bellevue, WA; Victor W. Mark, MD, University of Alabama at Birmingham, Birmingham, AL; Phaniraj Iyengar, MD, Neuroscience & Spine Institute, Charlotte, NC; Jonathan Harris, MD, Neurological Consultants, PA, Fort Lauderdale, FL; David Brown, MD, Hoag Memorial Hospital Presbyterian, Newport Beach, CA; Daniel A. Duffy, DO, PLC, St Mary’s of Michigan Field Neurosciences Institute, Saginaw, MI; Thomas Hemmen, MD, University of California, San Diego, La Jolla, CA; Thomas Polisoto, MD, Mercy Hospital of Buffalo, Buffalo, NY; Dennis Dietrich, MD, Advanced Neurology Specialists, Great Falls, MT; Cary Twyman, MD, Associates in Neurology, PSC, Lexington, KY; James McKinney, MD, UMDNJ – Robert Wood Johnson Medical School, New Brunswick, NJ; John Rothrock, MD, Renown Neuroscience Institute, Reno, NV, USA.
Conflicts of interest and funding. David M. Simpson has received research grants from Allergan, Merz, Ipsen, Astellas, and CSL Behring; has received honoraria from Astellas; and is a consultant to Astellas, Merz, Ipsen, Acorda Therapeutics, Inc., and Allergan. Scott Kasner has received research grants from WL Gore, Acorda Therapeutics, Inc., and Daiichi Asubio; has received royalties from UpToDate; and is a consultant to AstraZeneca, Merck, Novartis, Medtronic, Daiichi Sankyo, Pfizer, AbbVie, and Boehringer Ingelheim. Marshall Nash has received a research grant from Acorda Therapeutics, Inc. Michael J. Reding has received a research grant from and is a consultant to Acorda Therapeutics, Inc., and is a member of the American Society of Neurorehabilitation. James Goldenberg and Richard M. Zweifler report no disclosures; Richard M. Zweifler was an employee of Sentara Neurosciences Institute at the time of study. Ping Zhao, Adrian L. Rabinowicz, and Enrique Carrazana are employees of Acorda Therapeutics, Inc. and, as such, have received stock and/or stock options. Gustavo Suarez and Herbert R. Henney were employees of Acorda Therapeutics, Inc. at the time of study.
REFERENCES
