Helene L. Soberg, PhD1, Cecilie Roe, MD, PhD1,2, Audny Anke, MD, PhD3,4, Juan Carlos Arango-Lasprilla, PhD5,Toril Skandsen, MD, PhD6,7, Unni Sveen, PhD1,8, Nicole von Steinbüchel, PhD9 and Nada Andelic, MD, PhD1
From the 1Department of Physical Medicine and Rehabilitation, Oslo University Hospital, Ulleval, 2Faculty of Medicine, University of Oslo, Oslo, 3Department of Rehabilitation, University Hospital of North Norway, 4Faculty of Health Sciences, Institute of Clinical Medicine, University of Tromso, Tromso, Norway, 5IKERBASQUE, Basque Foundation for Science, University of Deusto Bilbao, Bilbao, Spain, 6Department of Neuroscience, Faculty of Medicine, Norwegian University of Science and Technology (NTNU), 7Department of Physical Medicine and Rehabilitation, St Olavs Hospital, Trondheim University Hospital, Trondheim, 8Oslo and Akershus University College of Applied Sciences, Oslo, Norway and 9Department of Medical Psychology and Medical Sociology, Georg-August-University, Goettingen, Germany
OBJECTIVE: To assess health-related quality of life in individuals with severe traumatic brain injury at 12 months post-injury, applying the Quality of Life after Brain Injury (QOLIBRI) instrument, and to study the relationship between injury-related factors, post-injury functioning and health-related quality of life.
Design/subjects: The study is part of a prospective, Norwegian multicentre study of adults (≥ 16 years old) with severe traumatic brain injury, as defined by a Glasgow Coma Scale score of 3–8 during the first 24 h post-injury. A total of 126 patients were included.
METHODS: Socio-demographic data and injury severity variables were collected. Functioning at 3 and 12 months was assessed with the Glasgow Outcome Scale Extended (GOSE), the Functional Independence Measure (FIM), the Rivermead Post-concussion Questionnaire (RPQ), and the Hospital Anxiety and Depression Scale (HADS). Hierarchical regression analysis was applied.
RESULTS: Mean QOLIBRI score was 68.5 (standard deviation = 18.8). Predictors of the QOLIBRI in the final regression model were: employment status (p = 0.05), GOSE (p = 0.05), RPQ (p < 0.001) and HADS (p < 0.001). The adjusted R2 showed that the model explained 64.0% of the variance in the QOLIBRI score.
CONCLUSION: Symptom pressure and global functioning in the sub-acute phase of traumatic brain injury and psychological distress in the post-acute phase are important for health-related quality of life at 12 months post-injury. These domains should be the focus in rehabilitation aiming to improve health-related quality of life in patients with severe traumatic brain injury.
Key words: traumatic brain injury; quality of life; depression; rehabilitation; outcome assessment.
J Rehabil Med 2013; 45: 763–769
Correspondence address: Helene Soberg, Department of Physical Medicine and Rehabilitation, Ulleval University Hospital, NO-0407 Oslo, Norway. E-mail: h.l.soberg@medisin.uio.no, helene.soberg@ulleval.no
Accepted Mars 12, 2013
INTRODUCTION
Traumatic brain injury (TBI) is a leading cause of death and disability around the world (1). Approximately 10 million people experience TBI every year. TBI is the most common cause of disability in people under 40 years of age. Those who survive TBI often face lifelong challenges and reduced health-related quality of life (HRQL) (2).
Individuals who have sustained a TBI often experience cognitive deficits (2), physical problems (3) and emotional issues (4). The cognitive changes include deficits in executive functioning (5), attention and information processing (6), memory and learning (7) and communication (8). Physical sequelae may include spasticity, mobility problems and chronic pain (9, 10). In addition, patients report long-term emotional problems, such as anxiety and depression (4). Many survivors find themselves unable to return to their pre-injury lives, causing feelings of loss of “self” (11) and reduced quality of life (12).
HRQL is considered an important outcome when describing problems in health and functioning in individuals with severe TBI (13, 14). The concept comprises a person’s sense of well-being and satisfaction with life in terms of physical, psychological and social functioning; perceptions of self-efficacy; independence; social support; and self-concept (13, 15). In rehabilitation, the restoration of HRQL represents a complex challenge, both for individuals with TBI and for rehabilitation professionals.
Reduced HRQL has been identified in individuals with TBI compared with healthy controls or reference populations (12, 15, 16). Several factors associated with poorer HRQL in TBI populations have been reported, such as racial/ethnic minority status (17), female gender (18) or TBI symptomatology (12, 19). The literature has shown diverging results concerning the relationship between injury severity and HRQL. Some studies have reported lower HRQL for individuals with more severe TBI; other studies have reported lower HRQL for individuals with mild TBI; in other studies, no difference with respect to injury severity was found (3, 12, 15).
The assessment of HRQL after TBI is performed primarily by global measures of well-being and generic measures of health and functioning, such as the Medical Outcome Study’s Short Form-36 (SF-36) and EuroQol-5D (20). However, generic measures may not capture the particular problems of TBI, and the need for condition-specific HRQL instruments in TBI is emphasized (13, 21). Recently, the Quality of Life after Brain Injury (QOLIBRI), a condition-specific instrument for measuring HRQL after TBI, was developed in an international collaborative process (22–24). The QOLIBRI captures the individuals’ well-being and satisfaction with their functioning and self, and provides a more precise measure of the individual’s experience of living with a TBI than generic measures. The development process of QOLIBRI has been thorough, and it has been validated in 2,000 people after TBI of different severities (23, 24). To our knowledge, the QOLIBRI has not yet been applied to a population consisting of individuals with severe TBI 1 year after injury. The aim of this study was to assess HRQL in individuals with severe TBI at 12 months post-injury by applying the QOLIBRI. We also aimed to study the relationship between injury-related factors, post-injury functioning and symptoms at 3 and 12 months, and HRQL at 12 months. Based on previous research, we hypothesized that symptom pressure would be negatively associated with HRQL, but that there would not be a distinct association between TBI severity and HRQL over time.
METHODS
Study design
The present study is part of a larger prospective, population-based Norwegian multicentre study of adults with severe TBI who were admitted to neurosurgical departments between 2009 and 2011. Patients were included from the trauma centres in the 4 health regions in Norway: University Hospital of North Norway, representing the northern region; St Olavs Hospital, representing the central region; Haukeland University Hospital, representing the western region; and Oslo University Hospital, representing the southeastern region of Norway.
Inclusion criteria and procedure
The enrolment of patients and the collection of data in the acute phase were performed separately at the 4 university hospitals. The electronic patient register was searched weekly to identify all patients who had been admitted to the trauma referral centres for acute severe TBI.
Inclusion criteria stated that patients must be adults (age 16 years or older) and admitted within 72 h post-injury. The participants were required to meet the definition of severe TBI by displaying an un-sedated Glasgow Coma Scale (GCS) score of 3–8 during the first 24 h. Exclusion criteria were: chronic subdural haematomas; pre-injury cognitive disability interfering with the assessments; severe psychiatric diseases; and drug abuse.
Participants
Between 2009 and 2011, 278 patients meeting the inclusion criteria were admitted to the 4 regional trauma hospitals. Of this initial cohort, 80 patients (28.8%) died during their stay in intensive care, and 20 patients (7%) died before the 12-month follow-up. For the present study, 162 patients were available for the 12-month follow-up, and QOLIBRI data were collected for 126 patients (77.8%). Data at 3 and 12 months were collected when the patients were admitted to the rehabilitation departments, or by telephone interview if they were discharged home. Because of time restrictions, we did not collect QOLIBRI data when we interviewed patients by telephone. The patient flow is detailed in Fig. 1. Seventy-eight percent of the 126 participants were men, and the mean age was 38.8 years (SD 17.8). There were no statistical differences in demographics and injury severity characteristics between the QOLIBRI responders and the other surviving participants who were non-responders on the QOLIBRI at 12 months. Descriptive statistics for the participants are shown in Table I.
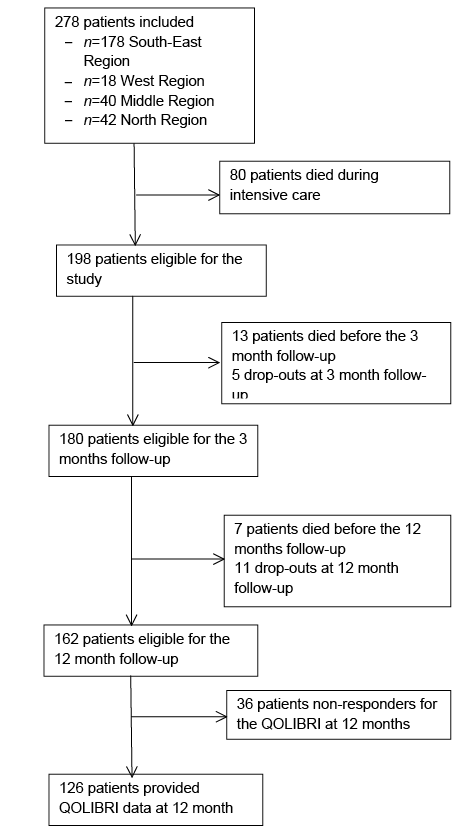
Fig. 1. Patient inclusion. QOLIBRI: Quality of Life after Brain Injury.
|
Table I. Demographics at the time of injury of the participants (n=126) |
|
|
Demographic information |
|
|
Age, years, mean (SD) |
38.9 (17.8) |
|
Gender, men, n (%) |
98 (77.8) |
|
Marital status, n (%) Married/living with a partner Single/divorced/cohabitating Unknown |
56 (44.4) 69 (54.8) 1 (0.8) |
|
Education, n (%) Low High |
82 (65.1) 44 (34.9) |
|
Pre-injury employment status, n (%) Employed/student Sick-leave/vocational or medical rehabilitation/social security support/disability pension Unemployed Retired/homemaker Unknown |
90 (71.5) 16 (12.8) 7 (5.6) 12 (9.5) 1 (0.8) |
|
SD: standard deviation. |
|
Data collection
During the acute phase, data were drawn from medical records from the patients’ stay in the neurointensive care units/neurosurgical departments. Data collected included demographic information, cause of injury (transport accidents, falls, assaults, others/sport injuries), GCS score, Abbreviated Injury Scale (AIS) score of the TBI (AIS head), Injury Severity Score (ISS), length of post-traumatic amnesia (PTA), and Rotterdam CT score.
Demographic variables collected included sex, age, and marital status, which was categorized into married or living with a partner; single, divorced or cohabiting. Level of education was dichotomized as low or high: fewer than 13 years of education was considered low, and a university education was considered high. Pre-injury employment status was categorized into the following 4 categories: being employed or a student; receiving sick leave, vocational or medical rehabilitation, social security support or a disability pension; being unemployed; and being retired or a homemaker. The employment variable was further dichotomized as being employed or a student vs the other 3 categories. When possible and highly probable, missing data for education were imputed based on type of work. For example, a participant whose occupation was listed as “fisherman” was categorized as having a low education. Comorbidity was coded as: having no comorbidity, having a TBI prior to the present injury, or having another disease at time of injury (heart condition, neurological disorder, multiple comorbidities).
The GCS was used for estimating TBI severity (25). The lowest GCS score within the first 24 h post-injury, or at the site of injury in cases of pre-hospital intubation, was registered. Other injury severity scores were provided by the regional trauma registries at the hospitals. In the AIS scoring system, injury severity is graded as 1 (minor), 2 (moderate), 3 (serious), 4 (severe), 5 (critical) or 6 (maximum; lethal injury with no known cure) (26). For each participant, the score of their most severe brain injury, AIS-head, was registered.
The ISS is the sum of the 3 highest squared AIS scores in 3 different body regions (27). A score above 15 is considered a severe injury.
The Rotterdam CT score is a CT classification with a range from 1 (least severe) to 6 (most severe). This score describes the status of basal cisterns, midline shift, epidural mass lesion and intraventricular blood or traumatic subarachnoid haemorrhage (SAH). The score predicts mortality at 6 months post-injury (28). The Rotterdam CT scoring was performed by neuroradiologist in 3 of the 4 hospital regions, and by a neurosurgeon in the remaining region. Scoring was based upon CTs from the acute hospital stay, and the worst score registered was used for analysis.
The Functional Independence Measure (FIM) assesses activities of daily living (ADLs). It has 18 items: self-care, sphincter control, mobility, communication, cognition and social adjustment (29). It consists of a summary score and 2 sub-scales, the FIM Motor (FIM-M) and FIM Cognitive (FIM-COG). FIM-M ranges from 13 to 91 points, and FIM-COG ranges from 5 to 35 points. Total FIM scores were dichotomized at the lowest quartile for the regression analysis. The FIM-M score was dichotomized as low/high at 90 points, but otherwise a FIM-M score ≤77 is set as a cut-off for being limited in activities; assistance from another person is needed. The FIM-COG score was also dichotomized as low or high; at 30 points, which also is the cut-off for being limited in ADLs for this subscale; assistance from another person is needed. The FIM was scored at 12 months.
The Glasgow Outcome Scale Extended (GOSE) (30) is an outcome scale that assesses global functioning by a structured interview in which the patients are divided into the following categories: 1 (dead), 2 (vegetative state), 3 (lower severe disability and complete dependence on others), 4 (upper severe disability and some dependence on others), 5 (lower moderate disability and unable to work or only able to work at a lower level of performance), 6 (upper moderate disability and able to return to previous work with some adjustments), 7 (lower good recovery with minor physical or mental deficits), and 8 (upper good recovery). The GOSE scores were categorized as Severe Disability (GOSE 3–4), Moderate Disability (GOSE 5–6), and Good Recovery (GOSE 7–8). The GOSE was administered at 3 and 12 months post-injury.
The Rivermead Post-concussion Questionnaire (RPQ) is a self-report questionnaire originally designed to measure severity of post-concussion symptoms following mild TBI (31). It has 16 items on the following 3 subscales: somatic (headache, dizziness, nausea, noise sensitivity, sleep disturbance, fatigue, blurred vision, light sensitivity, double vision), emotional (irritability, depression, frustration, restlessness) and cognitive (memory, concentration, speed of thought). The RPQ has shown satisfactory psychometric properties. It is scored with a 5-point scale, ranging from 0 (no problems) to 4 (severe problems), and the sum score range is 0 to 64, with higher scores indicating more problems. The RPQ scores are the sum of symptoms scores, excluding the ratings of one because this score signifies a level that is the same as pre-injury.
The Hospital Anxiety and Depression Scale (HADS), a 14-item measure that has been validated for persons with TBI, was administered at 12 months post-injury (32, 33). The items are measured on a scale from 0 (not at all) to 3 (yes definitely), and the scores range is from 0 to 42, with higher scores indicating more problems. Scores above 8 points on each subscale are considered indicative of clinically significant depression and anxiety (32). The total score, a combination of the depression and anxiety subscale, was analysed in the current study as an indicator of psychological distress. Scores between 15 and 18 were considered possible cases, whereas scores of 19 or above were considered indicative of clinically significant psychological distress requiring treatment (32).
The QOLIBRI was the main outcome measure in the present study. It is a self-report measure of HRQL after a TBI, which has 37 items (23, 24). The first part taps on the responders’ satisfaction with their HRQL in 4 domains (subscales) comprising cognition, self, daily life and autonomy, and social relationships. The second part relates to how bothered the responders rate themselves after TBI in 2 domains (subscales) concerning emotions and physical problems. Each item is scored on a 5-point scale, from 1 (not-at-all satisfied) to 5 (very satisfied), with reverse scoring on the bothered subscales (21, 23). The QOLIBRI was scored according to an algorithm published by von Steinbüchel et al. (23). Missing item scores on each subscale were imputed by the scale mean if less than one-third of the responses were missing. Raw scores were transformed into a score range of 0 (lowest) to 100 (highest) (22). Individual subscale scores and a total score were calculated. The QOLIBRI has shown satisfactory psychometric properties (21, 23). The internal consistency of the subscales and total score in the present study were measured with Cronbach’s α: cognition (α = 0.92), self (α = 0.92), daily life and autonomy (α = 0.90), social relationships (α = 0.84), emotions (α=0.89), physical problems (α = 0.78) and total score (α = 0.90). The QOLIBRI was administered at 12 months. The QOLIBRI was most often not administered to patients who had a GOSE of 3 at 3 months. However, for 7 patients with a GOSE of 3, QOLIBRI was completed by family or a personal assistant (22).
Data analysis and statistics
Descriptive data are displayed as the mean, SD and range, or as the median and interquartile range (IQR). Cross-tabulations with χ2-tests were performed for nominal data. Correlations were analysed with Spearman’s ρ or Pearson’s r. t-tests or analysis of variance (ANOVAs) were used to compare groups. Non-parametric statistical analyses were used for data that were not normally distributed.
Hierarchical multiple linear regression analysis was performed to assess factors that were associated with the QOLIBRI outcome at 12 months post-injury. Variables with p-values ≤ 0.1 from the univariate regression analyses were included in the multivariate model. The model comprised 99 people, and using 8 people per predictor variable, the model allowed 12 variables. In the univariate linear regression analyses, sex, age and education did not fulfil the criteria, but these factors and work status at time of injury were included in the regression analyses to adjust for heterogeneity among socio-demographic data. Several of the associations between QOLIBRI outcome and injury severity, such as ISS, GCS, Rotterdam score, PTA and comorbidity, were not sufficiently strong to be applied in this study and, as such, these statistical tests will not be described further here.
The first step of the hierarchal regression analysis examined the following demographic variables: age, sex (male/female), education (low vs high), pre-injury employment status (employed/student vs others). The second step examined injury severity (AIS-head). The third and fourth steps examined post-injury functioning at 3 months (GOSE and RPQ) and 12 months (GOSE, dichotomized FIM-M and FIM-COG, RPQ and HADS), respectively. The RPQ and HADS were log10 transformed to improve the distribution. The results are presented as R2, R2 change, F change and standardized beta values.
p-values ≤ 0.05 were considered statistically significant. All variables in the analyses had ≤ 10% missing cases. Analyses were performed using IBM SPSS Statistics 19.
RESULTS
The injury characteristics of the participants are shown in Table II. The majority of respondents were injured in road traffic accidents (n = 61, 48.0%). The participants had severe injuries, with a mean GCS score of 5.9 (SD 1.9) and a mean AIS-head score of 4.2 (SD 0.9). Fifty-nine people (43.0%) had an AIS-head of 5, which is indicative of critical injuries.
Approximately 5.0% (n = 6) of the patients reported a history of TBI prior to the present injury, and 39.0% (n = 49) reported having one or more other comorbid diseases.
|
Table II. Injury-related data of the participants |
|
|
Injury characteristics |
|
|
GCS (n = 126), mean (SD) |
5.9 (1.8) |
|
AIS-head (n = 124), mean (SD) |
4.2 (0.9) |
|
ISS (n = 124), mean (SD) |
27.2 (11.8) |
|
Length of PTA, (n = 124), n (%) < 1 weeks 1–2 weeks 2–3weeks 3–4 weeks > 4 weeks |
29 (23.4) 17 (13.7) 12 (9.7) 12 (9.7) 54 (43.5) |
|
Rotterdam score (n = 124), mean (SD) |
3.5 (0.9) |
|
Injury mechanism (n = 126), n (%) Traffic Fall Violence Other |
61 (48.4) 49 (38.8) 7 (5.6) 9 (7.1) |
|
Injury type (n = 126) n (%) Isolated TBI TBI with multiple trauma |
55 (43.7) 71 (56.4) |
|
GCS: Glasgow Coma Scale; ISS: Injury Severity Score; PTA: post-traumatic amnesia; SD: standard deviation; TBI: traumatic brain injury; AIS: Abbreviated Injury Scale. |
|
Mean QOLIBRI total score was 68.5 (SD 18.8). The subscale and total scores are displayed in Table III.
|
Table III. Quality of Life after Brain Injury (QOLIBRI) scores at 12 months post-injury |
|
|
QOLIBRI scale |
Mean (SD) |
|
Cognition |
68.3 (21.8) |
|
Self |
64.6 (22.9) |
|
Daily life and autonomy |
65.7 (24.1) |
|
Social Relations |
70.8 (21.4) |
|
Emotions |
75.1 (24.6) |
|
Physical problems |
68.6 (22.0) |
|
Total score |
68.5 (18.8) |
|
SD: standard deviation. |
|
Table IV displays the post-injury disability and functioning scores. There was a significant reduction in disability of 0.9 points on the GOSE from 3 to 12 months (p < 0.001). The distribution of GOSE disability categories at 3 and 12 months is shown in Table V. The ANOVA showed that there were significant differences in QOLIBRI scores between participants with good recovery on the GOSE at 12 months, who scored 81.1 points (SD 14.5), and those with moderate (61.1 points (SD 17.1), p < 0.001) and severe disability (62.0 points (SD 17.5), p = 0.001). According to the HADS, 17.9% of the participants had symptoms of psychological distress at 12 months post-injury. Six patients (5.0%) had mild-moderate symptom pressure, whereas 16 (13.0%) patients had symptoms of anxiety and depression that required treatment. According to the dichotomized FIM-M and FIM-COG scales, a small percentage of patients (6.7%) were limited in motor function such that they needed another person for assistance, whereas 20.0% were limited in cognitive tasks and needed another person for assistance.
|
Table IV. Disability and functioning at 3 and 12 months post-injury. The results are shown as mean (SD) or median (IQR) |
||
|
3 months |
12 months |
|
|
GOSE, mean (SD) |
5.2 (1.3) |
6.1 (1.4) |
|
RPQ, median (IQR) |
10.0 (4.0–18.0) |
12.5 (4.0–23.0) |
|
FIM-M, median (IQR) |
n.a. |
90.0 (90.0–91.0) |
|
FIM-COG, median (IQR) |
n.a. |
34.0 (30.0–35.0) |
|
FIM – Sum, median (IQR) |
n.a. |
125.0 (120.0–126.0) |
|
HADS, median (IQR) |
n.a. |
8.0 (3.0–12.0) |
|
n.a.: not applicable; SD: standard deviation; IQR: interquartile range; GOSE: Glasgow Outcome Scale Extended; RPQ: Rivermead Post-concussion Questionnaire; FIM; Functional Independence Measure: FIM-M: FIM Motor; FIM-COG: FIM Cognitive; HADS: Hospital Anxiety and Depression Scale. |
||
|
Table V. Distribution of patient frequency (%) in the Glasgow Outcome Scale Extended (GOSE) disability categories at 3 and 12 months for the 126 patients |
||
|
3 months n (%) |
12 months n (%) |
|
|
GOSE 3–4, severe disability |
25 (19.8) |
12 (9.6) |
|
GOSE 5–6, moderate disability |
85 (67.4) |
68 (53.9) |
|
GOSE 7–8, good recovery |
16 (12.7) |
46 (36.5) |
The results of the multiple regression analysis are presented in Table VI. The analysis showed that employment status before the injury was the only demographic factor that predicted HRQL on the QOLIBRI. AIS-head was a significant predictor when the model controlled for demographic factors (step 2) and functioning at 3 months (step 3). GOSE (p = 0.004) and RPQ at 3 months (p < 0.001) were significant predictors of the QOLIBRI. The adjusted R2 showed that the regression model explained 64.0% of the variance in the QOLIBRI score. The R2 change showed that demographic variables explained 7.0% of the variance; AIS-head added 4.0% to the explained variance, and functioning on the GOSE and RPQ at 3 months added another 29.0% of the variance. The last step added another 28.0% to the explained variance. The HADS was the strongest individual predictor in the final model (p < 0.001).
|
Table VI. Results from the multiple hierarchical regression models of the Quality of Life after Brain Injury score (n=99) |
||||
|
Step 1 |
Step 2 |
Step 3 |
Step 4 |
|
|
Age at injury |
0.13 |
0.12 |
0.12 |
0.08 |
|
Sex (men/women) |
–0.05 |
–0.04 |
0.03 |
0.08 |
|
Education (low/high) |
0.02 |
0.03 |
0.04 |
–0.01 |
|
Pre-injury employment (working or studying/other) |
0.28** |
0.28** |
0.22* |
0.15* |
|
AIS-head |
0.20* |
0.25** |
0.05 |
|
|
GOSE 3 months |
0.26** |
0.17* |
||
|
RPQlg 3 months |
–0.41*** |
–0.04 |
||
|
GOSE 12 months |
0.17* |
|||
|
RPQlg 12 months |
–0.30** |
|||
|
FIM-M low/high |
0.05 |
|||
|
FIM-C low/high |
0.05 |
|||
|
HADSlg |
–0.40*** |
|||
|
R2 |
0.07 |
0.11 |
0.40 |
0.68 |
|
Adjusted R2 |
0.03 |
0.06 |
0.36 |
0.64 |
|
R2 Change |
0.07 |
0.04 |
0.29 |
0.28 |
|
F Change |
1.80 |
4.16* |
22.44*** |
15.35*** |
|
*p = 0.05; **p = 0.01; ***p <0.001. Standardized beta coefficients are presented. AIS: Abbreviated Injury Scale; FIM; Functional Independence Measure: FIM-M: FIM Motor; FIM-COG: FIM Cognitive; GOSE: Glasgow Outcome Scale Extended; HADSlg; Hospital Anxiety and Depression Scale log10 transformed: RPQlg: Rivermead Post-concussion Questionnaire log10 transformed. |
||||
DISCUSSION
This study is the first to describe HRQL in a population of patients with severe TBI using the QOLIBRI. The findings are consistent with other studies where the SF-36, a generic measure of HRQL commonly used in TBI outcome research, was applied (3, 16, 34). The current study supplements the larger multi-centre project by enforcing the patient perspective on subjective health, well-being and functioning after severe TBI (35).
Responses on the QOLIBRI subscales showed that there was no single aspect that was particularly more reduced than the others. Nonetheless, the patient’s satisfaction with self, comprising items related to motivation, self-esteem, energy and self-perception, had the lowest subscale score. Fatigue is a well-known condition following TBI of all severities, which is linked to the change in cognitive capacity, sleep disturbance, pain and depression (19, 36). Concerning post-TBI feelings and perceptions of self, a recent review of a qualitative study performed by Levack et al. (11) describes several inter-related themes, including a mind/body disconnect, a disconnect with pre-injury identity, and the reconstruction of self-identity and of personhood.
Emotional well-being was the least reduced of the QOLIBRI subscales. This result is consistent with results on the HADS, which revealed that fewer than 20% of participants reported psychological distress at 12 months. However, participants reported more psychological distress on the HADS compared with the general population, in which the lifetime prevalence of depression is estimated to be 9% (37).
Compared with Truelle et al.’s study (22), in which 58% of patients were characterized as having a severe TBI, patients in the current study reported significantly higher HRQL (total score of 68.5 points vs 64.6 points). Comparatively higher scores were identified on all QOLIBRI subscales, except daily life, autonomy and physical function. The largest differences were in the areas of cognition, emotions and social relations. Comparing the differences between these two studies might shed some light on individuals’ adaptation in the rehabilitation process. Recognition of the impact of the TBI on solving cognitive tasks and general tasks and demands may evolve over time; social relations may suffer, and the experienced emotional distress may increase.
Patients in the current study had sustained their TBI 12 months prior to evaluation, whereas the time since injury was considerably longer in the study by Truelle et al. (22). As such, participants were still in a rehabilitation and recovery phase and had been exposed to the requirements and expectations of everyday life (e.g. work participation, social demands) to a lesser extent than the previous sample. Therefore, the differences in scores might be caused by less exposure to socially and cognitively challenging situations. Moreover, recent recommendations made by the Norwegian Health Authorities (http://www.helsedirektoratet.no/IS-1279) resulted in the improvements to rehabilitation protocols available to these patients, as well as in more seamless chains of treatment. Improved care and rehabilitation efforts might contribute to less uncertainty with respect to the current and future situation and contribute to the HRQL (38).
Linear regression analysis was used to determine the factors that contribute to the HRQL at 12 months post-injury. Of demographic variables, only pre-injury work status was a predictor of HRQL on the QOLIBRI in all steps of the regression analysis, reflecting the importance of a pre-injury productive lifestyle to HRQL (12).The relationship between pre-injury work and HRQL has been well established in previous literature. Pre-injury employment status in this study may have served as a proxy for personal resources that might strengthen or impair perceived health status and HRQL post-TBI. However, this study was not designed to assess personal resources and their influence on HRQL.
In line with our hypothesis, injury severity variables, such as GCS, intra-cranial injury assessed by the Rotterdam CT Score and the ISS, were not associated with HRQL. However, AIS head contributed significantly to the QOLIBRI score at the third step of the regression analysis, with predictors at 3 months indicating that a more severe head injury was associated with higher HRQL. This result is consistent with previous studies and suggests the link between severity of injury, reduced awareness and self-reported HRQL (39). However, AIS head was not a significant predictor in the final step of the regression with concurrent functional status and psychological distress added to the model. The association between injury severity and HRQL may dissolve over time, and other variables, such as psychological and social components, may become more important for HRQL at the later stages of injury (2, 14).
Global functioning, as evaluated by GOSE scores at 3 months and 12 months, was a significant predictor of HRQL in the current study. In addition, significant improvements in GOSE scores from 3 to 12 months post-injury were found, suggesting that disability following TBI is not static (38). Significant associations between recovery and QOLIBRI scores have been shown in other studies on TBI populations of all severities (21, 24). The analysis showed that patients with severe and moderate disability demonstrated the greatest reductions in HRQL; this result is consistent with Truelle’s study (22). However, no significant differences in QOLIBRI mean scores were found between these two disability groups, suggesting that patients with the worst outcomes may adjust well to TBI consequences (24). Other possible explanations may include reduced awareness (39), impaired memory of problems within QOLIBRI domains or better support provided to severely disabled people compared those with moderate disability (22). Furthermore, in 7 cases, relatives assisted the patients in completing the QOLIBRI, which may have led to over- or under-estimation of the HRQL in the most severe patient group. However, patients with a good recovery also reported reduced HRQL compared with the highest scale scores. These findings highlight the importance of including the subjective patient experience in TBI outcome evaluations.
Participants’ scores on the RPQ showed that the self-reported symptom pressure of the TBI reflecting somatic, cognitive and emotional impairments was lower at 3 months than at 12 months. One possible explanation for the increase in symptoms is that individuals with severe TBI may be less aware of their deficits for organic reasons, and thus these individuals may under-report symptoms during the first months post-injury (40). When the RPQ was added into the regression analysis, it was a significant predictor of HRQL. This finding suggests that a relationship exists between self-reported complaints and HRQL, supporting previous research (19). Our hypothesis that symptom pressure would be negatively associated with HRQL is similarly supported. However, no previous studies have reported RPQ as a predictor of HRQL in individuals with severe TBI.
In the current study, cognitive function was measured as self-reported symptoms on the RPQ, and cognitive functional ability was assessed via the FIM-COG by health personnel. FIM-COG scores were not associated with HRQL, even though satisfaction with cognitive functioning is a subscale of the QOLIBRI. More specifically, although the FIM-COG is widely used for evaluating cognitive sequelae in TBI, it is of limited sensitivity to cognitive disability after patient discharge from sub-acute rehabilitation and in TBI patients with high functional levels (3). Therefore, cognitive dysfunction may be underestimated in this study and may account for the non-significant relationship between FIM-COG and HRQL. In contrast, psychological distress at 12 months on the HADS was a significantly associated with HRQL, supporting our study hypothesis as well as other studies reporting that emotional status influences HRQL (4). Of course, depression and psychological distress are common problems after sustaining severe TBI, and significant correlations between the mental health subscales on the SF-36 and depression and between the QOLIBRI and depression have been identified in the TBI population (24).
Ahmadi et al. (41) found that, although patients in their study demonstrated reduced functioning on neuropsychological tests 12 months post-injury, and although depression was significantly more prevalent in patients than in healthy controls, the patients reported only moderately reduced HRQL on the SF-36. They emphasized that rehabilitation should be better targeted for both cognitive and psychological outcomes. In addition, Diaz (34) et al. reported a significant increase in the prevalence of major depressive disorder and generalized anxiety disorder after severe TBI. Depression was related to personality changes and had a negative impact on the HRQL on the SF-36.
The results of this study might serve to guide the rehabilitation processes for people with severe TBI. The strength of this multicentre study is that it used a representative cohort of Norwegian adults who were admitted to the trauma referral centres for severe TBI, who received rehabilitation care in the course of injury and who survived the first year after the injury. Nevertheless, a multicentre study will always be flawed by differences among study centres that are not documented, and by biases in registration procedures. Population norms are usually used to provide reference values for post-injury HRQL; however, such data do not exist for QOLIBRI scores.
In conclusion, our study indicates that somatic, emotional and cognitive symptom pressure and global functioning in the sub-acute phase of TBI, as well as psychological distress in the post-acute phase, are important for the self-perceived HRQL 12 months after injury. These domains are modifiable and should be the focus of rehabilitation interventions aiming to improve HRQL in patients with severe TBI.
ACKNOWLEDGEMENTS
We thank the Trauma Registry at Oslo University Hospital and Haukeland University Hospital for providing data regarding injury severity. We also thank Tone Jerstad, neuroradiologist for her effort in analysing the majority of CT scans and providing the Rotterdam scores. This multicentre study was funded by the Norwegian Research Council.
REFERENCES
