Mireille M. D. van der Linden1, Dominique C. van Rappard1, Joost G. Daams2, Mirjam A. G. Sprangers3Phyllis I. Spuls1 and John de Korte1
1Department of Dermatology, 2Medical Library, 3Department of Medical Psychology, Academic Medical Centre, Amsterdam, The Netherlands
Health-related quality of life (HRQoL) of rosacea patients is a relevant outcome measure in research and clinical practice. A review of the literature was systematically carried out regarding levels of HRQoL of patients with rosacea, including associations between HRQoL scores, demographic and clinical characteristics. Searches were performed in Cochrane, PubMed, EMBASE, PsycINFO, CINAHL and LILACS. HRQoL studies in patients with cutaneous rosacea, using validated HRQoL instruments, published between 1991 and 2014, were included. Data extraction was performed independently by 2 authors. Study design, demographics, clinical characteristics and HRQoL scores were summarized per HRQoL questionnaire. Associations between HRQoL, demographic and clinical characteristics were explored. Out of 984 references, 12 studies were included. Three HRQoL instruments were used: Short Form-36 (SF-36), Dermatology Life Questionnaire Index (DLQI) and Rosacea Quality of Life Index (RosaQoL). Because of the heterogeneity of the included studies, data synthesis was hardly feasible. All studies reported a negative impact on HRQoL, which appeared to be associated with disease severity and age. Results regarding the association with sex and subtype were mixed. With regard to the clinical relevance of HRQoL scores of rosacea patients, it seems that rosacea has a small to moderate effect on HRQoL. Key words: rosacea; health related quality of life; literature review.
Accepted Sep 30, 2014; Epub ahead of print Oct 1, 2014
Acta Derm Venereol 2014; XX: XX–XX.
Mireille M. D. van der Linden, Department of Dermatology, Academic Medical Centre, University of Amsterdam, Postbus 22660, NL-1100 DD Amsterdam, The Netherlands. E-mail: m.m.vanderlinden@amc.uva.nl
Health-related quality of life (HRQoL) of rosacea patients is a relevant outcome measure in research and clinical practice. In the 2011 update of the Cochrane Review of interventions for rosacea, HRQoL was considered to be the most important outcome parameter (1). In a number of studies, including clinical trials, the impact of rosacea on HRQoL has been described (2–13). In order to establish the level of HRQoL of rosacea patients, a systematic review was performed, including studies using standardized questionnaires.
Rosacea is a common, chronic inflammatory disorder, primarily affecting the face, characterized by the presence of flushing, erythema, papules, pustules and telangiectasia, with or without ocular signs and symptoms. In European studies, a prevalence of 2–10% has been reported (14, 15). In the USA, approximately 5% of the population has rosacea, but most of them do not know that they have it (16).
In 2002, the National Rosacea Expert Committee (NREC) defined 4 subtypes of rosacea based on morphological characteristics, with 3 cutaneous subtypes: (i) erythematotelangiectatic, (ii) papulopustular, (iii) phymatous rosacea, and (iv) ocular rosacea. Patients can have signs or symptoms of more than one subtype at the same time and progression from one subtype to another may occur (17, 18).
The cause of rosacea is unknown and its pathogenesis is not well understood (19–21).
Although there is no cure for this disease, several topical as well as oral medications have proven effective in temporarily reducing signs and symptoms (1, 22–24).
HRQoL refers to aspects of our lives that are dominated or significantly influenced by our mental or physical well-being (25). HRQoL instruments are questionnaires consisting of a number of items, usually answered by choosing one of the response options. With such instruments, measurement of HRQoL results in one or more scores, reflecting the impact of the disease on various domains of HRQoL and/or on the overall HRQoL. HRQoL can be measured with generic, dermatology- and/or disease-specific questionnaires.
Rosacea primarily affects the face and patients may experience feelings of shame, embarrassment and anxiety, and they may suffer from a lack of confidence, low self-esteem, a negative body image and depression (21, 26–28). Symptoms such as erythema, inflammatory papules and pustules, flushing, burning and stinging, may also lead to physical discomfort.
It seems that physicians often tend to underestimate the negative impact of skin disease on HRQoL. Moreover, objective clinical parameters may correlate poorly with HRQoL (29, 30). In daily clinical practice, insight into patients’ experience of HRQoL may be important in the management of the disease, and can be relevant in choosing an appropriate therapy (31).
To date, no review of HRQoL studies in cutaneous rosacea has been performed. The overall objective of the present study was to systematically review the available literature on HRQoL in patients with cutaneous types of rosacea. Specific objectives were: (i) to examine the level of HRQoL of patients with rosacea and (ii) to compare these levels with norm scores of healthy populations. In addition, the associations between HRQoL, demographic and clinical characteristics will be explored.
METHODS
Bibliographic databases and keywords
Systematic searches were conducted in the following bibliographical databases: PubMed, EMBASE, PsycINFO, CINAHL and LILACS. Since an initial search in the Cochrane Library yielded no relevant results, a more comprehensive search in this resource was abandoned. Details of these systematic literature searches are described in Appendix S11. The selection of key words, was based on the following considerations: Rosacea. According to the classification of the National Rosacea Committee, 4 rosacea subtypes can be distinguished: erythematotelangiectatic, papulopustular, phymatous rosacea, and ocular rosacea. The diagnosis ocular rosacea includes several ophthalmic syndromes that are expressions of rosacea. It is difficult to define this subtype. Furthermore, more serious expressions of ocular rosacea are usually treated by an ophthalmologist. For these reasons, ocular rosacea was excluded from our search. Studies on granulomatous rosacea were also excluded: no distinct definition exists and, in most studies, granulomatous rosacea is not considered a subtype. By some clinicians, phymatous rosacea, subtype 3, is considered as a separate clinical entity. For this reason, the search was expanded by the keywords “phymatous rosacea” and “rhinophyma”. HRQoL. HRQoL usually refers to aspects of our lives that are dominated or significantly influenced by our mental or physical well-being (25). To enable cross-study comparisons between HRQoL scores, the review was limited to studies that used internationally recognized, validated questionnaires that measure HRQoL. The names of well-established, validated questionnaires were added as search terms. Based on recent studies, the following questionnaires were identified (32–35): Dermatology Life Questionnaire Index (DLQI), Dermatology Quality of Life Scales (DQOLS), Dermatology Specific Quality of Life Instrument (DSQL), General Health Questionnaire (GHQ), Nottingham Health Profile (NHP), RosaQoL, Short Form-12 (SF-12), Short Form-36 (SF-36), Sickness Impact Profile (SIP), Skindex-16, Skindex-17, Skindex-29, World Health Organization Quality Of Life-100 (WHOQOL-100) and World Health Organization Quality Of Life-BREF (WHOQOL-BREF)
Major search concepts were rosacea or rhinophyma or phymatous rosacea combined with quality of life or questionnaire or the names of the previously mentioned questionnaires. Duplicate records were excluded by reference management software (Reference Manager).
Study selection: inclusion and exclusion criteria
Based on title and abstract or, in case an abstract was not available, on title only, studies were screened using the following inclusion criteria: (i) the population studied consisted of patients with cutaneous rosacea, and (ii) the study presented HRQoL data of patients with cutaneous rosacea. Next, the selected studies were screened based on full text, using the following exclusion criteria: (i) studies with a mixed population of patients with various skin diseases, that did not present separate data on patients with rosacea, (ii) studies that did not present scores of a validated HRQoL instrument, (iii) studies with sample size less than 20, (iv) studies in which no subtype and/or grading of severity of rosacea was listed, (v) duplicate publication of data, and (vi) reviews of already included studies. In case of abstracts without full text, the authors were requested to provide the full text. If the full text was not available, studies were excluded. Finally, all references of included studies were checked for additional studies.
The selection of the studies was performed independently by 2 authors (DR, ML). Disagreements between reviewers were resolved by discussion. A third author (JdK) was consulted if agreement could not be reached.
Data extraction and critical appraisal
Data extraction was performed independently by 2 authors (DR, ML) on: 1) first author and year of publication, 2) design of study, 3) objective, 4) HRQoL questionnaire(s) used, 5) number of patients and male/female ratio, 6) selection of the sample, 7) mean age, 8) rosacea subtype, 9) disease severity, 10) HRQoL baseline scores. To assess the quality of HRQoL measurement of the studies, each study was assessed for size of study sample (i.e. 20–50; 51–200; > 200), grading of rosacea severity, classification into subtypes, comparison with persons with skin diseases other than rosacea or healthy controls (resulting in present, or absent) and the applied HRQoL instrument (indicated as (+) for a generic instrument, (++) for a dermatology specific instrument and (+++) for a rosacea-specific tool). To allow any critical appraisal, study design and level of evidence were assessed in accordance with guidelines of the National Institute for Clinical Excellence (NICE) (February 2004, updated 2005) for studies of the accuracy of diagnostic tests. Levels of evidence range from Ia (systematic review) to IV (expert opinion).
Data synthesis and comparison
To enable cross-study comparisons, studies were grouped according to the specific HRQoL instrument being used. Within these groups, HRQoL scores were compared taking subtype and severity of rosacea into account. In addition, associations between HRQoL and sex, age, rosacea severity and subtype, were summarized.
RESULTS
Study selection
The selection process is summarized in Fig. 1. After de-duplication, the literature search yielded 984 references. Based on title and abstract, or title only, 35 studies fulfilled the inclusion criteria. After full-text screening 12 articles were eligible for data extraction. No additional studies were found by checking the references of these studies.
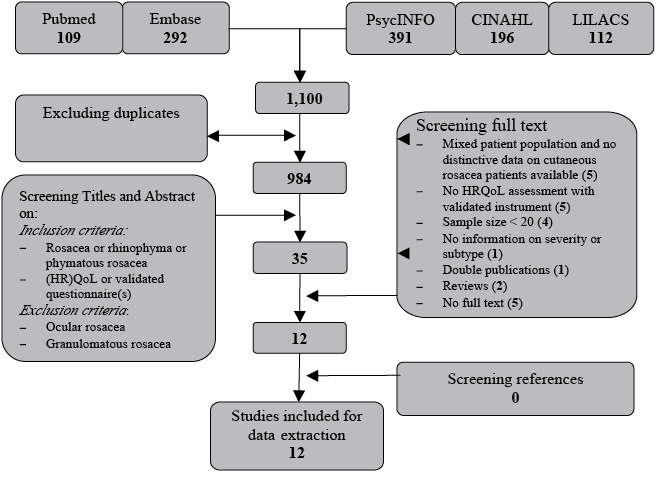
Fig. 1. Identification of studies. HRQoL: health-related quality of life.
Data extraction
Table SI1 summarizes the study characteristics of the included studies. Ten studies were written in English, one in German, and one in Polish. Six studies were interventional studies determining the efficacy of a dermatological treatment (3, 4, 6, 10, 12, 13). One study presented data on the association between HRQoL, demographic and clinical characteristics, and on the effects of various treatment modalities on HRQoL of patients with rosacea (2). Five studies were descriptive and presented data on the impact of rosacea on HRQoL (5, 7–9, 11). In all studies, measurement of HRQoL was restricted to 1 instrument. HRQoL was measured by means of 3 validated questionnaires: 1 dermatology-specific questionnaire (DLQI) (2, 5, 7, 9, 10, 12, 13), 1 disease-specific (RosaQoL) (3, 4, 6, 8) and 1 generic instrument (SF-36) (11).
The DLQI, the most commonly used instrument in clinical practice and in randomized controlled trials, is a 10-item questionnaire, assessing the impact of skin disease from the patients’ point of view regarding symptoms and feelings, daily activities, leisure, work, personal relationships and treatment. DLQI scores can range from 0 to 30. Higher scores indicate a lower degree of HRQoL. The DLQI has been validated extensively (36, 37), and its psychometric properties have been described in more than 100 studies (38). The DLQI has demonstrated excellent discriminant and construct validity as well as high reliability and internal consistency (39).
The RosaQoL is a validated disease-specific HRQoL instrument, partly derived from the dermatology-specific Skindex-29, and partly consisting of rosacea-specific questions (30). The RosaQol has demonstrated high reliability (Cronbach’s a 0.82–0.97, intraclass correlation coefficient (ICC) 0.70–0.95), and preliminary responsiveness in patients with improving rosacea. In the RosaQoL, 21 items are grouped into 3 subscales: Symptom, Emotion and Function. Questions are scaled from 1 (never) to 5 (all the time). The scores of the subscales and the total scores are averaged and range also from 1 to 5. Higher scores are indicative of worse HRQoL.
The SF-36 is a generic, extensively studied and well-validated instrument (33, 38, 40). It has been used in numerous studies, including dermatological studies. Structure and re-test reliability are somewhat controversial (32, 41). It provides scores for 8 health domains and 2 scores of a higher order: the Physical Component Summary (PCS) and the Mental Component Summary (MCS). Norm PCS and MCS scores have a mean of 50 and a standard deviation (SD) of 10 in the USA population.
Critical appraisal
Table SII1 summarizes the quality assessment of the included studies. Six studies had small sample sizes, less than 50. Disease severity was described in 7 studies, although assessment of severity was done in different ways. Classification into rosacea subtypes was reported in 8 studies. In 3 studies separate data for the different subtypes were presented, but in 2 of these studies, sample sizes were smaller than 20 (7, 8, 11).
Comparisons of HRQoL scores of patients with rosacea were made with those of persons without rosacea in 2 studies. In 7 studies the DLQI was used as HRQoL instrument. Four studies used the RosaQoL and only one study used the SF-36. Most studies had a level of evidence of II or III, primarily based on the study design and size of the population studied.
Data synthesis and comparison
The included studies showed a huge variety with respect to study design, objective and studied sample, thereby limiting data synthesis (Table SI1).
Seven studies had used the DLQI as HRQoL instrument (2, 5, 7, 9, 10, 12, 13). DLQI scores ranged from 4.1 to 17.3. The highest baseline score (17.3) was presented in the study of Shim, which was remarkably high in comparison with the other scores (12). We asked the author for an explanation for this high score; she stated that it is likely that the rosacea cases in her study were severe, because only approved severe cases of rosacea were funded in the study by Shim TN (personal communication).
According to difference in sex: HRQoL in women with rosacea was more impaired than in men, according to Aksoy (2) (pre- and post-treatment DLQI scores, p < 0.001) and Hiltscher et al. (7) (subgroups with subtype 1 and subtype 2 together (n = 28), p = 0.08). In the study of Böhm et al. (5) on the other hand, men reported significantly greater impairment of HRQoL than women (p < 0.05).
In the study of Aksoy (2) and Böhm et al. (5), baseline DLQI scores were significantly related to age (p < 0.002 and r = –0.19, respectively, p < 0.01). Being younger was related to higher (worse) DLQI scores. Differences in scores could not be explained by differences in subtypes. In the study of Aksoy, no differences were found in mean DLQI scores between the different clinical subtypes (2). Cross-study comparison of DLQI scores, with regard to rosacea severity, was difficult because grading of severity was not done, or assessed differently. In the study of Aksoy, mean DLQI scores before and after treatment were correlated with rosacea severity scores (p < 0.001) (2). In the study of Böhm et al. (5) self-assessed rosacea severity appeared to be correlated with DLQI scores (0.71).
In the study of Langenbruch et al. (9), they compared HRQoL scores of patients with rosacea with those from previous surveys of patients with psoriasis or atopic dermatitis. In this study, the mean DLQI score (SD) of rosacea patients was lower (better) than the scores of psoriasis and atopic dermatitis patients (8.5 (SD 6.0) and 6.7 (SD 6.2), respectively).
Four of the 12 included studies used the RosaQoL as instrument to assess HRQoL (3, 4, 6, 8). Overall RosaQoL scores ranged from 2.6 to 3.3. At cross-study comparison, differences in overall RosaQoL scores could not be explained by differences in rosacea subtypes. In one study, RosaQoL scores in comparison of subtypes were reported (8). In this study, the highest total score was found for subtype 3 (phymatous rosacea) (p < 0.04) (8). The difference in total RosaQoL score, compared with both subtype 1 and subtype 2 scores, was based on a significant difference in the components Emotion (p < 0.007) and Symptom (p < 0.001).
Cross-study comparison of RosaQoL scores regarding to severity of rosacea was difficult because of difference in grading of severity. None of the studies investigated the association between sex, age or rosacea severity and RosaQoL scores.
In one study, SF-36 scores, including PCS scores and MCS scores of rosacea patients, were compared with scores of persons without rosacea (11). PCS and MCS scores of rosacea patients were significantly lower (worse) than those of persons without rosacea (p = 0.0003 and p = 0.003, respectively) and also PCS and MCS scores of rosacea patients without concomitant diseases (subgroup) were significantly worse than those of healthy persons. (p = 0.02 and p = 0.003, respectively). SF-36 scores of rosacea patients were lower (worse) in all domains except for social functioning (SF) (p = 0.00001–0.03).
In rosacea patients without concomitant diseases, age and PCS scores were significantly correlated (p < 0.05). Being older was associated with worse PCS score. No association was found between age and MCS. In the healthy control group, no associations were found between age and PCS or MCS.
DISCUSSION
This review presents an overview of the levels of HRQoL of rosacea patients. All studies reported a negative impact on HRQoL. Based on the HRQoL scores of the included studies, we conclude that rosacea has a statistically significant, negative impact on patients’ HRQoL. Results regarding the association between HRQoL and sex were mixed: 2 studies (2, 7), reported worse HRQoL of women in comparison with men; however, one study (5) reported worse HRQoL of men.
HRQoL of rosacea patients is associated with age. Being younger was related to worse HRQoL in 2 studies with large sample size (2, 5). In one study with small sample size, HRQoL was more impaired in older persons (11).
HRQoL of rosacea patients is correlated with rosacea severity scores and self-assessed rosacea severity (2, 5).
Statistical significance does not provide information about the clinical meaning of the reported levels of HRQoL of patients with rosacea. To assign clinical meaning to HRQoL scores, it is important to know how to interpret these scores to the degree of impact of the disease on HRQoL. Unfortunately, relatively few data exist on the interpretability of HRQoL scores. Interpretation methods can be categorized as either distribution-based or anchor-based systems (42, 43). Distribution-based approaches use statistical characteristics of the results in terms of the underlying distribution of results in a given population. Anchor-based approaches examine the relationship between HRQoL scores of a particular instrument and an independent, external measure or anchor.
Hongbo et al. (44) used an anchor-based method to establish a banding system with ranges of DLQI scores, to support the clinical meaning of DLQI scores (0–1: no effect on patient’s life, 2–5: small effect on patient’s life, 5–10: moderate effect on patient’s life, 11–20: very large effect on patient’s life and 21–30: extremely large effect on patient’s life).
When we compare the mean DLQI scores of the included studies (with one exception: the study of Shim, in which DLQI scores were remarkably high), with the scores of the banding system, we conclude that rosacea has a small to moderate, negative impact on patients’ life (2, 5, 7, 9, 10, 12, 13).
In the study of Aksoy, patients who reported “an easy living with rosacea” had a mean DLQI score of 2.9 (SD 4.4), those who reported “sometimes hard” had a mean DLQI score of 5.0 (SD 3.9) and those who reported “always hard” had a mean DLQI score of 9.4 (SD 5.1). These scores correspond well with the scores of the banding system of Hongbo et al. (2, 44). When we compare HRQoL scores of rosacea patients with those of patients with other inflammatory skin diseases, HRQoL scores of patients with rosacea were lower (better) than the scores of psoriasis and atopic dermatitis patients (9).
Study limitations
Although HRQoL is considered to be an important outcome measure in dermatological research and practice, only 12 studies could be included. These studies showed a large variation in terms of studied population, design, HRQoL instrument and objective(s). The composition of the samples ranged from patients with a diagnosis of rosacea at a dermatology clinic to members of patients’ associations. Unfortunately, clinical characteristics, such as subtype classification, signs and symptoms and severity, were not provided in each study. Differences in grading systems between the studies made synthesis and cross-comparisons difficult. Because of this heterogeneity, it was not possible to pool data. The sensitivity of the 3 instruments used to measure HRQoL in persons with rosacea might not be equivalent. This might explain differences in conclusions according to correlations with demographic and clinical characteristics (different subtypes).
Both et al. (32) recommended the SF-36 and the Skindex-29 as instruments of choice to assess HRQoL in dermatology. The Skindex-29 might be more sensitive for assessing specific problems in rosacea than the DLQI. The RosaQoL, a rosacea-specific instrument derived from the Skindex-29, might be even more sensitive than the Skindex-29 itself. Therefore, the RosaQoL might be useful as an outcome measure for evaluating treatment or new therapies in rosacea. The following may serve as an illustration for this suggestion: in the included studies, DLQI scores of rosacea patients were not affected by clinical subtype, but, on the other hand, the highest RosaQoL total score was found for subtype 3 (phymatous rosacea) (p < 0.04) (8).
Conclusion
HRQoL measurement in patients with rosacea using DLQI, RosaQoL and SF-36, confirm that rosacea has a negative impact on HRQoL. In order to interpret HRQoL scores of rosacea patients into clinically meaningful values, it seems that rosacea has a small to moderate effect on HRQoL.
HRQoL appeared to be associated with disease severity and age: being younger was related to worse DLQI scores. No conclusion can be drawn regarding any association between sex, rosacea subtype and HRQoL.
Future studies
Future studies on HRQoL should include information on clinical characteristics as well as severity. It is likely that subtypes, signs and symptoms differ in their impact on HRQoL and, because rosacea is a chronic disease with remissions and exacerbations, HRQoL might correlate with severity of the disease.
According to van Zuuren et al., there is an urgent need for well-designed studies of several treatments on rosacea (1). Future trials should include HRQoL assessment as primary outcome (1). Dermatology-specific and disease-specific instruments are especially useful as an outcome measure for evaluating treatment or new therapies (45, 46). The RosaQoL might be the most sensitive instrument to measure changes in HRQoL, and is therefore the most suited instrument to be used in randomized controlled trials (RCTs) (30, 46).
The designers of the RosaQoL recommend that future studies are conducted to confirm its validity and responsiveness (30). The RosaQoL would be more useful if clinical meaning to RosaQoL scores in itself and clinically relevant difference in scores have been determined. Prinsen et al. (47) identified clinically meaningful cut-off scores by comparing patients’ responses to specific “anchor” questions with their Skindex-29 scores (42, 46–48). Similar to that method, clinically meaningful cut-off scores of the RosaQoL could be identified (47).
It is hoped that clinicians treating patients with rosacea will find this review helpful and that they are encouraged to use HRQoL assessments in their daily practice in order to optimize the medical treatment of rosacea.
The authors declare no conflicts of interest.

1http://www.medicaljournals.se/acta/content/?doi=10.2340/00015555-1976
REFERENCES
