OBJECTIVE: The aim of this study was to examine the self-reported health status of road traffic accident victims and the predictors of self-assessed recovery 1 year after major trauma in a French population.
DESIGN: A follow-up study.
METHODS: The cohort comprised 276 seriously injured victims of road traffic accidents, aged > 16 years from the Rhône administrative department, France. Victim characteristics at the time of the crash and self-reported health status 1 year after trauma were collected. Predictive factors for self-assessed recovery were examined using a Poisson regression approach.
RESULTS: The majority of victims were male (76%); most had severe injuries (76%), involving mainly the lower limbs and the head (68% and 55%, respectively). At 1-year follow-up, 80% reported being not fully recovered. Self-reported health status was not significantly associated with age, gender, being in employment, type of road user, or health status during the year preceding the accident, but rather with low socio-economic status, high injury severity, and presence of lower limb injury.
CONCLUSION: Care for subjects who are at high risk of not fully recovering (manual workers, the very seriously injured, and those with lower limb injury) needs to be extended and improved. Longer follow-up studies on the risk factors for not fully recovering are needed in order to reduce harmful consequences for victims.
Key words: follow-up studies; traffic crashes; wounds and injuries; outcome assessment; recovery of function; subjective health.
J Rehabil Med 2011; 43: 776–782
Correspondence address: Martine Hours; UMRESTTE IFSTTAR; 25 Avenue François Mitterrand, FR-69675 Bron Cedex, France. E-mail: martine.hours@ifsttar.fr
Submitted December 15, 2010; accepted June 17, 2011
INTRODUCTION
Previous studies have shown that road traffic accidents were the main cause of injury in most countries (1, 2) and that major trauma resulting from road traffic accidents may induce long-term negative effects, either objective or subjective, in victims’ lives, such as reduction in quality of life (2, 3), functional limitations (1, 4–6) and psychological problems (2, 7). Soberg et al. (5) found that the mental and general health of subjects with a New Injury Severity Score (NISS) >15 did not improve significantly between discharge home and 1 year after the crash. Studying quality of life after major trauma in subjects aged 18 years or over, Holbrook & Hoyt (2) reported that 169 out of 1048 subjects (16%) showed poor recovery at 12 months. Barnes & Thomas (3) reported that, 12 months after injury, 58% of hospitalized subjects had not fully recovered and still had pain, healing problems, and reduced leisure and work activity. Schluter & McClure (6) found that 119 (61%) of 195 subjects hospitalized for at least 6 days still had major functional limitations 12 months after the crash. Rates of non-return to work at 1-year follow-up varied between studies, from 10% to 36% (3, 8, 9). These studies assessed the consequences of trauma in terms of various outcomes: quality of life, post-traumatic stress disorder, and return to work. In France, since 2002, road safety has been 1 of the 3 most important government programmes. Although an unprecedented decrease in mortality has been obtained through police measures, such as increased controls on alcohol and speed, the decrease in severe casualties has not been as marked. Reducing the prevalence and impact of major trauma has therefore become a prime goal of the road safety authorities (10). Most victims of major trauma caused by road traffic accidents now have a good chance of survival, but there have been few French studies of late outcome in victims of road traffic accidents. Outside of France, studies have shown that adult victims of road traffic accidents experience far more severe health problems than do children, with significant impairment of well-being (11), and that various baseline factors, such as gender, age, type of injury and length of hospital stay, may predict long-term health status (1, 2, 4–6, 8). Such studies on French victims are still lacking.
ESPARR (Etude et Suivi d’une Population d’Accidentés de la Route dans le Rhône: Rhône area road traffic accident victim follow-up study) (12) is a study conducted in the Rhône administrative department of France. It involves a 5-year follow-up of a cohort of victims of road traffic accidents, and assesses the medical, physical, social, and psychological consequences of the crashes on the victims and their families.
The aim of the present study, which is part of ESPARR, was to investigate predictive factors of self-assessed health status in victims of major road trauma at 1-year’s follow-up in a French population.
METHODS
Participants
The ESPARR cohort is linked to the Rhône Road Trauma Registry, which records all road traffic accident casualties seeking medical care in public or private health facilities of the Rhône Département. Inclusion criteria are: having been in a road traffic accident, involving at least one mechanical means of transport, and occurring in the Rhône administrative area; having been admitted to one of the area’s hospital emergency departments; having survived the crash until hospital admission; being resident in the same area (to facilitate follow-up).
In addition, the present study included only seriously-to-critically injured subjects: i.e. with at least one injury scored ≥ 3 on the Abbreviated Injury Severity Scale (AIS) (13). The most severe injury was described by its maximum injury severity score (M-AIS). Also, because recovery processes and assessment tools differ between children and adults, participants had to be aged 16 years or over, and they (or their parents or legal representatives) had to give informed consent to the follow-up and complete a self-administered questionnaire 1 year after the crash.
Further details of patient contact, recruitment and interview for collection of baseline and clinical characteristics have been published previously (12).
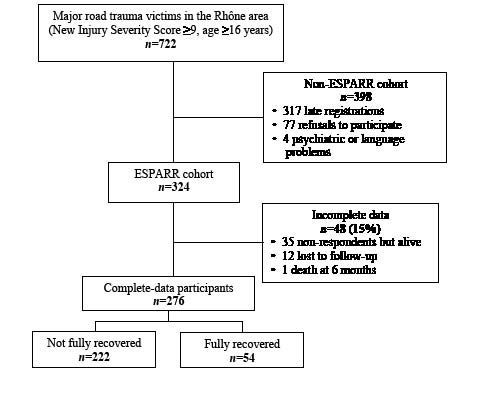
From October 2004 to July 2006, the Rhône Road Trauma Registry recorded 722 victims. Of these, 324 met the ESPARR inclusion criteria and were initially included; the participants (or their representatives) were interviewed as soon as possible after the crash (median delay: 4 days; 1st and 3rd quartiles: 1 and 10.5 days). The subsequent withdrawal of 48 victims resulted in 276 subjects being included in the final analyses (Fig. 1).
Fig. 1. Process of patient inclusion. ESPARR: Etude et Suivi d’une Population d’Accidentés de la Route dans le Rhône.
Study data and measurement tools
Two sources of data were used for the present study: the ESPARR cohort data, and data from the Rhône Road Trauma Registry.
Patient characteristics data collected during the initial interview:
• Demographic characteristics: age at crash, gender.
• Socio-economic status: this variable is derived from the “French occupational and social categories, level 1, 8 categories” (14); it was then regrouped into 5 categories according to their frequency.
• Current employment: this variable was divided into 2 categories according to their employment at the time of the accident. Participants were considered to be “in employment” if they were students or had a regular job at baseline.
• Type of road user: this variable was divided into 4 categories according to their mode of transport.
Medical data:
• Comorbidity collected during the initial interview: subjects were considered as having a comorbidity if, at the time of the crash, they had at least one chronic disease (excluding vision problems) listed in the French Ministry of Transport decree of December 21, 2005 (15).
• Initial injury report: were collected from the medical records and coded by a trained physician:
• Injury severity: as measured by the AIS, which standardizes injury data and scores lesions from 1 (minor) to 6 (fatal); M-AIS, the score of the most severe injury; and NISS (16), sum of the squares of AIS scores for the 3 most severe injuries, regardless of body region.
• Type of injury: injuries were also classified by body part into subgroups according to their injuries (head, face, neck, spine, abdomen, upper limbs, and lower limbs). Thoracic injuries were divided into 2 subgroups: “severe thoracic injury” for thoracic M-AIS from 3 to 5, and “absence of severe thoracic injury” for no thoracic involvement or thoracic M-AIS of 1 or 2.
Self-reported data: 1 year after the crash, a self-administered questionnaire assessed the health, social, emotional, and financial status of each participant (17). These data were collected by questionnaires, either sent by regular post followed by reminder telephone calls or completed during a face-to-face interview.
• Self-assessed recovery: a standard single-item self-assessed recovery measure was used: “How would you describe your health status today?”, with 4 response options (“Fully recovered”, “Improved but not recovered”, “Stabilized” or “Deteriorated”), dichotomized for analysis as “Fully recovered” vs “ Not fully recovered”, the latter combining all 3 remaining response options.
• Quality of life: quality of life was evaluated with a standard instrument (the World Health Organization Quality of Life Questionnaire-Short Form (WHOQOL-BREF)), which is an abbreviated version (26 items) of the WHOQOL (100 items), and covers 4 domains: physical health (7 items), psychological health (6 items), social relationships (3 items), environment (8 items) and 2 global health-related quality-of-life items assessing overall satisfaction with life and general sense of personal well-being. Responses to each item were coded from 1 to 5, summed, and transformed to a scale from 0 (worst health-related quality of life) to 100 (best health-related quality of life) (18).
Statistical analysis
In order to assess representativeness, our population was compared with a reference group of major road traffic accident trauma victims recorded in the Rhône Road Trauma Registry during the same period (October 2004 to July 2006), i.e Non-ESPARR victims and non-respondent ESPARR cohort (Fig. 1). Nominal variables were compared using χ2 test or Fisher’s exact test, and quantitative variables by Student’s t-test. The correlation between responses to our subjective health question and to the overall health question in the WHOQOL-BREF (a validated instrument used to assess health-related quality of life) was assessed with Spearman’s rho.
Predictive factors for being not fully recovered 1 year after the crash were sought among the parameters collected at baseline. One of the advantages of cohort studies is that relative risk, instead of odds ratios, which are only approximations of the real relative risk, can be calculated directly; furthermore, odds ratios can be used as an approximation of relative risk only if the prevalence of the health problem in question in the study population is very low, which was not the case in the present study. A Poisson regression approach was used for modelling (19, 20) to estimate relative risk directly (20, 21). As the Poisson regression was applied to binomial data, a sandwich estimation of the variance of the estimated relative risk was used (20). In the univariate analysis, the associations between subject characteristics, injury severity and the probability of poor subjective health were assessed with the χ2 test. For each characteristic, the association was quantified by a risk ratio. A 95% confidence interval (95% CI) was given for each relative risk.
Variables that were significantly associated with subjective health status at the 20% level on univariate analysis were included in the multivariate analysis, after checking for collinearity between explanatory variables. Gender and age, considered as adjustment variables, were included in the multivariate analysis regardless of their significance level. Stepwise selection with backward elimination of subjective health status predictors was applied, with p > 0.05 for exclusion. Confounding factors were checked at each stage of model construction.
Statistical Analysis System software, version 9.1 for Windows (SAS Institute, Cary, NC, USA) was used for all analyses.
RESULTS
Comparison between study sample and reference group
Overall, the study sample did not differ significantly from the reference group concerning gender or severity of injury. However, the mean age of the study population was significantly lower than that of the reference group (37.2 years, standard deviation (SD) 17.0, vs 41.4 years, SD 20.6; p < 0.01) and the study sample included more car drivers but fewer pedestrians, inline-skate/scooter users and passengers than the reference group (p < 0.01) (Table I).
| Table I. Description of the study population and comparison of characteristics with the reference group |
| Characteristics | Study sample (n = 276) n (%) | Reference group (n = 446) n (%) | p-value |
| Sex | | | 0.57 |
| Male | 210 (38.8) | 331 (61.2) | |
| Female | 66 (36.5) | 115 (63.5) | |
| Type of road user | | | < 0.01 |
| Pedestrian, inline-skate/scooter user, passenger | 71 (30.1) | 165 (69.9) | |
| Cyclist | 33 (38.8) | 52 (61.2) | |
| Motorized 2-wheel/ quad-bike driver | 104 (42.8) | 139 (57.2) | |
| Car driver | 67 (46.2) | 78 (53.8) | |
| Not known | 1 (7.7) | 12 (92.3) | |
| Maximum Abbreviated Injury Scale | | | 0.07 |
| 3 | 214 (39.8) | 324 (60.2) | |
| 4 | 46 (30.7) | 104 (69.3) | |
| 5 | 16 (47.1) | 18 (52.9) | |
Description of the study sample
Three out of 4 victims (210/276; 76%) were male. The majority (76%) had M-AIS = 3 injuries. The main injury sites were the lower limbs and head (68% and 55%, respectively).
For the question “How would you describe your health status today?”, only 54 subjects (19.6%) responded “Fully recovered”, the vast majority of respondents (222/276; 80.4%) reported being not fully recovered 1 year after trauma (139 subjects (50.4%) responded as “Improved but not recovered”, 46 subjects (16.7%) as “Stabilized” and 37 subjects (13.4%) as “Deteriorated”). Blue-collar workers tended to have a higher probability of not fully recovered than white-collar workers (Table II). Overall injury severity was significantly linked to the percentage of victims reporting not fully recovered at 1-year follow-up, which increased with degree of severity. The proportion of subjects reporting full recovery was lower in those with NISS ≥ 16 than with NISS between 9 and 15 (15% vs 27%; p < 0.05) (Table III).
| Table II. Estimations of the probabilities of not fully recovered vs fully recovered at 1-year follow-up after severe injury following a road traffic accident according to victims’ characteristics. Results of univariate analyses |
| Victims’ characteristics | Fully recovered (n = 54) n (%) | Not fully recovered (n = 222) n (%) | Relative risk (95% confidence interval) |
| Age at crash | | | |
| 16–24 years | 26 (27.1) | 70 (72.9) | 1* |
| 25–44 years | 15 (16.1) | 77 (83.8) | 1.2 (1.0–1.3) |
| 45–64 years | 10 (15.4) | 55 (84.6) | 1.2 (1.0–1.4) |
| ≥ 65 years | 3 (13.6) | 19 (86.4) | 1.2 (1.0–1.5) |
| Sex | | | |
| Male | 43 (20.5) | 167 (79.5) | 1 |
| Female | 11 (16.7) | 55 (83.3) | 1.1 (0.9–1.2) |
| Socio-economic status | | | |
| White-collar worker | 20 (18.9) | 86 (81.1) | 1** |
| Intermediate-level employee | 12 (24.5) | 37 (75.5) | 0.9 (0.7–1.1) |
| Farmer, craftsman, shopkeeper | 4 (20.0) | 16 (80.0) | 1.0 (0.7–1.3) |
| Blue-collar worker | 4 (7.4) | 50 (92.6) | 1.1 (1.0–1.3) |
| Student, housewife | 14 (29.8) | 33 (70.2) | 0.9 (0.7–1.1) |
| Comorbidity | | | |
| No | 39 (20.0) | 156 (80.0) | 1 |
| Yes | 15 (18.5) | 66 (81.5) | 1.0 (0.9–1.2) |
| In employment at time of crash | | | |
| No | 8 (12.9) | 54 (87.1) | 1* |
| Yes | 46 (21.5) | 168 (78.5) | 0.9 (0.8–1.0) |
| Type of road user | | | |
| Pedestrian, inline-skate/scooter user, passenger | 8 (11.3) | 63 (88.7) | 1* |
| Cyclist | 6 (18.2) | 27 (81.8) | 0.9 (0.8–1.1) |
| Motorized 2-wheel/quad-bike driver | 26 (25.0) | 78 (75.0) | 0.8 (0.7–1.0) |
| Car driver | 14 (20.9) | 53 (79.1) | 0.9 (0.8–1.0) |
| *0.05 < p < 0.20;**p < 0.05 . |
| Table III. Estimations of the risk of being not fully recovered vs fully recovered at 1-year follow-up after severe injury following a road traffic accident, according to injury severity and lesions. Results of univariate analyses |
| Injury characteristics | Fully recovered (n = 54) n (%) | Not fully recovered (n = 222) n (%) | Relative risk (95% CI) |
| Overall injury severity | | | |
| NISS 9–15 | 27 (26.7) | 74 (73.3) | 1** |
| NISS ≥16 | 27 (15.4) | 148 (84.6) | 1.2 (1.0–1.3) |
| Head | | | |
| No lesion | 27 (22.1) | 95 (77.9) | 1 |
| AIS 1–2 | 15 (16.1) | 78 (83.9) | 1.1 (0.9–1.2) |
| AIS 3–5 | 12 (19.7) | 49 (80.3) | 1.0 (0.9–1.2) |
| Neck | | | |
| No lesion | 53 (19.6) | 218 (80.4) | 1 |
| AIS 1 or 2 | 1 (20.0) | 4 (80.0) | 1.0 (0.6–1.5) |
| Face | | | |
| No lesion | 39 (20.1) | 155 (79.9) | 1 |
| Lesion | 15 (18.3) | 67 (81.7) | 1.0 (0.9–1.2) |
| Spine | | | |
| No lesion | 43 (20.7) | 165 (79.3) | 1 |
| Lesion | 11 (16.8) | 57 (83.2) | 1.1 (0.9–1.2) |
| Severe thoracic injury | | | |
| No | 39 (20.2) | 154 (79.8) | 1 |
| Yes | 15 (18.1) | 68 (81.9) | 1.0 (0.9–1.2) |
| Abdomen | | | |
| No lesion | 47 (20.7) | 180 (79.3) | 1 |
| Lesion | 7 (14.3) | 42 (85.7) | 1.1 (0.9–1.2) |
| Upper limbs | | | |
| No lesion | 28 (22.3) | 110 (79.7) | 1 |
| AIS 1 or 2 | 13 (16.9) | 64 (83.1) | 1.0 (0.9–1.2) |
| AIS 3–5 | 13 (21.3) | 48 (78.7) | 1.0 (0.8–1.2) |
| Lower limbs | | | |
| No lesion | 21 (24.1) | 66 (75.9) | 1* |
| AIS 1 or 2 | 13 (25.0) | 39 (75.0) | 1.0 (0.8–1.2) |
| AIS 3–5 | 20 (14.6) | 117 (85.4) | 1.1 (1.0–1.3) |
| *0.05 < p < 0.2; **p < 0.05. CI: confidence interval; NISS: New Injury Severity Score; AIS: Abbreviated Injury Scale. |
The two global WHOQOL-BREF items assessing overall satisfaction with life and general sense of personal well-being showed that 51.1% (141 persons) of the population rated their quality of life as good or very good, and 42.8% (118 persons) were satisfied or very satisfied with their health status. A significant correlation was found between subjective health status and global health satisfaction on the WHOQOL-BREF (R = 0.49, p < 0.001). The group of victims reporting being fully recovered at 1-year follow-up had better scores in all quality of life domains than those reporting being not fully recovered. However, the difference is only significant for the physical and psychological domain (p < 0.001) (Table IV).
| Table IV. Global health-related quality of life and satisfaction, World Health Organization Quality of Life Questionnaire-Short Form (WHOQOL-BREF) scores with self-reported recovery subgroup |
| WHOQOL-BREF | Fully recovered (n = 54) n (%) | | Not fully recovered (n = 222) n (%) | Total (n = 276) |
| |
| How would you rate your quality of life? | |
| Very poor/poor | 3 (7.5) | | 37 (92.5) | 40 |
| Neither poor nor good | 7 (7.6) | | 85 (92.4) | 92 |
| Good/very good | 44 (31.2) | | 97 (68.8) | 141 |
| How satisfied are you with your health? | |
| Very dissatisfied/dissatisfied | 2 (2.0) | | 97 (98.0) | 99 |
| Neither satisfied nor dissatisfied | 5 (8.9) | | 51 (91.1) | 56 |
| Satisfied/very satisfied | 47 (39.8) | | 71 (60.2) | 118 |
| WHOQOL-BREF scores, mean (SD) | | | | |
| Physical area* | 83.3 (13.2) | | 59.7 (21.5) | 64.3 (22.2) |
| Psychological area* | 71.3 (13.9) | | 60.2 (19.3) | 62.4 (18.9) |
| Social relationships area | 77.8 (18.3) | | 67.9 (19.1) | 69.8 (19.3) |
| Environmental area | 74.5 (15.1) | | 63.0 (17.3) | 65.3 (17.5) |
| *Test of difference between the fully recovered and not fully recovered group (p < 0.001). SD: standard deviation. |
Predictive factors for poor subjective health at 1-year follow-up
After adjustment for the baseline characteristics, subjective health status was not found to be associated with age, gender, being in employment at the time of the crash, type of road user, or health status during the year before the crash. However, associations were found with socio-economic status, overall severity, and lower limb injury. Regarding socio-economic status, multivariate analysis showed that blue-collar workers had a 20% increased risk of poor subjective health compared with white-collar workers (p = 0.02). Similarly elevated risk was also observed for subjects with NISS ≥ 16 compared with NISS between 9 and 15 (p < 0.01); subjects with severe lower limb injury (M-AIS = 3–5) were more at risk of poor subjective health than those without such injury (Table V).
| Table V. Factors related to be not fully recovered 1 year after road traffic accident in ESPARR cohort subjects with major trauma (NISS ≥ 9). Results of the multivariate analysis (n = 275) |
| Factors | Adjusted relative risk (95% CI) | p-value |
| NISS ≥ 16 vs NISS 9, 15 | 1.2 (1.1–1.4) | < 0.01 |
| Lower limbs | | 0.03 |
| No lesion | 1 | |
| AIS 1 or 2 | 1.0 (0.8–1.2) | |
| AIS 3–5 | 1.2 (1.0–1.3) | |
| Socio-economic status | | 0.04 |
| White-collar worker | 1 | |
| Intermediate-level employee | 0.9 (0.8–1.1) | |
| Farmer, craftsman, shopkeeper | 1.0 (0.8–1.3) | |
| Blue-collar worker | 1.2 (1.0–1.3) | |
| Student, housewife | 0.9 (0.7–1.2) | |
| Age at crash | | 0.38 |
| 16–24 years | 1 | |
| 25–44 years | 1.2 (1.0–1.3) | |
| 45–64 years | 1.2 (1.0–1.3) | |
| ≥ 65 years | 1.2 (0.9–1.4) | |
| Sex | | |
| Female vs male | 1.1 (0.9–1.3) | 0.19 |
| NISS: New Injury Severity Score; AIS: Abbreviated Injury Scale; CI: confidence interval; ESPARR: Etude et Suivi d’une Population d’Accidentés de la Route dans le Rhône. |
DISCUSSION
There have been only a few studies of health status after serious road traffic accidents in France. The present study examined the subjective health status of a population of road traffic accident victims with NISS ≥ 9 and identified the main predictive factors for being not fully recovered 1 year after the crash. Regarding the main outcome measure, self-reported health status 1 year after the accident was “fully recovered” in only 20% of the study sample. Self-reported health status was not significantly associated with age, gender, being in employment, type of road user, or health status during the year preceding the accident, but rather with low socio-economic status, high injury severity, and presence of lower limb injury.
Some features of the study population allow meaningful comparison with previous reports. The predominance of males (76% in the study sample, 74% in the reference group) is similar to that reported by Mayou & Bryant (7) in the Oxford study on adult victims followed up for 1 year. The mean age (37 years) was also similar to that of the major trauma population, aged ≥ 16 years, in Holtslag et al. and other reports (4, 7, 9, 22), in which the mean age of adult victims ranged between 30 and 40 years. Lower limb injuries predominated in the present data, as they did in another study that reported 58% victims with lower limb injury (3).
As described previously, severity and type of injury were found to be related to being not fully recovered. In several previous studies (2, 5–8), severe injury led to serious health impairment and was a predictive factor for long-term health status (5, 6, 8); for example, Mayou & Bryant (7) reported that victims with severe injuries had the most severe physical consequences. The present study found a significant difference in overall recovery between victims with NISS ≥ 16 and with NISS ranging between 9 and 15. Regarding type of injury, our data confirm the association between lower limb injury and being not fully recovered after major trauma (6, 22, 23). Other investigations reported associations between type of injury (e.g. spinal) and functional outcome (1, 4); the present analysis failed to find any significant association between health status at 1 year and spinal injury, but power was insufficient in this regard because few subjects had very severe lesions involving the spinal cord. Self-assessment of well-being is likely to underestimate the severity of the real outcome, as some victims, particularly those who sustained traumatic brain injury, sometimes experienced anosognosia, which may explain why in the present study, contrary to Holtslag et al.’s study (4), traumatic brain injury was not found to be a predictive factor for not fully recovering. The medical literature does not mention relationships between socio-economic status or type of road user and subjective health status 1 year after major road trauma. When adjusted for the global severity of the injury, blue-collar workers in the present study were 20% more likely to report not having fully recovered at 1 year than white-collar workers. Subjective poor health recovery is related to pain (24). Whereas blue collar workers do not have more limb injuries than other socioeconomic categories, it is possible that pain is more intolerable for people who have a physically demanding job and thus they are prevented from returning to work, which may explain why more blue-collar workers are not fully recovered. However, in a previous analysis (25), which investigated the predictors of return to work, the results show that there was no significant difference in the return to work between blue-collar workers and others when the severity was taken into account. On the other hand, Schreuder et al. (26) did not find differences in job demands and health complaints in white- and blue-collar workers. Thus, we cannot establish whether blue-collar workers have an objective difference in their health status from others.
The present analysis showed no significant associations between the subjective health status at one year and gender, age, type of road user, being in employment at the time of the crash, or presence of comorbidity. Nevertheless, we decided to introduce the first two factors as adjustment variables in the multivariate analysis, whatever their significance level. Gender, although correlating with health status in several studies (1, 2, 8), was not highlighted in the present study or other studies (5, 6). The relationship between age and long-term health status after a crash has been studied previously (1, 4–6, 8). Schluter & McClure (6) reported that age was a predictive factor for functional impairment at 12 months. A study of functional capacity after trauma in victims aged ≥ 15 years (1) showed that age was significantly related to functional impairment at both 12 and 24 months. These results oriented our hypothesis that age at the time of the accident might be a predictive factor for health status; however, this failed to emerge in the present logistic regression model after adjustment for the other factors.
Self-reported health has often been studied in major trauma populations, using general questions from the EUROQOL-5D, Short Form-36 Health Survey (3, 5, 7, 9, 22), Sickness Impact Profile (9, 23), or Quality of Well-Being Scale (2), assessing general and specific dimensions of health status. In most of the above-cited articles, health status was defined as “good” when victims reported no problem in mental or physical health. The present study agrees with several previous publications (7, 11) as to the choice of subjective assessment of outcome at 1 year. The correlation between objective and subjective health has been investigated and highlighted in the literature, particularly in populations with health problems (27–30). Subjective health has been correlated with mortality. These results suggest that subjective health measurement validly reflects significant implications for healthcare.
In our study, the majority of victims who reported a full recovery (44/54, 81.5%) rated a better quality of life than those who reported a not full recovery (97/222, 43.7%). The formulation used to describe subjective health gave more specific information than the overall health item of the WHOQOL-BREF: with 4 modalities (“Fully recovered”, “Improved but not recovered”, “Stabilized” and “Deteriorated”), the present self-assessment reflected the subjective health status of the victim related to the crash; in contrast, the WHOQOL-BREF subjective health item fails to specify whether any negative perception is related to the crash. The objective of the present study was not to analyse the victims’ quality of life, but only their assessment of their health one year after the crash. We therefore preferred to use our own item, in order to have a good level of specific information. Furthermore, the correlation between our own item and that of the WHOQOL-BREF was satisfactory.
By comparing our results about the WHOQOL-BREF with the results of a study in the general French population (31), we found that our severely injured patients had lower scores of quality of life than the general French population. However, the study in the general French population investigated only 3 of 4 domains of the WHOQOL-BREF and the question related to the WHOQOL-BREF was changed slightly in that general French study. It should be noted, however, that the French general population studied was older and had a greater proportion of women than our population study. Quality of life is very dependent on age and gender: women are more likely to have a less good quality of life than men; furthermore, quality of life decreases with age. Thus, the strong decrease in the quality of life of our population (which is composed of numerous young men) reveals the strong impact of the accident on quality of life, as reported by Baumann et al. (31).
There were differences in the literature regarding the tools used to assess type and severity of injury. Although introduced in 1997 to improve outcome prediction in trauma victims, the NISS is, as yet, rarely used (5). Even so, certain studies of trauma victims have demonstrated that the NISS is better able to predict functional outcome (32), probability of survival (33) and need for intensive care (34) than the Injury Severity Score. We therefore predict that the NISS might be adopted as the new “gold standard” for severity scoring.
The present report concerns a part of a cohort study with binary outcomes in which the outcome event was common (80% self-reported not fully recovered). Thus it was preferable to estimate relative risk (20, 21) than to calculate odds ratios, which are only an approximation of the relative risks.
The major importance of the present study is that it is one of the first to report on long-term outcome in French victims of road traffic accidents. Other strong points are the prospective design and the complete baseline data provided by the Rhône Road Trauma Registry, which, with appropriate corrections, enable reliable extrapolation of the results to the total recorded casualty population and thus a non-negligible improvement in our knowledge of outcome of major road trauma in the Rhône Département.
There were limitations inherent in these analyses. Firstly, the conditions of collecting the information were not strictly the same for all victims. The slight difference in the result for the telephone interview is probably explained by the fact that more fully recovered people do not reply to the postal questionnaire or to the medical visit invitation than not fully recovered people. If there is a bias, it is more likely to be related to the non-responses than to the questions themselves. However, the non-response is quite low (15%) (Fig. 1) and the two groups are not, in fact, different except on age (which is taken into account in the analysis). Secondly, some studies in the literature show that claiming compensation is a factor associated with health status after trauma (35, 36). A bias in self-report of recovery can be caused by the process of compensation in our population. The majority of the study population had not received compensation by the time of the 1 year follow-up (186/276, 67.4%). We made a comparison between the victims reported as fully recovered and those reported as not fully recovered concerning having received compensation or not. The difference was not significant (p = 0.899). Thus, it is unlikely that this introduced a bias in the self-report of recovery in our population. Thirdly, the metrological properties (accuracy, validity, reproducibility) of the whole ESPARR questionnaire are not controlled. However, the ESPARR questionnaire itself is built as often as possible using validated scales or indicators: the main variable (fully recovered/not fully recovered) is highly correlated with the second question of the WHOQOL-BREF (health satisfactory): the WHOQOL-BREF itself is a validated scale; SEC is an usual French socioeconomic scale; injuries were reported by medical staff and coded by the trained physician of the Rhone Registry (who were blind to the ESPARR status).
In conclusion, one year after a serious road traffic accident, the majority of victims still have problems with their health status. This study indicated the need to extend follow-up and even medical care beyond one year after injury in some subgroups. More specifically, it seems necessary to enhance and extend care in subjects at high risk of not fully recovering, such as manual workers, very seriously injured victims (NISS ≥16) and those with lower limb injuries. Moreover, according to its initial intent, the present follow-up study should be extended for several years in order to assess further the long-term consequences of road traffic accident injuries and o expand our knowledge of factors linked with better recovery.
ACKNOWLEDGEMENTS
The authors are grateful to the victims for their cooperation in data collection. The authors would like to thank all those who assisted in carrying out this study: Nadia Baguena, Jean Yves Bar, Amélie Boulanger, Elodie Paquelet, Stuart Nash, Véronique Sotton for collecting the data, Irène Vergnes for organizing the databases; Anne-Marie Bigot, Nathalie Demangel, Geneviève Boissier for subject database management; Blandine Gadegbeku and The Association for the Rhône Road Trauma Registry (ARVAC) for their help in collecting and providing medical data; the Scientific Committee (Daniel Floret, François Chapuis, Jean Michel Mazaux, Jean Louis Martin, Jacques Gaucher); all the hospital staff who accepted the interviewers’ presence and referred victims; and the SAMU team who reported their daily emergency interventions.
Special thanks to Mr Jean-Louis Martin and Dr Muriel Rabilloud for data processing and statistical analysis advice, to M. Jean Iwaz for comments and manuscript editing, and to Iain McGill for English translation.
We acknowledge funding from the French Ministry of Equipment, Transport, Housing, Tourism and Sea (Program Predit 3 “New Knowledge in the Field of Road Safety”: N° SU0400066) and from the French Ministry of Health (Program PHRC 2003: PHRC-N03 and PHRC 2005: PHRC- N051).
The individual authors have no competing interests to declare.
REFERENCES