Jacob Pontoppidan Thyssen1, Marianne Hald1, Christian Avnstorp2, Niels Kren Veien2, Grete Lauerberg2, Niels Henrik Nielsen2, Knud Kaaber2, Berit Kristensen2, Ove Kristensen2, Jens Thormann2, Susanne Vissing2, Torkil Menné3 and Jeanne Duus Johansen1
1National Allergy Research Centre, Gentofte University Hospital, Gentofte, 2Danish Contact Dermatitis Group, and 3Department of Dermatology, Gentofte University Hospital, Hellerup, Denmark
The use of nickel in certain consumer goods has been regulated in Denmark since 1990. The aim of this study was to reveal the clinical characteristics of nickel-allergic patients seen in seven private dermatology clinics and to identify current sources of nickel that may elicit nickel dermatitis. During 2006 to 2007, 634 patients with dermatitis aged 17–91 years were patch-tested and completed a questionnaire including a question about the occurrence of dermatitis following skin contact with ear-rings or ear-pins, watches, buttons or metal clasps (i.e. metal dermatitis). χ2 tests were applied to test for statistical significant differences. Analysis revealed a lower prevalence of nickel allergy among women in the youngest age group (17–22 years) in comparison with older age groups (23–34 years and 35–46 years) (p < 0.03). Most patients experienced metal dermatitis on the first occurrence between 1975 and 1985. No new cases of metal dermatitis were identified after 1985. We conclude that nickel allergy has decreased among young females with dermatitis due to the nickel regulation. Key words: nickel; hand eczema; occupational dermatitis; risk factor; sensitization; allergy; regulation.
(Accepted December 4, 2008.)
Acta Derm Venereol 2009; 89: 384–388.
Jacob Pontoppidan Thyssen, National Allergy Research Centre, Department of Dermatology and Allergology, Gentofte University Hospital, Ledreborg Allé 40, 1, DK-2820 Gentofte, Denmark. E-mail: jacpth01@geh.regionh.dk
In the late 20th century, a nickel allergy epidemic was observed in Denmark (1–6). To reduce nickel allergy, the government passed the Danish nickel regulation in 1990 (7), which prohibited certain consumer products (e.g. jewellery, spectacles, buttons and belt buckles), which were intended to come into direct and prolonged contact with the skin, if they released more than 0.5 µg nickel/cm2/week. So far, a decreasing prevalence of nickel allergy has been observed among patients with dermatitis as well as among Danish schoolgirls (8–10). At present, we assume that the majority of positive patch test reactions to nickel are caused by sensitization before 1990 (i.e. before the nickel regulation was passed). However, nickel allergy may still occur as a consequence of exposure to consumer items not covered by the nickel regulation (11, 12), or due to exposure to personally imported goods (13), or due to occupational nickel exposure. To our knowledge, there are very few published data that identify present-day consumer goods that may cause nickel dermatitis in nickel-allergic patients. Such data are of interest as they may indicate potential sources of nickel exposure that should be addressed in order to further limit nickel exposure in Denmark.
This study was performed in seven private dermatology clinics in Denmark. The aim was to reveal present-day characteristics of nickel-allergic dermatitis patients and to compare them with those of patients with dermatitis who are not allergic to nickel. Furthermore, we sought to identify current metal exposures that may lead to nickel dermatitis. Finally, we aimed to briefly discuss the effects of the Danish nickel regulation. This is of general interest among European dermatologists and policymakers, as the 1994 European Union (EU) Nickel Directive (Table I) was based on the Danish regulation (14, 15).
Table I. European Union Nickel Directive (14, 15)
| 1 | Original requirement (before 2005): Nickel was prohibited in post-assemblies used during epithelialization after piercing, unless they were homogenous and the nickel concentration was less than 0.05%. New requirement from 2005: Nickel release from all items inserted into pierced parts of the body (not only during epithelialization after piercing) should be less than 0.2 µg/cm2/week. |
| 2 | Nickel may not be used in products intended to come into direct and prolonged contact with the skin, such as ear-rings, necklaces, finger rings, spectacles, wristwatches, buttons if nickel release from the parts coming into direct and prolonged contact with the skin is greater than 0.5 µg/cm2/week. |
| 3 | Nickel is prohibited in products such as those listed under point 2 if they have a coating and if they do not fulfil the requirement under point 2 for a period 2 years of normal use. |
MATERIALS AND METHODS
Case identification and patch testing
Between June 2006 and January 2007, 634 consecutive patients with dermatitis (i.e. patients with dermatitis in whom contact allergy was suspected) above 17 years of age (17–91 years) were invited to participate in a study performed in seven private dermatology clinics in Jutland and Sealand, Denmark, representing urban and rural areas. Dermatologists registered the clinical profile of the patient’s eczema (i.e. using the MOAHLFA index), performed patch testing and collected questionnaires. No information was obtained about the number and characteristics of non-participants, but the overall participation-rate was high in all clinics as it was a short questionnaire. The European baseline patch test series (Almiral Hermal Gmbh, Reinbek, Germany or Chemotechnique, Malmö, Sweden) were used for testing in five clinics, whereas the TRUE-test® (Mekos Laboratories, Hilleroed, Denmark) was used in two clinics. The concordance rate between the test systems is generally high for reactions to nickel but low for reactions to cobalt (16–18). Patches were applied on the upper back and left for 2 days. Readings were performed on either day 2 or day 3 and in the majority of patients also on day 5 or day 7 using the International Contact Dermatitis Research Groups (ICDRG) criteria (19). A positive reaction (1+) was defined as at least homogenous redness and palpable infiltration in the test area. Reactions not fulfilling these criteria, whether these were follicular reactions, faint erythema, or typical irritant reactions, were classified as non-allergic reactions.
Questionnaire
All participants completed a short questionnaire including questions about nickel exposure and dermatitis following exposure to consumer goods with a metallic surface. Patients were asked: “Have you ever had an eczema reaction following skin contact with ear-rings or ear-pins, watches, buttons or metal clasps?” (“yes”, “no”). Patients who gave an affirmative answer were further asked: “If yes, how old were you at the first occurrence?”. The response was later used to calculate the year of first occurrence of metal dermatitis. In addition, patients who gave an affirmative answer were asked: “If yes, which metal items have lead to dermatitis on the most recent occurrence?” (“ear-ring/ear-pin”, “other jewellery”, “watch”, “buttons”, “spectacles”, “belt buckles”, “other”). Finally, patients who responded “other” were asked to specify causative items.
Statistical analysis
Positive nickel patch tested patients with dermatitis were compared with a group of nickel patch test negative patients with dermatitis. The χ2 test (and where appropriate the Fisher’s exact test) was used for testing independence of categorical variables. Statistical results were expressed as odds ratios (ORs) with 95% confidence intervals (95% CI) and were considered significant if p-values were below 0.05. The population was not normally distributed as assessed by Kolmogorov-Smirnov test (p < 0.014). The histogram was skewed to the left with a significant proportion of younger individuals. Finally, an independent-sample t-test was performed to compare the mean age of patients with and without nickel sensitization. Data analysis was performed using the Statistical Products and Service Solutions package (SPSS Inc., Chicago, IL, USA) for Windows (release 15.0).
RESULTS
Table II shows the baseline characteristics of 634 consecutive dermatitis patients stratified by patch-test response to nickel. A total of 117 (18.5%) patients had a positive patch test reaction to nickel. The mean age ± standard deviation (SD) was lower among nickel-allergic patients (42.1 ± 2.6 years) than among patients without nickel allergy (47.3 ± 1.6 years) (p < 0.001). Furthermore, nickel allergy occurred more often in female patients than in male patients (OR = 6.69; CI 95% = 3.31–13.51). Cobalt allergy was observed in 33 patients (5.2%), whereas combined nickel and cobalt allergy was observed in 21 (3.3%) patients. As cobalt allergy did not alter the outcome of the statistical analyses, cobalt allergy was excluded from these. A stratification by age in women showed that the prevalence of nickel allergy was 14.6% (6/41) among 17–22 year-olds; 31.8% (34/107) among 23–34 year-olds; 31.9% (36/113) among 35–46 year-olds, 27% (20/74) among 47–58 year-olds and 11.4% (12/105) among 59–91 year-olds. A comparison of women in the youngest age groups (i.e. 17–22 year-olds) with women in older age groups (i.e. 23–34 year-olds and 35–46 years-olds, respectively) revealed a significant difference (p < 0.03).
Table II. Baseline characteristics of 634 consecutive eczema patients stratified by patch test response to nickel. Univariate analysis (χ2-test and, where appropriate, Fisher’s exact test) were used to test for statistical differences between nickel patch test positive and negative patients
| Frequency of variables | Total % (n) | Nickel patch test positive patients (n = 117) % (n) | Nickel patch test negative patients (n = 517) % (n) | Odds ratio (95% CI)c |
| Cobalt sensitization | 5.2 (33) | 17.9 (21) | 2.3 (12) | 9.20 (4.38–19.34) |
| MOAHLFA indexa |
| Males | 30.6 (194) | 7.7 (9) | 35.8 (185) | 0.15 (0.07–0.30) |
| Occupational dermatitis | 11.4 (72) | 18.8 (22) | 9.7 (50) | 2.16 (1.25–3.74) |
| Atopy | 14.7 (93) | 19.7 (23) | 13.5 (70) | 1.56 (0.92–2.63) |
| Hand dermatitis | 38.2 (242) | 45.3 (53) | 36.6 (189) | 1.48 (0.99–2.23) |
| Leg ulcers | 1.7 (11) | 0.9 (1) | 1.9 (10) | 0.44 (0.05–3.45) |
| Facial dermatitis | 18.5 (117) | 22.2 (26) | 17.6 (91) | 1.34 (0.81–2.20) |
| Age > 40 years | 61.8 (392) | 53 (62) | 63.8 (330) | 0.64 (0.42–0.96) |
| Age < 40 years | 38.2 (242) | 47 (55) | 36.2 (187) | 1.56 (1.04–2.35) |
| Females | 69.4 (440) | 92.3 (108) | 64.2 (332) | 6.69 (3.31–13.51) |
| Metal dermatitisb | 36.3 (230) | 74.4 (87) | 27.8 (143) | 7.91 (4.92–12.70) |
| Metal dermatitis before 1990 | 19.1 (121) | 44.4 (52) | 13.3 (69) | 5.47 (3.52–8.52) |
| Metal dermatitis later than 1990 | 8.9 (57) | 18.8 (22) | 6.7 (35) | 2.85 (1.53–5.30) |
aThe MOAHLFA index stands for Male, Occupational dermatitis, Atopic dermatitis, Hand dermatitis, Leg ulcers, Facial dermatitis and Age above 40 years. It shows the characteristics of patients tested at a patch test clinic and may be used for comparison (39).
bHave you ever experienced eczema from skin contact with ear-rings or ear-pins, watches, buttons or metal clasps?
cOdds ratio for the comparison of nickel patch test positive patients and nickel patch test negative patients.
CI: confidence interval.
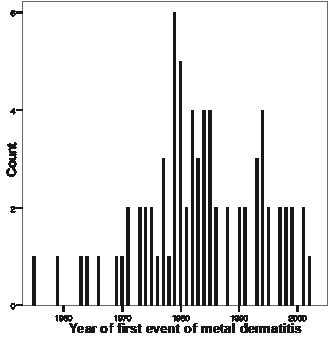
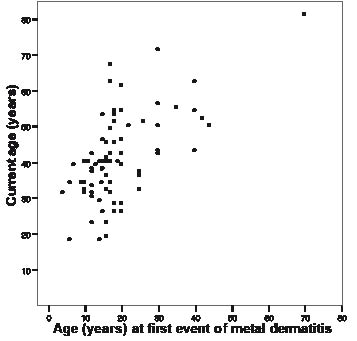
Metal dermatitis (i.e. lifetime event of eczema from skin contact with ear-rings or ear-pins, watches, buttons or metal clasps) was more often reported among nickel-allergic patients than among patients without nickel allergy (OR = 7.91; 95% CI = 4.92–12.70). There was no statistical significance in the frequency of metal dermatitis between female and male nickel-allergic patients. A stronger association was identified among patients who reported metal dermatitis before 1990 (OR = 5.47; 95% CI = 3.52–8.52) than among patients who reported metal dermatitis later than 1990 (OR = 2.85; 95% CI = 1.53–5.30) (Table II). Fig. 1 shows that most nickel-allergic patients experienced their first event of metal dermatitis (response rate 63%) between 1975 and 1985, although a few reported symptoms as early as 1955 and as late as 2002. Fig. 2 shows the correlation between the age of nickel-allergic eczema patients in 2007 and their age at first occurrence of metal dermatitis. Most patients were between 10–30 years of age at their first event of metal dermatitis. However, some 40–70 year-olds reported their first occurrence of metal dermatitis at an older age.
Fig. 1. Self-reported year of first event of metal dermatitis among nickel-sensitized dermatitis patients (eczema from skin contact with ear-rings or ear-pins, watches, buttons or metal clasps) (n = 74).
Fig. 2. Correlation between “current age” of dermatitis patients (i.e. age in 2007) and “the age at first event of metal dermatitis” (eczema from skin contact with ear-rings or ear-pins, watches, buttons or metal clasps).
Metal dermatitis to watches (n = 45), ear-rings or ear-pins (n = 44), buttons (n = 42), jewellery (n = 31), belt buckles (n = 29) and metal frames from spectacles (n = 15) were frequently reported in both sexes as items that caused metal dermatitis in the most recent occurrence. However, women reported metal dermatitis to ear-rings or ear-pins in the most recent occurrence significantly more often than men (OR = 1.69; 95% CI = 1.44–1.97). Other reported exposures included mascara, coins, jewellery, buttons, belts, tools and mobile phones. Except for coins, participating dermatologists reported the same variety of causative and relevant nickel exposures.
DISCUSSION
This investigation revealed some important characteristics of nickel-allergic patients seen in private dermatology clinics in Denmark: they were often women and had a younger mean age compared with those without nickel allergy (Table II). A stratification by age among female patients showed that the prevalence of nickel allergy was significantly lower among 17–22 year-olds compared with older age groups (i.e. 23–34 year-olds and 35–46 year-olds, respectively). The higher prevalence observed among older age groups of women may be explained by a cohort effect (i.e. patients who were mainly sensitized to nickel prior to 1990 have aged but remain sensitized). These findings are in accordance with the outcome of one previous longitudinal study performed in a private dermatology clinic in Denmark (10).
This study also showed that nickel-allergic patients reported “metal dermatitis” significantly more often than patients without nickel sensitization (Table II). Since the prevalence of cobalt allergy was similar in the two groups, answers to this question may be used to assess the occurrence of nickel dermatitis. The majority of nickel-allergic patients reported that their first occurrence of metal dermatitis was in the 1970s and 1980s (Fig. 1) and that they were in their teens at the time (Fig. 2). However, a few older patients (current age 40–70 years) reported that they experienced their first event of metal dermatitis in their 30s to 50s (corresponding decades therefore mainly included the 1970s and 1980s). Since nickel-allergic patients were relatively young (mean age 41.1 years) and the age distribution was skewed to the left, exposure to piercing and inexpensive jewellery, for example, must have happened within relatively recent years (i.e. 10–30 years ago). If no nickel regulation had been passed in Denmark, we hypothesize that the reported “year of first event of metal dermatitis” would have been more spread out to recent years and not concentrated around 1980. Furthermore, the results shown in Fig. 1 may have been influenced by recall bias, since some patients may rather remember recent events than events in the distant past. Taken together, these results suggest a general decrease in metal dermatitis among nickel-allergic patients, although no significant difference could be identified between patients who reported metal dermatitis before 1990 and patients who reported metal dermatitis later than 1990.
Cases of metal dermatitis occurring later than 1990 may be explained by occupational nickel exposure (20) as well as consumer nickel exposure (i.e. to items not included in the legislation, such as mobile phones (11), personally imported jewellery from countries without nickel regulations (13, 21, 22), jewellery purchased in EU countries before the EU Nickel Directive came into full force in 2001 (23), or items sold from vendors not following the Danish nickel regulation and EU Nickel Directive (Table I) (24–26)). Finally, the Danish nickel regulation does not completely prevent nickel dermatitis, as approximately 5% of a sensitized population may react to an occluded (e.g. wrist watch and buttons) dose of 0.44 µg nickel/cm2 per week (27). The combination of our results and those from previous Danish studies (8–10) indicate the beneficial effects of the Danish nickel regulation. A working group within the Danish Environmental Agency has estimated that the regulation has reduced the direct and indirect society costs due to nickel dermatitis by approximately 2 billion US$ over a 20-year period (28). In Germany, a decreasing prevalence of nickel allergy has also been demonstrated, possibly due to the EU Nickel Directive (Table I) (29). In Poland, a country that recently entered the EU, the proportion of patients aged 0–20 years decreased significantly among nickel dermatitis patients between 1995 and 2004 (30). The authors speculated that the decrease was a result of the close economic ties to the EU. Of interest, the prevalence of nickel allergy seems to increase in the USA among patients with dermatitis (31–33). This may be explained by excessive nickel release (i.e. < 0.5 µg/cm2/week) from, for example, jeans buttons, belt buckles and ear-rings (13, 21, 22). Similarly, in Taiwan, a country that does not regulate consumer nickel exposure, an increase in the prevalence of nickel allergy among patients with dermatitis has been observed since 1978 (34).
Among nickel-allergic patients, almost all categories of metal items were frequently reported as causing metal dermatitis on the most recent occurrence, i.e. watches, ear-pins, buttons, jewellery, belt buckles and metal frames from spectacles. Only a few patients mentioned mascara, coins, tools and mobile phones. Participating dermatologists reported the same items (except for coins). It has been repeatedly discussed whether the handling of coins can elicit contact dermatitis in nickel-allergic individuals (35–37). So far, no general consensus has been reached, but many dermatologists agree that normal handling of coins does not lead to nickel dermatitis, whereas repeated occupational exposure to nickel from coins in some cases may elicit nickel dermatitis (37). Potential sources of nickel exposure, such as mobile phones and work tools, may, in some cases, lead to nickel dermatitis (11, 12, 20). Thus, this study does not indicate new sources of nickel allergy, but confirms already known causes. Dermatologists should continue to recommend their patients to use the dimethylglyoxime test on these well-known nickel-releasing items. In support, it has been demonstrated that repeated non-occlusive exposure to low nickel concentration may maintain and even worsen hand eczema in nickel-sensitized individuals (38).
ACKNOWLEDGEMENT
Funding for this research was provided by The Copenhagen County Research Foundation.
The authors declare no conflict of interest.
References