Treatment of Palmoplantar Psoriasis with Monochromatic Excimer Light (308-nm) Versus Cream PUVA
Norbert J. NEUMANN, Natalia MAHNKE, Dorothea KORPUSIK, Helger STEGE and Thomas RUZICKA
Department of Dermatology, Heinrich-Heine-University Duesseldorf, Germany
Palmoplantar psoriasis is a chronic disease, which is very resistant to treatment and often leads to severe disabilities. Photochemotherapy employing psoralens combined with UVA irradiation (PUVA) is a well-accepted therapy for palmoplantar psoriasis. Its topical application (bath PUVA; cream PUVA) avoids the typical side effects of orally applied psoralens. We compared the efficacy of cream PUVA therapy with monochromatic excimer light therapy, a treatment modality employing 308-nm UVB radiation generated by a new kind of light source. Ten patients with psoriasis of the palms and soles were randomly assigned to receive cream PUVA on one side and 308-nm UVB on the contralateral side. Based on the psoriasis area and severity index (PASI) score, clinical assessment was carried out before and 5 weeks after the beginning of the study. At the end of the treatment period both test groups showed a remarkable PASI score reduction (308-nm UVB, 63.57%; cream PUVA, 64.64%). No relevant adverse effects were observed, except for mild irritation in a few patients. After a 12-week follow-up, a relapse of the disease was only observed in one patient. Thus, mono-chromatic excimer light cleared palmoplantar psoriasis as rapidly as cream PUVA. In contrast to cream PUVA, monochromatic excimer light therapy is not associated with prior drug application. This might lead to a lower incidence of adverse reactions and better compliance. Therefore, monochromatic excimer light therapy seems to be a useful new therapeutic option for palmoplantar psoriasis. Key words: psoralens; UVB: UVA; psoriasis.
(Accepted April 12, 2005.)
Acta Derm Venereol 2006; 86: 22–24.
Dr N. J. Neumann, Department of Dermatology, Heinrich- Heine-University, Moorenstrasse 5, 40225 Duesseldorf, Germany. E-mail: neumannt@uni-duesseldorf.de
Chronic palmoplantar psoriasis is an idiopathic condition located on palms and soles and characterized by erythema, scaling and fissuring. Although palmoplantar psoriasis appears to be a distinct entity in terms of
epidemiology and pathophysiology, it might be associated with other forms of psoriasis. Palmoplantar psoriasis may affect people of all ages. Once established, it might last for decades and can cause impaired dexterity or mobility, as well as discomforting pruritus and pain.
Photochemotherapy employing psoralens combined with UVA irradiation (PUVA) is a well-accepted therapy for palmoplantar psoriasis and topical application (bath PUVA; cream PUVA) avoids the typical side effects of systemically administered psoralens.
Recently, it was demonstrated that an excimer laser-generated 308-nm UVB radiation might be an effective treatment modality for psoriasis (1, 2). Additionally, Campolmi et al. (3) reported the efficacy of monochromatic excimer light (MEL) in palmoplantar psoriasis. The aim of our study was to compare the efficacy of cream PUVA photochemotherapy with 308-nm monochromatic excimer light in the treatment of palmoplantar psoriasis.
PATIENTS AND METHODS
Ten patients (six men and four women, age range 11–71, mean age ± SD 47.3 ± 8.37 years) with clinically and histologically defined plaque-type palmoplantar psoriasis were enrolled and randomized in this study. No patient was treated with photochemotherapy or systemic psoriasis treatments before and the participants were required to discontinue any topical treatment for at least 1 month before enrolment.
The individual minimal erythema dose (MED) of mono- chromatic UVB (308 nm) was determined in all patients on parts of the lower back prior to the study and 70% of the MED-MEL was used as initial MEL dosage.
Investigator-blinded clinical evaluation was performed weekly during 5 study weeks as well as during a 12-week follow-up after the end of the study. Following a random left/ right trial design, palmae or plantae were irradiated with MEL (308 nm) (starting from 0.75 J/cm2 up to 4.5 J/cm2) or treated with cream PUVA (starting from 0.5 J/cm2 up to 8 J/cm2) four times a week.
Photochemotherapy employing 8-MOP combined with UVA irradiation
Psoralen was administered topically as a cream preparation: Meladinine solution 0.03% in Ungentum cordes. The cream was applied 1 hour before UVA irradiation. Polychromatic (315–400 nm) UVA irradiation was applied by UV 181 AL (feet) and UV 200 AL (hands). Both light sources were manufactured by Waldmann (Villingen-Schweinningen, Germany), irradiating a power density of 36 W (UV 181 AL) or 8 W (UV 200 AL), respectively.
Monochromatic excimer light (308 nm)
The 308-nm XeCl MEL (Excilite–Deka, Florence, Italy) produces a power density of 48 mW/cm2 at a source-to-skin distance of 15 cm (maximum irradiated area: 512 cm2).
PASI score
The baseline severity of the palmoplantar psoriasis was measured using a modified psoriasis area and severity index (PASI) score based on the characteristics of target lesions. Since it was first described in 1978, PASI has been a widely utilized tool for the objective evaluation of psoriasis (4). The modified PASI score ranges from 0 to 60 on a scale
representing the proportion of area involved and the severity of erythema, infiltration and desquamation, ranking from 0 (normal) to 4 (severe). Additionally the affected area is registered and – according to the expansion – valued in score points from 0 to 5 points. The proportion of area involved:
area in %: 0 = 0; 1–20 = 1; 21–40 = 2; 41–60 = 3; 61–80 = 4; 81–100 = 5 score points. PASI score = affected surface area in patients with palmoplantar psoriasis (erythema+infiltration+desquamation). The PASI score can reach a maximum of 60 points [5×(4+4+4)].
Statistical analysis
To compare PASI score distributions in both test sites (MEL vs cream PUVA), the Wilcoxon test for two paired samples was employed.
RESULTS
At the start of the study there were no significant differences between the PASI score distribution in the respective treatment sites (p≤0.317). All patients randomly
treated half-sided with 308-nm MEL or 8-MOP-cream PUVA showed a clinical improvement evidenced by flattening of plaques and decreased scaling, starting after four to eight treatments (1–2 weeks) (Tables I and II; Fig. 1). At the end of the trial period, the mean PASI scores were reduced from 28.00 ( ± 18.74 SD) to 10.20 (± 12.20 SD) in the MEL and from 26.30 ( ± 19.60 SD)
to 9.30 ( ± 9.43 SD) in the cream PUVA group. At the end of the fifth week no significant differences of the PASI score reduction resulted from comparison of both study groups (p≤0.581).
Accordingly, the mean PASI scores were significantly decreased in both treatment sites (MEL, 63.57%; cream PUVA, 64.64%).
Table I. Individual PASI scores during treatment with monochromatic excimer light (308 nm)
Patient 1 2 3 4 5 6 7 8 9 10 X ( ± SD)
AOT RP RS RP LP RS RS LS LP RP RS
Start 24 6 21 12 50 32 4 27 44 60 28 ( ± 18.74)
Week 1 12 6 21 10 45 30 4 27 32 60 24.7 ( ± 17.99)
Week 2 12 4 15 8 45 20 2 18 32 45 20.1 ( ± 15.67)
Week 3 6 4 12 4 35 20 2 18 15 35 15.1 ( ± 12.18)
Week 4 6 2 10 4 40 12 1 6 12 30 12.3 ( ± 12.77)
Week 5 6 0 10 0 40 12 0 6 8 20 10.2 ( ± 12.20)
AOT: area of treatment, RP: right palm, LP: left palm, RS: right sole, LS: left sole.
Side effects
Three patients developed an erythema in skin areas treated with MEL. Erythema and mild irritation were recorded in palmae or plantae of four patients treated with cream PUVA. No relevant phototoxic or photo- allergic reactions were observed in any treated skin area. After a 12-week follow-up, a relapse of the disease was only observed in one patient on both test sites.
Table II. Individual PASI scores during treatment with cream PUVA
Patient 1 2 3 4 5 6 7 8 9 10 X ( ± SD)
AOT LP LS LP RP LS LS RS RP LP LS
Start 24 6 21 12 50 32 4 10 44 60 26.3 ( ± 19.60)
Week 1 12 3 15 8 45 30 4 10 32 60 21.9 ( ± 19.18)
Week 2 12 3 10 6 35 20 2 6 32 35 16.1 ( ± 13.38)
Week 3 12 3 10 4 35 20 2 6 15 35 14.2 ( ± 12.33)
Week 4 6 1 10 4 30 12 1 2 12 30 10.8 ( ± 9.30)
Week 5 6 1 10 4 30 12 0 2 8 20 9.3 ( ± 9.43)
AOT: area of treatment, RP: right palm, LP: left palm, RS: right sole, LS: left sole.
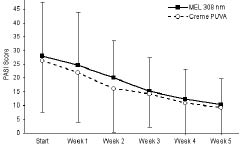
Fig. 1. Mean PASI scores (+ or – SD) during treatment with cream PUVA and monochromal excimer light (MEL; 308 nm).
DISCUSSION
Photochemotherapy employing psoralen combined with UVA irradiation has been shown to induce remission in palmoplantar psoriasis (5). Disadvantages of systemic PUVA treatment include nausea, pruritus and the need to protect skin and eyes from sunlight during and beyond the treatment days. Topically applied methoxy-psoralen (8-MOP) in ointment avoids the systemic side effects of oral psoralens and induces a significantly decreased time course of phototoxicity after irradiation with UVA (6). However, cream PUVA treatment sometimes leads to an acute phototoxic dermatitis or itching and long-term treatment is associated with an increasing risk of skin cancer. Previously it was demonstrated that wavelengths between 300 and 313 nm have therapeutic effects on psoriasis (7) and that narrowband UVB
(311 nm) phototherapy is an effective treatment in psoriasis (8). The efficiency of the new 308-nm mono-chromatic excimer source – with an emission close to that used in narrowband UVB phototherapy – was described in the treatment of palmoplantar psoriasis (3). The application of MEL may present some advantages
compared with laser therapy: lower power density with a consequently reduced risk of accidents due to over-
exposure and a wider irradiation field leading to the option to treat larger skin areas at a time. The
contraindications and risks of MEL treatment (short- term and long-term) are supposed to be comparable to narrowband UVB. Narrowband UVB can cause derma-
titis solaris in short-term therapy while long-term exposure might cause skin ageing and skin cancers. Although the complete spectrum of side effects of
narrowband UVB is still unknown (9), does not seem to be more hazardous than broadband UVB (10) and is pro-bably less hazardous than PUVA photochemotherapy.
All patients showed clinical improvement after four to eight sessions (1–2 weeks) of cream PUVA or MEL phototherapy in our open study design. Due to the different treatment modalities and the use of dissimilar UV sources made it impossible to blind the patients. However, all readings were performed investigator-blinded. Based on the suggestion of Carlin et al. (11) that a PASI score reduction of 50% corresponds to a clinically significant endpoint in assessment of psoriasis, a mean PASI score reduction of more than 60% in both our study groups represents a remarkable clinical improvement. After a 12-week follow-up, a relapse of the disease was observed in only one patient. MEL cleared skin lesions of palmoplantar psoriasis as rapidly as cream PUVA photochemotherapy and was as efficacious as cream PUVA treatment. However, MEL treatment is easier to perform and therefore it might lead to better compliance. Thus, our results indicate that MEL therapy might be a valuable new treatment option for palmoplantar psoriasis.
REFERENCES
1. Asawanonda P, Anderson R, Chang Y, Taylor CR. 308 nm excimer laser for the treatment of psoriasis: a dose-response study. Arch Dermatol 2000; 136: 619–624.
2. Kemery L, Bonis B. 308-nm excimer laser therapy for psoriasis. Arch Dermatol 2001; 137: 95.
3. Campolmi P, Mavilia L, Lotti TM, Rossi R, Brazzini B, Hercogova J, et al. 308 nm monochromatic excimer light for the treatment of palmoplantar psoriasis. Int J Immunopathol Pharmacol 2002; 13: 11–13.
4. Feldman SR. A quantitative definition of severe psoriasis for use in clinical trials. J Dermatol Treat 2004; 15: 27–29.
5. Stege H, Berneburg M, Ruzicka T, Krutmann J. Cream PUVA photochemotherapy. Hautarzt 1997; 48: 89–93.
6. Neumann NJ, Ruzicka T, Lehmann P, Kerscher M. Rapid decrease of phototoxicity after PUVA bath therapy with 8-methoxypsoralen. Arch Dermatol 1996; 132: 1394.
7. Parrish JA, Jaenicke KF. Action spectrum for phototherapy of psoriasis. J Invest Dermatol 1981; 76: 359–362.
8. Green C, Ferguson J, Lakshmipathi T, Johnson BE. 311 nm UVB phototherapy—an effective treatment for psoriasis. Br J Dermatol 1988; 119: 691–696.
9. El-Ghorr AA, Norval M. Biological effects of narrowband (311 nm TL01) UVB irradiation: a review. J Photochem Photobiol B 1997; 38: 99–106.
10. Berneburg M, Röcken M, Bendix F. Phototherapy with narrowband versus broadband UVB. Acta Derm Venereol 2005; 85: 98–108.
11. Carlin CS, Feldman SR, Krueger JG, Menter A, Krueger GG. A 50% reduction in the Psoriasis Area and Severity Index (PASI 50) is a clinically significant endpoint in the assessment of psoriasis. J Am Acad Dermatol 2004; 50: 859–866.
