Laura Hak, PhD1, Han Houdijk, PhD1,2, Peter van der Wurff, PhD3, Maarten R. Prins, MSc1,3, Peter J. Beek, PhD1,4 and Jaap H. van Dieën, PhD1,5
From the 1Research Institute MOVE, Faculty of Human Movement Sciences, VU University Amsterdam, 2Heliomare Rehabilitation Centre, Wijk aan Zee, 3Center for Augmented Motor Learning and Training, National Military Rehabilitation Centre Aardenburg, Doorn, The Netherlands, 4Brunel University, School of Sport & Education, Uxbridge, UK and 5King Abdulaziz University Jeddah, Saudi Arabia
OBJECTIVE: To investigate whether post-stroke participants can walk at different combinations of stride frequency and stride length and how these adaptations affect the backward and medio-lateral margins of stability.
SETTING: Computer Assisted Rehabilitation Environment (CAREN).
PARTICIPANTS: Ten post-stroke individuals.
INTERVENTION: Six trials of 2 min walking on a treadmill at different combinations of stride frequency and stride length. Treadmill speed was set at the corresponding speed, and subjects received visual feedback about the required and actual stride length.
OUTCOME MEASURES: Mean stride length and frequency and backward and medio-lateral margins of stability for each trial.
RESULTS AND CONCLUSION: Stroke patients were able to adjust step length when required, but had difficulty adjusting step frequency. When a stride frequency higher than self-selected stride frequency was imposed patients additionally needed to increase stride length in order to match the imposed treadmill speed. For trials at a high stride frequency, in particular, the increase in the backward and medio-lateral margins of stability was limited. In conclusion, training post-stroke individuals to increase stride frequency during walking might give them more opportunities to increase the margins of stability and consequently reduce fall risk.
Key words: stroke; gait; rehabilitation; accidental falls.
J Rehabil Med 2015; 47: 00–00
Correspondence address: Jaap H. van Dieën, Research institute MOVE, VU University Amsterdam, Van der Boechorststraat 9, NL-1081 BT Amsterdam, The Netherlands. E-mail: j.van.dieen@vu.nl
Accepted Aug 14, 2014; Epub ahead of print Nov 6, 2014
Introduction
Multiple studies have shown that post-stroke individuals fall far more often than able-bodied people in the same age category (1–6). Because of the high incidence of falls, as well as the severe consequences that falls might have in post-stroke individuals, there is a large body of research focusing on this specific problem (7–10). From these studies it appears that walking is one of the activities during which the risk of falling is relatively high (5). Stroke patients are at increased risk of falling during walking, because of, among other factors, larger centre of mass (CoM) excursions during walking (10–12), in combination with difficulties in foot placement, which affect the place and size of the base of support (BoS) (12).
Balance during walking can be quantified by the margins of stability (MoS), which describe the movement of the body CoM relative to the BoS. Balance during dynamic tasks such as walking not only depends on the position of the CoM with respect to the BoS, but also on the velocity of the CoM. Therefore the MoS during walking is defined as the distance between the extrapolated centre of mass (XCoM) and the limits of the BoS, where the XCoM takes both the position and the velocity of the CoM into account (13). The MoS can be calculated in both medio-lateral (14–16) and backward (15–18) direction, where the backward MoS is usually calculated with respect to the posterior border of the BoS of the leading foot at initial contact (Fig. 1). A negative medio-lateral MoS, implying that the XCoM is located lateral of the border of the BoS, will result in a deviation from a straight walking trajectory. A negative backward MoS, implying that the XCoM is located posterior to the border of the BoS of the leading foot, will result in an interruption of forward progression.
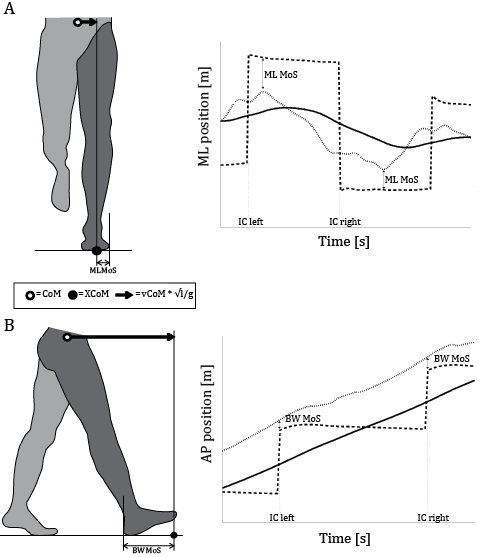
Fig. 1. Schematic representation of the definition of the backward and medio-lateral margin of stability (MoS). (A) The medio-lateral (ML) MoS is defined as the minimum distance in medio-lateral direction between the extrapolated centre of mass (XCoM; dotted line in the right panel) and the lateral border of the foot during foot-contact. The XCoM is calculated as the position of the centre of mass (CoM; solid line in the right panel) plus its velocity (vCoM) times a factor √(l⁄g), with l being the length of the pendulum (for which leg length is often used) and g the acceleration due to gravity. (B) The backward (BW) MoS is defined as the distance in anteroposterior direction between the XCoM and the posterior border of the leading foot (dashed line in the right panel) at initial contact.
In a previous study, we compared medio-lateral and backward MoS between post-stroke individuals and able-bodied controls (12). This was done during unperturbed walking, as well as during more challenging walking conditions with perturbations of the walking surface and with a gait adaptability task in which fast and accurate adaptations of the gait pattern had to be made in order to hit virtual targets projected on a screen. For all conditions, post-stroke individuals appeared to be able to regulate their medio-lateral MoS to the same degree as able-bodied subjects, despite larger medio-lateral excursions of the XCoM compared with able-bodied controls. To this end, post-stroke individuals had to walk with a larger step width and a relatively high stride frequency, compared with able-bodied controls. In contrast, the backward MoS was smaller in post-stroke individuals. This smaller backward MoS appeared to be caused by inadequate adjustments in stride frequency and stride length, resulting in a decrease in walking speed during challenging conditions. Able-bodied subjects kept their walking speed constant compared with unperturbed walking, and adapted both stride frequency and stride length to adequately perform the gait adaptability task.
The aforementioned results (12) indicate that post-stroke individuals respond differently to manipulations of gait stability and adaptability, compared with able-bodied controls, and that this difference has a detrimental effect on the backward MoS. However, these results do not elucidate whether post-stroke individuals are simply unable to use the same strategy as able-bodied controls, or prefer to use an alternative strategy for other reasons. The limited increase in stride frequency and stride length in post-stroke individuals might be caused by reduced push-off (19–22) and swing capacity (23–25) of the hemiparetic leg, for instance as a result of muscle weakness and/or spasticity. However, the results of our previous study (12) could also be explained by a higher fear of falling (26) in post-stroke individuals, or by a conflict between the cognitive demands of the gait adaptability task and walking ability (27–29). As a consequence of such emotional and cognitive factors, these subjects might choose to reduce their walking speed, even though they are physically able to maintain walking speed in these situations.
The primary aim of the present study was therefore to investigate whether post-stroke individuals are able to voluntarily adapt their gait pattern and walk at different combinations of stride frequency and stride length, both at a comfortable walking speed and at higher speeds. The second aim was to investigate how adjustments in stride frequency and length, and the concomitant change in walking speed influence the size of the backward and medio-lateral MoS and whether potential difficulties in adapting stride frequency and length limit the backward and medio-lateral MoS. With respect to the first research question, we hypothesized that post-stroke individuals would experience difficulties with increasing their stride frequency and stride length. This would stand in contrast to the performance of young and able-bodied subjects, who were able to increase both stride frequency and stride length independently from each other (30). With respect to the second research question we hypothesized that potential difficulties in adapting stride parameters will result in limitations in backward and medio-lateral MoS (30).
Methods
Subjects
Ten adult subjects (mean age 57.6 years (standard deviation (SD) 15.4), mean height 1.72 m (SD 0.11) and mean weight 77.9 kg (SD 16.5)) who had had a stroke participated in this study. Participants were recruited from the patient population of the Military Rehabilitation Centre Aardenburg, Doorn, The Netherlands. Additional subject characteristics are reported in Table I. All participants were under treatment during the period in which the experiment took place. A minimum score of 4 on the Functional Ambulation Categories (FAC) (31), in combination with a minimum score of 45 on the Berg Balance Scale (BBS) (32), was required to participate in this study. Exclusion criteria were: (i) cognitive or communicative disorders (Mini Mental State Examination < 24), visual impairments and attention impairments that can affect the performance on the experiment, (ii) severe cardiovascular diseases that contraindicate moderately intense exercise, (iii) other co-morbidities that could affect balance control during walking, and (iv) medication that could interfere with balance control during walking. One of the subjects (number 10, Table I) had a much longer time since stroke compared with the other subjects; however this subject was included in the study because he was under treatment again during the study period and he met the inclusion and exclusion criteria. The medical ethics committee of VU Medical Center Amsterdam approved the study protocol before it was conducted (Ref: NL35402.029.11) and all subjects gave their written informed consent in accordance with university policy.
|
Table I. Subject characteristics |
||||||
|
Subject No. |
Age, years/sex |
Height, m |
Weight, kg |
Side hemiparesis |
Berg Balance Scale |
Time since stroke, months |
|
1 |
39/F |
1.70 |
70 |
Left |
52 |
4 |
|
2 |
70/F |
1.70 |
65 |
Left |
56 |
3 |
|
3 |
26/F |
1.50 |
54 |
Left |
56 |
1 |
|
4 |
73/M |
1.85 |
90 |
Left |
51 |
1.5 |
|
5 |
62/M |
1.75 |
90 |
Right |
55 |
1 |
|
6 |
62/M |
1.74 |
95 |
Right |
45 |
1.5 |
|
7 |
59/M |
1.83 |
96 |
Right |
54 |
6 |
|
8 |
62/M |
1.77 |
82 |
Left |
51 |
17 |
|
9 |
74/F |
1.60 |
52 |
Right |
56 |
6 |
|
10 |
49/M |
1.80 |
85 |
Right |
54 |
93 |
Equipment
All subjects walked in the so-called Computer-Assisted Rehabilitation Environment (CAREN) of Motek Medical b.v., Amsterdam, The Netherlands, which consists of an instrumented treadmill mounted onto a 6-degree-of-freedom motion platform in combination with a virtual environment. Twelve high-resolution infrared cameras (Vicon, Oxford, UK) were used to capture kinematic data of 16 reflective markers attached to the pelvis and the lower extremities (lower body plug-in-gait (33, 34)). A safety harness system suspended overhead prevented the subjects from falling, but did not provide weight support. In the present experiment, the virtual environment was used to provide real-time feedback about the current and required stride length (Fig. 2; upper panel).
Protocol
Familiarization session. Prior to the experiment, each participant performed a 30-min familiarization session, on another day than the experimental session. During this session all experimental conditions were practiced.
Experimental protocol. After a warm-up trial, the experiment started with approximately 3 min of walking. During the first minute of this trial, the comfortable walking speed was determined by gradually increasing the belt speed until the subject reported that the current walking speed was comfortable. Belt speed was then increased beyond the reported comfortable walking speed and subsequently gradually decreased until the subject reported that the current walking speed was comfortable again. Comfortable walking speed was defined as the mean of the 2 reported comfortable walking speeds. During the second minute of the trial, subjects walked at their comfortable walking speed and during the last minute of the trial the comfortable stride length was determined. The experimental protocol consisted of 6 trials of 2 min of walking. Subjects walked at different walking speeds by either increasing stride length, stride frequency or both. Walking speed, stride length and, hence, also stride frequency were imposed as a percentage of the comfortable value. In Fig. 2, an overview of these percentages for the different experimental trials is given. The percentages of comfortable stride frequency and stride length were chosen in such a way that walking speed was the same for the trials on the diagonals from the upper left to the lower right. For each trial, belt speed was set at the required walking speed for the trial in question. During the trial, visual feedback about the required and the actual stride lengths was given through the virtual environment (Fig. 3). This feedback method allowed some natural fluctuations in stride length and frequency at the imposed speed.
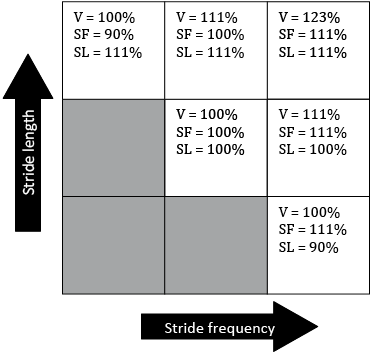
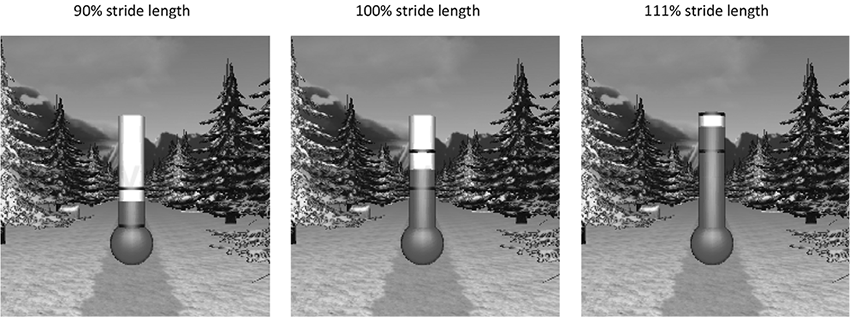
Fig. 3. Visual feedback given about the required stride length (the height of the area between the dark lines) and the current stride length (the height of the grey column). The lower part of the thermometer corresponds to 90% of comfortable stride length (left-hand picture), the middle part of the thermometer corresponds to 100% of comfortable stride length (middle picture), and the upper part of the thermometer corresponds to 111% of the comfortable stride length (right-hand picture). Subjects were instructed to keep the grey column between the dark lines.
Data collection
Three-dimensional positional data of markers attached to the lateral malleoli of the ankles, heels and the pelvis (left and right anterior superior iliac spines (LASI & RASI), and left and right posterior superior iliac spines (LPSI & RPSI)) were collected with the Vicon system. The sample rate of data collection was 120 samples/s.
Data analysis
Before data analysis, kinematic data were low-pass filtered with a bi-directional Butterworth filter with a cut-off frequency of 4 Hz; the first 15 s of each trial were removed to eliminate start-up effects.
Stride frequency and stride length. Stride frequency was determined as the inverse of the mean duration between 2 subsequent heel-strikes, where heel-strikes were detected as the local maxima of the position of the ankle markers in the anterioposterior direction. Stride length was calculated as the anterior-posterior distance between both ankle markers at the moment of heel-contact. Besides the absolute values for stride length and stride frequency, the relative stride length (SLrel) and frequency (SFrel) were calculated by dividing the absolute values for each trial by the preferred stride length and frequency measured during the pre-experimental trial.
Margins of stability. To calculate the MoS, a method derived from the procedure developed by Hof et al. (13) was used. In the present study, the extrapolated centre of mass (XCoM) was defined as the mean of the markers attached to the LASI, RASI, LPSI and RPSI, which served as an estimate of the centre of mass (CoM), plus its velocity times a factor √(l⁄g), with l being the maximal height of the estimated CoM and g the acceleration of gravity. The margins of stability (MoS) were calculated as the position of the XCoM relative to the lateral malleolus of the ankle of the leading foot for the medio-lateral MoS and relative to the heel marker of the leading foot for the backward MoS. For each step, medio-lateral and backward MoS were calculated for the moment at which the MoS reached its minimum value within each step and were subsequently averaged over all strides within the trial. Although similar in concept, our method differs from that of Hof et al. (13) as he used force plate data for calculating the XCoM and the margins of stability. In addition, in our definition of the backward MoS, the equation XCoM-BoS was used, instead of the original equation BoS-XCoM by Hof et al. (13).
Statistical analysis
To establish whether subjects were able to adjust their stride length and stride frequency following the instructions that were given, generalized estimating equations (GEE) were used to evaluate the following regression equation: SLrel = intercept + βSL*imposed SLrel + βSF*imposed SFrel. GEE is a regression analysis technique that accounts for the dependency of repeated measurements. In this analysis the imposed stride frequency and stride length were expressed as a fraction of the comfortable value. In the regression equation βSL and βSF are the regression coefficients that quantify the contribution of the imposed adjustments in stride length and/or stride frequency to the actual adjustment in stride length. If subjects were fully able to follow the instructions, the regression equation would look like: SLrel = 0 + 1*imposed SLrel + 0*imposed SFrel. A βSL that is significantly smaller or larger than 1 would imply that subjects adjusted stride length respectively less or more than the imposed adjustment in stride length. A βSF that is significantly smaller or larger than 0 would imply that subjects respectively decreased or increased their stride length, when only an adjustment in stride frequency was imposed. Note, that since stride length and frequency are mutually dependent when treadmill speed is imposed, a second regression equation evaluating actual stride frequency is redundant, and therefore not analysed
GEE were also used to investigate whether performed SLrel and SFrel influenced the size of the medio-lateral and backward MoS. The latter regression equation was subsequently used to predict values for the medio-lateral and backward MoS that could have been reached when subjects would have fully adapted their stride frequency and length to the imposed adjustments and to compare these values with the medio-lateral and backward MoS that were actually observed as a result of the realized adaptations in stride frequency and stride length.
In the case of a non-significant regression coefficient or intercept, the GEE analysis in question was repeated after removing these non-significant factors from the model. Because all trials were offered randomly, an exchangeable working correlation matrix was chosen to define the dependency of the repeated measurements in the model. These analyses were performed using IBM SPSS Statistics 20.0.
Results
The results of the GEE analyses are summarized in Table II. From the regression coefficients presented in Table II it can be derived that subjects adjusted stride length significantly when adjustments in stride length were imposed (βSL = 1.096; p < 0.001). The βSL of 1.096 significantly differs from 1 (as the 95% confidence interval did not include 1). This implies that the adjustments in stride length were slightly larger than the imposed adjustments in stride length. Subjects also adjusted stride length when they were asked to adjust stride frequency (βSF = 0.263; p < 0.001). This indicates that the adjustments in stride frequency were limited for these trials, and therefore adjustments in stride length were necesarry to walk at the required treadmill speed.
Backward MoS increased both with an increase in stride length (βSL = 0.092; p < 0.001) and with an increase in stride frequency (Table II: βSF = 0.437; p < 0.001), while medio-lateral MoS only increased with an increase in stride frequency (Table II: βSF = 0.054; p < 0.001). The regression equations presented in Table II were subsequently used to predict the values for the medio-lateral and backward MoS that could have been reached when subjects would have fully adapted their stride frequency and length to the imposed adjustments (white bars in Fig. 4) and to compare those to the backward and medio-lateral MoS that were realized by the actually performed adaptations in stride frequency and stride length (black bars in Fig. 4). In Fig. 4, it can be seen that the increase in medio-lateral and backward MoS was especially limited for the trials in which subjects were instructed to walk at 111% stride frequency compared with the trials at comfortable stride frequency. In comparison, when subjects would have fully increased their stride frequency up to 111% of their comfortable value, the increase in respectively backward and medio-lateral MoS would be, on average, 30% and 43% higher compared with the realized increase in backward and medio-lateral MoS for these trials.
|
Table II. Results of generalized estimating equations (GEE) analyses. GEE regression coefficients (β) and their 95% confidence interval (95% CI) for the effect of the imposed stride length and stride frequency, on the one hand, and the performed stride length, on the other hand, and for the effect of the performed stride length and stride frequency, on the one hand, and the backward margins of stability (MoS) and medio-lateral MoS, on the other hand. In these model both the imposed and actual stride length and stride frequency are expressed as the fraction of the comfortable value. In the case of non-significant factors in the original model, GEE analysis was repeated after removing these factors, resulting in the final model |
|||||
|
Parameter |
β [95% CI] |
p-value |
|||
|
Relative stride lengtha |
|||||
|
Intercept |
–0.357 [–0.490, –0.223] |
< 0.001* |
|||
|
Regression coefficient stride length (βSL) |
1.096 [1.003, 1.190] |
< 0.001* |
|||
|
Regression coefficient stride frequency (βSF) |
0.263 [0.190, 0.336] |
< 0.001* |
|||
|
Backward MoSb |
|||||
|
Intercept |
–0.442 [–0.543, –0.341] |
< 0.001* |
|||
|
Regression coefficient stride length (βSL) |
0.092 [0.063, 0.121] |
< 0.001* |
|||
|
Regression coefficient stride frequency (βSF) |
0.437 [0.343, 0.530] |
< 0.001* |
|||
|
Original model |
Final model |
||||
|
β [95% CI] |
p-value |
β [95% CI] |
p-value |
||
|
Medio-lateral MoSc |
|||||
|
Intercept |
0.015 [–0.011, 0.041] |
0.254 |
|||
|
Regression coefficient stride length (βSL) |
0.010 [–0.009, 0.029] |
0.306 |
|||
|
Regression coefficient stride frequency (βSF) |
0.030 [0.016, 0.044] |
< 0.001* |
0.054 [0.047, 0.061] |
< 0.001* |
|
|
*p < 0.05 level. aThe model used is: performed SLrel = intercept + βSL*imposed SLrel + βSF*imposed SFrel. bThe model used is: backward MoS = intercept + βSL*performed SLrel + βSF* performed SFrel. cThe model used is: medio-lateral MoS = intercept + βSL*performed SLrel + βSF* performed SFrel. |
|||||
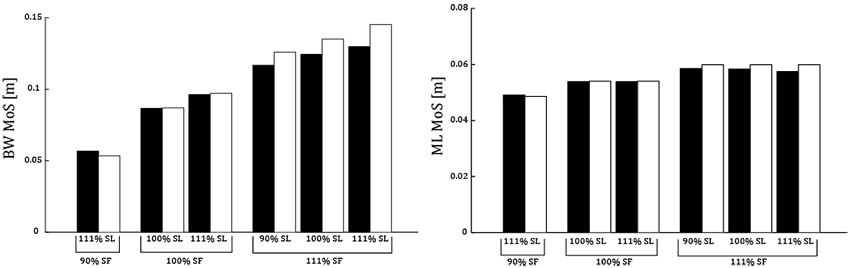
Fig. 4. Backward (BW) and mediolateral (ML) margins of stability (MoS) by using the regression equations: backward MoS = –0.442 + 0.092*SLrel + 0.437*SFrel and ML MoS = 0.054*SFrel (Table II). In these equations SLrel and SFrel are the relative stride length (SL) and stride frequency (SF), respectively. The black bars represent the BW and ML MoS as a result of the realized adaptations in SF and SL for the different trials. The white bars represent the BW and ML MoS as a result of the imposed adaptations in SF and SL for the different trials.
Discussion
The primary aim of this study was to investigate whether post-stroke participants can walk at different combinations of stride frequency and stride length, both at comfortable walking speed and higher than comfortable walking speed. Subjects were able to adjust stride length when required, and these adjustments in stride length were slightly larger than the imposed adjustments in stride length. However, subjects had difficulty adjusting their stride frequency when this was required. This was evident, as subjects also adjusted stride length when an adjustment in stride frequency only was imposed. For these trials adjustments in stride length were necessary to compensate for the reduced ability to adjust stride frequency, in order to maintain the imposed treadmill speed.
The second aim of this study was to investigate how adjustments in stride frequency, stride length, and the concomitant change in walking speed, influenced the size of the backward and medio-lateral MoS and whether potential difficulties in adaptations of stride frequency and length limit the increase in backward and medio-lateral MoS. Backward MoS increased with an increase in both stride frequency and stride length. However, considering the regression coefficients (0.437 corresponding to an increase in stride frequency and 0.092 corresponding to an increase in stride length), the increase in backward MoS as a result of an increase in stride frequency was almost 5 times larger than the increase in backward MoS as a result of a comparable increase in stride length. This finding is in accordance with previous findings in a group of able-bodied subjects (30). Both an increase in stride frequency and length coincide with an increase in walking speed, which has been demonstrated to be an important mechanism to increase the backward MoS (17, 30, 35). However, because of the negative effect of an increase in stride length itself on the backward MoS (17, 30, 35), a much larger increase in the backward MoS is achieved when the increase in walking speed is realized by an increase in stride frequency. An increase in medio-lateral MoS was only found with an increase in stride frequency.
Although backward and medio-lateral MoS in post-stroke individuals depend in a similar fashion on stride length, frequency and velocity as in able-bodied controls (30), the capacity of post-stroke individuals to regulate their MoS is limited due to a limitation in the capacity to increase stride frequency. For instance, because post-stroke individuals were not able to increase their stride frequency up to 111% of their comfortable stride frequency, the increase in respectively backward and medio-lateral MoS was, on average, 30% and 43% smaller than the increase in backward and medio-lateral MoS that could have been reached at the imposed stride frequency (Fig. 4). Hence, we can conclude that the limited increase in stride frequency in post-stroke individuals can have substantial consequences for the ability to increase backward and medio-lateral MoS. This lack of regulating MoS might increase the risk of losing balance in the medio-lateral or backward direction during walking in post-stroke individuals.
The results of this study were in line with results of previous studies in which it was found that an increase walking speed was mostly realized by an increase in stride length instead of an increase in stride frequency (36, 37). In addition, Roerdink et al. (38) found that some of the participating post-stroke individuals in their study had difficulties with adjusting stride frequency in response to auditory cueing. A potential explanation for the difficulty in increasing stride frequency might be that post-stroke individuals already walk at a relatively high stride frequency during comfortable walking compared with able-bodied controls (12, 36). However, impairments in the neuromuscular system (e.g. muscle spasticity, muscle weakness, reduced selectivity, etc.) could also play a role. The exact cause of the observed limitation in stride frequency adjustments, however, cannot be derived from this study, and requires further investigation.
The results of this study provide some clues that training the capacity to adjust step frequency in patients after stroke might result in improved ability to select a proper stepping strategy to regulate MoS and potentially reduce fall risk. Some indications can be found in the literature that training programmes in which gait adjustments are provoked are beneficial in terms of minimizing fall risk (39, 40). However, at this stage it cannot be concluded that the capacity to adjust gait can in fact be trained and that this training will have a direct effect on fall risk. Nevertheless, it would be of interest to study the effect of such a training programme on the capacity to regulate gait stability in challenging walking conditions, as previously used experimentally (12) and during daily life.
A limitation of this study is the estimation of the CoM as the mean of the markers attached to the LASI, RASI, LPSI, and RPSI of the pelvis to calculate the XCoM. It is possible that the post-stroke group has greater sway of the upper body, in which case this method could cause underestimation of the displacement of the XCoM, and therefore overestimation of the size of the MoS. However, from a study of De Bujunda et al. (11), it appears that, at least in the frontal plane, displacements and accelerations of the shoulders and pelvis during walking are very similar and therefore trunk mass moves in synchrony with the pelvis. This was the case for both post-stroke individuals and able-bodied controls. Therefore, we expect that the potential error made in the estimation of the CoM position in the current study will be small. In addition, potential mistakes in estimating the CoM location are probably systematic and would therefore not influence the within-subject differences between trials in which we were interested. A second limitation might be the relatively small and homogeneous group of subjects that participated in this study. Although their walking ability was clearly affected due to their stroke, all subjects were able to walk without a device during the experiment. Within this group the results were very consistent between subjects. However, this also implies that generalization of the results to groups with a more severe or mild stroke should be made with care.
In conclusion, the results of the present study indicate that post-stroke individuals have problems with increasing their stride frequency during walking. As a result, their capacity to increase the backward and medio-lateral MoS is also limited, which might place them at a higher risk of losing balance in the sideways and backward directions. It would be of interest to evaluate further the potential benefit of training stride frequency adjustments on fall risk in people after stroke.
Acknowledgements
The contribution of Laura Hak to this study was partly funded by Motek Medical b.v., but there was no contribution of Motek Medical b.v. to the content of this study. The authors wish to thank the Center for Augmented Motor Learning and Training form the National Military Rehabilitation Centre for their help with the data collection.
References
