Yasushi Sugimoto, Eri Araki, Naoko Inoguchi, Yumi Matsumura, Satoshi Kore-eda, Yuji Horiguchi, Yoshiki Miyachi and Atsushi Utani*
Department of Dermatology, Kyoto University Graduate School of Medicine, 54 Kawahara-Cho, Shogoin, Sakyo-Ku, Kyoto 606-8507, Japan. *E-mail: utani@kuhp.kyoto-u.ac.jp
Accepted October 16, 2006.
Sir,
Eccrine angiomatous hamartoma (EAH) is a rare benign hamartoma of eccrine glands and blood vessels. It most commonly develops before adulthood as a single, slow-growing lesion on the extremities. We describe here a case of adult-onset EAH with generalized multiple hairy reddish-brown indurated plaques with a rapidly progressive course. As the lesions showed histopathological findings such as an increase in mature eccrine glands and blood vessels, the diagnosis was determined to be EAH. This case was observed carefully because the lesion had characteristics not only of a hamartoma but also of a tumour.
CASE REPORT
A 40-year-old man presented with a 5-year history of multiple enlarging plaques on his trunk and extremities. The first lesion appeared on his right thigh as a reddish-brown plaque. Within one year of onset, new plaques and nodules began to develop on his trunk and other extremities. All of the lesions increased in size continuously. Some were associated with occasional stabbing pain, but otherwise they were asymptomatic. Physical examination revealed as many as 15 reddish-brown plaques and flat nodules over the patient’s chest, abdomen, back, buttock, left axilla, legs, arms, and left dorsal hand with or without mild hypertrichosis (Fig. 1). Some lesions showed moderate indurations. At a 2-year follow-up visit, all lesions showed considerable enlargement. The 2 indurated plaques on the upper back had grown into a single fused large plaque of ~25×50 cm. Some lesions that initially were only mildly hypertrichotic had even more thickened hair (Fig. 1).
Fig. 1. Clinical appearance of the reddish-brown plaques on: (A) left dorsal hand; (B) medial side of the right forearm; (C) buttock, and; (D) right upper back. The lesions in (A) and (B) show aggressive enlargement and more severe hypertrichosis after 2 years of observation (A(2y), B(2y)).

Biopsied specimens taken from lesions on the right forearm demonstrated increased well-differentiated sweat glands and partially dilated vascular channels in the deeper dermis (Fig. 2). Two types of blood vessel proliferation were noted: one with thick walls as seen in cavernous haemangioma and the other with thin walls like those of capillary haemangioma (Fig. 2B and C). Abundant mucin deposition surrounded the proliferating units of eccrine glands and vessels (Fig. 2C). Mild acanthosis, focal inflammation and fibrosis in the deep dermis and subcutaneous tissues were also noted (Fig. 2A). Granulomas with epidermal cells, neutrophils and mononuclear cells, indicating destruction of hair follicles, were found in the other set of biopsied specimens (Fig. 2D), which may be related to increased hairs in the lesions. A dense inflammatory infiltrate is not usually seen in an EAH, and represents a unique finding in this case. Repeated cultures of biopsied samples showed no growth of fungi, mycobacteria or bacteria, suggesting that inflammation was not caused by infection.
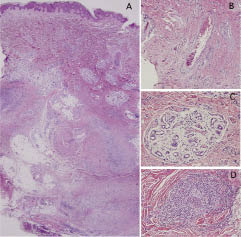
Fig. 2. Histopathology. (A, B, C) Proliferation of sweat glands and blood vessels with thick or thin walls. (A) Focal inflammatory cell infiltrations and diffuse fibrosis in the deep dermis and subcutaneous tissues were observed. (C) Mucin deposits within a nest of proliferated eccrine glands and blood vessels. (D) Granulomas with epidermal cells, neutrophils and mononuclear cells in the dermis. Haematoxylin-eosin staining of the specimens from the lesion on the right forearm. Original magnification, (A) ×12.5; (B) ×100; (C, D) ×200.
DISCUSSION
The clinical phenotype of EAH has been reviewed recently (1–3). To date, 46 cases of EAH have been reported, excluding the present case. EAH predominantly has a single lesion (34 of 47 cases, 72%). Commonly associated symptoms are pain, hyperhidrosis, and hypertrichosis. The lesion presents more often on the extremities (approx. >70%) than on the trunk. Thirty-five of 47 cases (74%) developed before adulthood. In the present case, the combination of the following features of EAH was unique: multiple lesions; adult-onset; a rapid growth of the lesions; and the presence of extremely large plaques on the back.
We found 12 cases of multiple EAH in the literature (3–10). No significant difference in onset age was observed between multiple and single EAH. In the 2 cases of adult-onset multiple EAH, both had lesions limited to the dorsa of fingers (4) or the lower leg (5). There were 2 generalized cases with more than 10 lesions on the whole body (3, 6), both with congenital onset. Our patient is the first reported case of generalized EAH that developed in adulthood. The aetiology of EAH is not known, but the mechanism of spreading multiple EAH to several parts of body may be due to mosaicism of a gene mutation occurring in the early developmental stage.
Because malignant degeneration of EAH has not been reported, simple excision is usually chosen as a curative treatment for small lesions of EAH. However, it cannot be chosen in this case because of the number and size of lesions and because of deep skin involvement. Our patient is now being treated with oral analgesics to relieve stabbing pain of his left hand lesion. This case should be observed carefully because the lesion has characteristics not only of a hamartoma but also of a tumour. Surgical removal of lesions in the present case must be considered when the hamartomas perturb joint movement or provoke severe pain by involvement of surrounding peripheral nerves or cosmetic problems.
REFERENCES
1. Pelle MT, Pride HB, Tyler WB. Eccrine angiomatous hamartoma. J Am Acad Dermatol 2002; 47: 429–435.
2. Martinelli PT, Tschen JA. Eccrine angiomatous hamartoma: a case report and review of the literature. Cutis 2003; 71: 449–455.
3. Garcia-Arpa M, Rodriguez-Vazquez M, Cortina-de la Calle P, Romero-Aguilera G, Lopez-Perez R. Multiple and familial eccrine angiomatous hamartoma. Acta Derm Venereol 2005; 85: 355–357.
4. Cebreiro C, Sanchez-Aguilar D, Gomez Centeno P, Fernandez-Redondo V, Toribio J. Eccrine angiomatous hamartoma: report of seven cases. Clin Exp Dermatol 1998; 23: 267–270.
5. Seraly MP, Magee K, Abell E, Bridenstine J, Jegasothy BV. Eccrine-angiomatous nevus, a new variant. J Am Acad Dermatol 1993; 29: 274–275.
6. Aloi F, Tomasini C, Pippione M. Eccrine angiomatous hamartoma: a multiple variant. Dermatology 1992; 184: 219–222.
7. Nair LV, Kurien AM. Eccrine angiomatous hamartoma. Int J Dermatol 1994; 33: 650–651.
8. Sulica RL, Kao GF, Sulica VI, Penneys NS. Eccrine angiomatous hamartoma (nevus): immunohistochemical findings and review of the literature. J Cutan Pathol 1994; 21: 71–75.
9. Morrell DS, Ghali FE, Stahr BJ, McCauliffe DP. Eccrine angiomatous hamartoma: a report of symmetric and painful lesions of the wrists. Pediatr Dermatol 2001; 18: 117–119.
10. Lee SY, Chang SE, Choi JH, Sung KJ, Moon KC, Koh JK. Congenital eccrine angiomatous hamartoma: report of two patients. J Dermatol 2001; 28: 338–340.
