OBJECTIVE: To describe the manual ability of adolescents with cerebral palsy and to investigate the relationship of manual ability with daily activities.
DESIGN: Cross-sectional study.
SUBJECTS: Ninety-four adolescents with cerebral palsy, aged 12–16 years.
METHODS: Manual ability was assessed according to the Manual Ability Classification System (MACS) and the ABILHAND-Kids. Daily activities were assessed with the Vineland Adaptive Behavior Scales (VABS) sub-scales for (personal and domestic) daily living skills. The relationship between manual ability and daily activities was investigated with regression analysis: independent variables were manual ability, disease and personal characteristics.
RESULTS: MACS and ABILHAND-Kids were both strongly associated with personal daily activities (explained variance 77% and 84%, respectively) and less strongly with domestic daily activities (explained variance 45% and 62%, respectively). Including other disease characteristics and personal characteristics in the model increased the explained variance of personal daily activities to 91% for both models and the explained variance of domestic daily activities to 68% and 73% for the MACS and ABILHAND-Kids models, respectively.
CONCLUSION: Manual ability is limited in many adolescents with cerebral palsy, and limitations in manual ability are strongly related to limitations in daily activities.
Key words: manual ability; cerebral palsy; daily activities; adolescents.
J Rehabil Med 2010; 42: 493–498
Correspondence address: Mirjam van Eck, VU University Medical Center, Department of Rehabilitation Medicine, PO Box 7057, NL-1007 MB Amsterdam, The Netherlands. E-mail: m.vaneck@vumc.nl
Submitted January 7, 2009; accepted January 20, 2010
Introduction
Several studies have reported limitations in daily activities in children and adolescents with cerebral palsy (CP) (1–4). Østensjø et al. (5) found that the Gross Motor Function Classification System (GMFCS) was a strong predictor for daily activities in children with CP, but age and learning problems were also found to be significantly, but less strongly, associated with daily activities, suggesting that an increase in accomplishment of daily activities is more dependent on the severity of the CP than on age. Comparably, in young adults with CP, restrictions in daily activities and participation were attributable to impaired gross motor functioning, a lower level of education and younger age (2). In a previous study focusing on the same cohort that was investigated in the present study, GMFCS level, learning disability and limb distribution were found to be associated with daily activities (3). The factors mentioned above explained approximately 50–80% of the variance of personal and domestic daily activities (2, 3, 5). However, although they do explain a considerable amount of variance, these results suggest that there are other factors that may be associated with daily activities. Manual ability is thought to be a possible determinant of daily activities such as dressing, personal care, and handling objects, because hand impairments contribute to difficulties experienced in performing these activities (6).
Compared with gross motor function, little attention has been paid to the arm-hand function of children with CP, although it has been reported that arm-hand function is impaired in almost 50% of patients with CP (6–8). Until a few years ago, reliable and validated instruments to measure manual ability in children with cerebral palsy were not available (9, 10). Fine motor function, measured with the Bimanual Fine Motor Function, was found to be limited in 55% of children with CP aged 5–8 years (7), and hand-grip of the affected hand was found to be moderately to severely impaired in 45% of children with hemiplegic CP aged 11–18 years (6). Restrictions in arm-hand function can lead to restrictions in the capacity to perform daily activities that require the use of the upper limbs (11). It has also been reported that hemiplegic children rarely use their involved arm and hand spontaneously in play and daily activities (6). Limitations in functional activities of the upper extremity in young adults with CP were found to be an important determinant for participation, apart from their gross motor function and level of education (12). Two studies have investigated the influence of manual ability on daily activities, and found a strong correlation between the Melbourne Assessment of Unilateral Upper Limb Function score and personal daily activities in children with CP (13). A recent study also reported a strong correlation between the Manual Ability Classification System (MACS) level and personal daily activities (14). However, in all those studies the influence of personal and disease characteristics were only minimally investigated, or not at all. Apart from the results of these studies, little is known about the influence of manual ability on daily activities in adolescents with CP. Therefore, the objective of this study was to describe the manual ability of adolescents with CP and to investigate the relationship of manual ability to daily activities.
Methods
Participants
The present study was a cross-sectional analysis of the last (fourth) measurement in a 3-year longitudinal cohort study, because the MACS and ABILHAND-Kids measurement instruments were not available when this cohort study started, and were therefore not used for the first 3 measurements. The adolescents were 12, 14 or 16 years old at this last (fourth) measurement. All children with CP who were known in rehabilitation centres, hospitals or special schools in the north-west region of the Netherlands were invited to participate (3). The exclusion criteria were: insufficient knowledge of the Dutch language and the presence of additional disorders that have an important and lasting influence on movement skills. The study protocol was approved by all the regional medical ethics committees. Of the 244 children identified, 110 children and their parents returned the written consent form with a positive response. Over the years there were a total of 16 drop-outs, resulting in 94 children participating at the last measurement. This research was performed as part of the Pediatric Rehabilitation Research in the Netherlands (PERRIN) programme (www.perrin.nl), which is a longitudinal study of functioning in children with CP.
Measures
Daily activities. Daily activities were assessed according to the (personal and domestic) daily living skills sub-scales of the Vineland Adaptive Behavior Scales (VABS) survey form (15, 16). The VABS has been designed to assess functioning, with sub-scales for motor skills, daily living skills, communication and socialization, in children aged 0–17 years, with and without disabilities (15). We used the Dutch translation of the VABS (17). The personal and domestic daily living skills sub-scales of the VABS consist of 39 and 21 items, respectively, with response categories of 0 to 2 (0 = never performed, 1 = sometimes or partly performed, 2 = usually or habitually performed), thus the scores range from 0 to 78 and from 0 to 42, respectively. The internal consistency of the sub-scale for daily living skills is 0.90, and its test-retest reliability is 0.85 (16).
Manual ability. Manual ability was measured with the ABILHAND-Kids questionnaire (10) and classified with the MACS (9). The ABILHAND-Kids measures the child’s “capacity to manage daily activities requiring the use of hands and upper limbs, whatever the strategies involved” (18). A total of 21, mainly bimanual, activities were rated by the children’s parents on a 3-point scale (0 = impossible, 1 = difficult, 2 = easy), describing their child’s perceived difficulty in performing each activity. The questionnaire was developed on the basis of the Rasch measurement model, which makes it possible to convert ordinal scores into interval scores (10). To facilitate interpretation of the analyses, the ABILHAND-Kids interval score was recalculated into a percentage of the maximum score, ranging from 0 to 100.
The MACS is a 5-level classification system that has been developed to classify the way in which children with CP use their hands when handling objects during daily activities (9). The classification is designed to reflect the child’s typical manual performance, not the child’s maximal capacity (Appendix I).
Other associated factors. Other possibly associated factors, i.e. disease characteristics (severity of the motor involvement, limb distribution and selective motor control) and personal characteristics (learning disability, age and gender), were also analysed.
The severity of the motor involvement was classified according to the GMFCS, which is a 5-level classification system according to age, in which distinctions between the levels of motor functioning are based on functional limitations, the need for assistive devices and, to a lesser extent, quality of movement (19).
Limb distribution was sub-divided into 3 categories: hemiplegia (unilateral involvement), diplegia, and tetraplegia (both bilateral involvement). Diplegia was defined as the legs being more severely affected than the arms, and tetraplegia was defined as the arms being affected as severely, or more severely, than the legs.
To measure selective motor control (SMC), the adolescents were first asked to extend the knee, and then to dorsiflex the ankle of each leg, while sitting on a bench with no support for the feet. The following scores per leg were possible: 0 = no selective movement, only synergistic movement; 1 = diminished selective movement (in the first range selective movement, followed by synergetic movement); and 2 = full selective movement during extension of the knee and dorsiflexion of the ankle (20). Knee and ankle movements were scored separately. The scores for the 2 legs together produced a total score ranging from 0 to 8. The total SMC scores were then sub-divided into 3 categories: poor SMC = total scores 0, 1, 2; moderate SMC = total scores 3, 4 or 5; and good SMC = total scores 6, 7 or 8.
Learning disability was based on type of school: children classified as having no learning disability were those who were following a regular education programme in a regular school, or in a school providing special education for physically disabled children. Children with a learning disability were those who were following special education programmes in special schools for children with learning disabilities (with or without physical disabilities), or in special day-care centres for severely (cognitive and physical) handicapped children.
Data collection
All the adolescents and their parents visited the Department of Rehabilitation Medicine at the University Medical Center. During the visit a trained researcher gathered information about diagnosis and type of school, classified the adolescents according to the GMFCS and the MACS, and carried out the physical examination. The VABS survey form was completed by a researcher from the Department of Orthopedagogy during a structured interview with the parents or with attendants of the adolescent. In addition, the parents completed the ABILHAND-Kids questionnaire.
Statistics
Statistical analyses were performed with SPSS software (version 15.0), and descriptive statistics were used to summarize manual ability. A one-way ANOVA with Tukey post hoc analyses was performed to determine differences between groups. The relationship between manual ability and VABS daily living skills was investigated with regression analysis. First, 2 models were constructed with VABS daily living skills as dependent variable, and MACS and ABILHAND-Kids as independent variables. Subsequently, the remaining independent variables were added to the model 1 by 1. The variables with a p-value < 0.1 were included in the final analysis and selected for the final model using a backward procedure. MACS, GMFCS, limb distribution, SMC and age group were included as a categorical variable, using dummy variables (21). The difference between using 5 GMFCS categories in the analysis, or using a dichotomized GMFCS (by combining levels I–III and IV–V) was only a few percent, so we included the dichotomized GMFCS to increase the statistical power.
Results
Participants
The characteristics of the 94 adolescents with CP who participated in the present study are presented in Table I.
| Table I. Characteristics of the participating adolescents with cerebral palsy (n = 94) |
| Characteristics | n |
| Gender | |
| Boys | 60 |
| Girls | 34 |
| Age group, years | |
| 12 | 28 |
| 14 | 29 |
| 16 | 37 |
| Learning disability | |
| Yes | 24 |
| No | 70 |
| Manual Ability Classification System | |
| I | 39 |
| II | 31 |
| III | 9 |
| IV | 10 |
| V | 5 |
| GMFCS level | |
| I | 50 |
| II | 6 |
| III | 10 |
| IV | 8 |
| V | 20 |
| Limb distribution | |
| Hemiplegia | 37 |
| Diplegia | 38 |
| Tetraplegia | 19 |
| Selective Motor Control | |
| Poor | 34 |
| Moderate | 16 |
| Good | 44 |
| GMFCS: Gross Motor Function Classification System. |
Manual ability
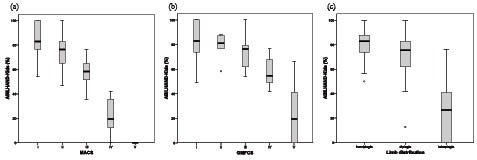
The MACS levels were distributed over several GMFCS levels (Table II). The ABILHAND-Kids score per MACS level, GMFCS level and limb distribution are presented in Fig. 1. Significant differences in ABILHAND-Kids scores were found between all MACS levels (p < 0.05) (Fig. 1a), and there were significantly lower ABILHAND-Kids scores between GMFCS V and the other GMFCS levels and between GMFCS IV and GMFCS I (p < 0.05) (Fig. 1b). Adolescents with tetraplegia had significantly lower ABILHAND-Kids scores than adolescents with hemiplegia or diplegia (p < 0.05) (Fig. 1c). No statistically significant difference was found between adolescents with hemiplegia and adolescents with diplegia.
| Table II. Distribution of Manual Ability Classification System (MACS) levels over Gross Motor Function Classification System (GMFCS) levels |
| GMFCS | I | II | III | IV | V | Total |
| MACS | | | | | | |
| I | 29 | 3 | 6 | 1 | 0 | 39 |
| II | 19 | 2 | 3 | 4 | 3 | 31 |
| III | 2 | 1 | 1 | 2 | 3 | 9 |
| IV | 0 | 0 | 0 | 1 | 9 | 10 |
| V | 0 | 0 | 0 | 0 | 5 | 5 |
| Total | 50 | 6 | 10 | 8 | 20 | 94 |
Fig. 1. Box-plot of the ABILHAND-Kids score (%): (a) per MACS level; (b) Gross Motor Function Classification System level; and (c) limb distribution. Median and interquartiles are shown.
Personal daily activities
The mean score for VABS personal daily activities was 59 (SD 20). Univariate linear regression showed that the MACS and the ABILHAND-Kids were both strongly associated with personal daily activities (explained variance 77% and 84%, respectively). GMFCS level, limb distribution, selective motor control and learning disability were also associated with personal daily activities in the univariate analyses (p < 0.1).
Table III presents the multiple linear regression models for VABS personal daily living skills. Adolescents with lower MACS levels (i.e. better manual ability) and higher ABILHAND-Kids scores, had higher scores for personal daily activities. Explained variance increased from 77% (with MACS) to 86% (GMFCS level added), 89% (limb distribution added), 90% (selective motor control added) to 91% (learning disability added; final model). Explained variance increased from 84% (with ABILHAND Kids) to 88% (GMFCS level added), 90% (limb distribution added) to 91% (learning disability added; final model).
| Table III. Multiple linear regression models for VABS personal daily living skills |
| Dependent variable: VABS personal daily living skills | B | 95% CI | p | % explained variance |
| Model with MACS | | | | Adjusted R2 0.77 |
| Constant | 70.8 | 67.7 ; 73.8 | < 0.001 | |
| MACS | | | | |
| MACS I (ref. cat.) | 0 | | | |
| MACS II | –7.1 | –11.6 ; –2.5 | 0.003 | |
| MACS III | –17.9 | –25 ; –10.9 | < 0.001 | |
| MACS IV | –45.2 | –52 ; –38.4 | < 0.001 | |
| MACS V | –60.8 | –69.9 ; –51.7 | < 0.001 | 77 |
| MACS + other characteristics | | | Adjusted R2 0.91 |
| Constant | | | | |
| MACS | 72.5 | 69.9 ; 75.1 | < 0.001 | |
| MACS I (ref. cat.) | 0 | | | |
| MACS II | –0.5 | –3.9 ; 3.1 | 0.820 | |
| MACS III | –3.5 | –8.8 ; 1.9 | 0.203 | |
| MACS IV | –17.2 | –24.1 ; –10.2 | < 0.001 | |
| MACS V | –29.1 | –37.5 ; –20.6 | < 0.001 | 77 |
| GMFCS (GMFCS I–III = 0 GMFCS IV–V = 1) | –10.5 | –16.8 ; –4.2 | 0.001 | |
| Limb distribution | | | | |
| Hemiplegia (ref. cat.) | 0 | | | |
| Diplegia | 0.83 | –2.7 ; 4.4 | 0.641 | |
| Tetraplegia | –7.1 | –13.2 ; –0.9 | 0.024 | |
| Selective motor control | | | | |
| Good (ref. cat.) | 0 | | | |
| Moderate | –4.4 | –8.5 ; –0.4 | 0.033 | |
| Poor | –8.8 | –14.7 ; –2.9 | 0.004 | |
| Learning disability | –7 | –11.4 ; –2.7 | 0.002 | 14 |
| Model with ABILHAND-Kids | | | Adjusted R2 0.84 |
| Constant | 14.8 | 10.5 ; 19.1 | < 0.001 | |
| ABILHAND-Kids | 0.7 | 0.6 ; 0.7 | < 0.001 | 84 |
| ABILHAND-Kids + other characteristics | Adjusted R2 0.91 |
| Constant | 41.9 | 35 ; 48.8 | < 0.001 | |
| ABILHAND-Kids | 0.4 | 0.3 ; 0.4 | < 0.001 | 84 |
| GMFCS (GMFCS I–III = 0 GMFCS IV–V = 1) | –11.8 | –16.3 ; –7.3 | < 0.001 | |
| Limb distribution | | | | |
| Hemiplegia (ref. cat.) | 0 | | | |
| Diplegia | –0.3 | –3.2 ; 2.7 | 0.856 | |
| Tetraplegia | –8.1 | –13.6 ; –2.5 | 0.005 | |
| Learning disability | –6.9 | –10.9 ; –2.8 | 0.001 | 7 |
| CI: confidence interval; VABS: Vineland Adaptive Behavior Scales; MACS: Manual Ability Classification System; GMFCS: Gross Motor Function Classification System.; ref. cat.: reference category. |
Domestic daily activities
The mean score for VABS domestic daily activities was 15 (SD 10). Univariate analyses also showed a significant association between the MACS and ABILHAND-Kids and domestic daily activities (explained variance 45% and 62%, respectively). GMFCS level, selective motor control, limb distribution, learning disability and age group were also associated with domestic daily activities in the univariate analyses (p < 0.1).
Table IV presents the multiple linear regression model for VABS domestic daily living skills. Adolescents with lower MACS levels and higher ABILHAND-Kids scores had higher scores for domestic daily activities. Explained variance increased from 45% (with MACS), to 59% (selective motor control added), 60% (learning disability added), to 68% (age group added; final model). Explained variance increased from 62% (with ABILHAND Kids), to 69% (selective motor control added), to 73% (age group added; final model).
| Table IV. Multiple linear regression model for VABS domestic daily living skills |
| Dependent variable: VABS domestic daily vliving skills | B | 95% CI | p | % explained variance |
| Model with MACS | | | | Adjusted R2 0.45 |
| Constant | 21 | 18.6 ; 23.4 | < 0.001 | |
| MACS | | | | |
| MACS I (ref. cat.) | 0 | | | |
| MACS II | –5.1 | –8.7 ; –1.4 | 0.007 | |
| MACS III | –11.6 | –17.1 ; –6 | < 0.001 | |
| MACS IV | –19.2 | –24.5 ; –13.9 | < 0.001 | |
| MACS V | –20.6 | –27.7 ; –13.5 | < 0.001 | 45 |
| MACS + other characteristics | | | Adjusted R2 0.68 |
| Constant | 19.4 | 16.7 ; 22 | < 0.001 | |
| MACS | | | | |
| MACS I (ref. cat.) | 0 | | | |
| MACS II | –0.8 | –3.8 ; 2.3 | 0.631 | |
| MACS III | –2.6 | –7.4 ; 2.3 | 0.299 | |
| MACS IV | –7.9 | –13.3 ; –2.6 | 0.004 | |
| MACS V | –4.8 | –11.9 ; 1.9 | 0.155 | 45 |
| Selective motor control | | | | |
| Good (ref. cat.) | 0 | | | |
| Moderate | –3.9 | –7.6 ; –0.3 | 0.036 | |
| Poor | –10.4 | –14.2 ; –6.6 | < 0.001 | |
| Learning disability | –5.2 | –8.9 ; –1.6 | 0.005 | |
| Age, years | | | | |
| 12 (ref. cat.) | 0 | | | |
| 14 | 1.6 | –1.5 ; 4.7 | 0.312 | |
| 16 | 6.6 | 3.6 ; 9.6 | < 0.001 | 23 |
| Model with ABILHAND-Kids | | | | Adjusted R2 0.62 |
| Constant | –4 | –7.3 ; –0.7 | 0.018 | |
| ABILHAND-Kids | 0.3 | 0.2 ; 0.3 | < 0.001 | 62 |
| ABILHAND-Kids + other characteristics | | Adjusted R2 0.73 |
| Constant | 4.5 | –0.5 ; 9.6 | 0.078 | |
| ABILHAND-Kids | 0.2 | 0.1 ; 0.2 | < 0.001 | 62 |
| Selective motor control | | | | |
| Good (ref. cat.) | 0 | | | |
| Moderate | –4.4 | –7.5 ; –1.3 | 0.006 | |
| Poor | –8.8 | –12.2 ; –5.4 | < 0.001 | |
| Age, years | | | | |
| 12 (ref. cat.) | 0 | | | |
| 14 | 1.2 | –1.6 ; 4 | 0.398 | |
| 16 | 4.7 | 2.1 ; 7.4 | 0.001 | 11 |
| CI: confidence interval; VABS: Vineland Adaptive Behavior Scales; MACS: Manual Ability Classification System; ref. cat.: reference category. |
Discussion
The objective of this study was to describe the manual ability of adolescents with CP and to investigate the relationship of manual ability to daily activities. Manual ability, measured with the MACS, was limited (MACS II–V) in 59% of the adolescents. Manual ability, measured with the ABILHAND-Kids, was lower in adolescents with GMFCS IV–V than in adolescents with GMFCS I, and adolescents with tetraplegia had significantly lower ABILHAND-Kids scores than adolescents with hemiplegia or diplegia. The MACS and the ABILHAND-Kids were both strongly associated with personal daily activities. They were also significantly, but less strongly, associated with domestic daily activities. The results showed that manual ability does indeed add information about the level of daily activities.
The percentage of adolescents with limitations in manual ability is in agreement with the results reported by Carnahan et al. (22), who found limited manual ability (MACS II–V) in 58% of a large group of children with CP. In another study, a lower percentage of limited manual ability, measured with the MACS (MACS II–V (19%)) was found in young adults with CP (12). However, this deviating percentage could be explained by the exclusion of adults with learning disabilities, which resulted in a study population with rather good gross motor function, manual ability and level of education (12). The MACS levels were distributed over several GMFCS levels. These results are similar to the results reported by Carnahan et al. (22), who also found a poor overall agreement between GMFCS and MACS levels. This is what we expected to find, and this was why we investigated the relationship between manual ability and daily activities in addition to the variables that are already known to be associated with daily activities.
It is remarkable that the simple 5-level MACS classification explains almost the same amount of variance of personal daily activities as the ABILHAND-Kids questionnaire, because the ABILHAND-Kids is expected to provide more details about manual ability than the rather gross 5 level classification of the MACS. However, ABILHAND-Kids showed a stronger association with domestic daily activities, compared with the MACS. The level of domestic daily activities is probably more strongly related to fine motor abilities, which can be measured more precisely with the ABILHAND-Kids.
Our results demonstrate the importance of manual ability in daily activities, even when GMFCS level was taken into account. They also showed the importance of independence in manual abilities (MACS level I–II) in order to achieve a high level of performance in daily activities. This is illustrated by the considerably lower level of performance in daily activities of adolescents with MACS levels III–V in the regression models. This is also in agreement with the results of earlier studies, in which the ABILHAND score was found to be an important predictor for limitations in daily activities (12) and a high correlation was found between the MACS level and personal daily activities (14). Based on these findings it is recommended that manual ability measurements should be included in the regular assessment of adolescents with CP, and that these measures of manual ability should be incorporated in the rehabilitation treatment. In daily practice the simple MACS classification would be sufficient to give an indication of limitations in personal daily activities, and the ABILHAND-Kids score could be an indicator of limitations in domestic daily activities.
Other factors, apart from manual ability, did not add very much more information about the level of personal daily activities. To a great extent the level of personal daily activities could be explained either by MACS level or ABILHAND-Kids score. However, selective motor control, learning disability and age group added 23% to the explained variance in the level of domestic daily activities. This indicates that not only disease characteristics, but also personal factors are important in the ability to perform domestic daily activities. Adolescents with poor selective motor control, adolescents with a learning disability, and younger adolescents are impaired in domestic daily activities. This is partially in agreement with the results of another study in which it was also found that younger age was associated with a lower level of domestic daily activities (2).
Further research, and especially studies based on longitudinal designs, should be carried out to determine the course of manual ability and to investigate the influence of the course of manual ability on the course of daily functioning in children with CP. The data that are obtained in such a study can then be used for the development of intervention programmes to improve daily activities in these children.
Conclusions are limited by the cross-sectional design of the study. As suggested above, it would be interesting to investigate the influence of an improvement or deterioration in manual ability on the performance of daily activities, and for this purpose a longitudinal study would be recommended. Furthermore, it should be noted that all the information presented in our study was collected from the parents, and not from the adolescents themselves. We chose this method because some of the adolescents had learning disabilities, but this limits the generalization of the results to the entire CP population. However, it is common clinical practice to gather information about the level of functioning of children from their parents. Another limitation of the study is that learning disability was based on type of school and not directly assessed.
In conclusion, the results of our study confirm that manual ability is limited in a large percentage of adolescents with CP, and that limitations in manual ability are strongly related to limitations in daily activities. The classification or assessment of manual ability should be a regular component of the physical examination in order to guide decisions concerning further treatment.
Acknowledgements
This research was performed as part of the PERRIN (Pediatric Rehabilitation Research in the Netherlands) research program, and the project was supported by the Netherlands Organisation for Health Research and Development (grant number 1435.0028).
References