Sayaka Shibata1, Makoto Sugaya1, Yousaku Minatani1, Hideki Fujita1, Yuichiro Tsunemi1, Tomomitsu Miyagaki1, Hidehisa Saeki1, Kanako Kikuchi1, Takashi Asai2, Mineo Kurokawa2 and Kunihiko Tamaki1
Departments of 1Dermatology and 2Hematology & Oncology, Faculty of Medicine, University of Tokyo, 7-3-1 Hongo, Bunkyo-ku, Tokyo, 113-8655, Japan. E-mail; sayakashibata-tky@umin.ac.jp
Accepted February 9, 2009.
Sir,
Folliculotropic mycosis fungoides (MF) is a rare variant of MF characterized by the presence of folliculotropic infiltrates and preferential involvement of the head and neck area. The prognosis of patients with folliculotropic MF is worse than that of patients with classical MF (1). Some patients with folliculotropic MF take an aggressive course with visceral involvement.
CASE REPORT
A 62-year-old Japanese man visited our hospital with a 5-year history of itchy nodules on his scalp, which had gradually increased in number. He presented with multiple skin-coloured or dark-red tumoural nodules on his scalp and infiltrated dark erythematous plaques on his face (Fig. 1a, b). The largest nodule was 3 cm in diameter. He had lymphadenopathy on his left neck, but no systemic symptoms, such as fever, weight loss, or night sweats.
Fig. 1. (a) Clinical picture at first presentation. (b) Closer view of the nodule on the scalp. (c) Dense infiltrates of lymphocytes into the dermis (H&E ×40). (d) Folliculotropism of atypical cells (H&E ×200).
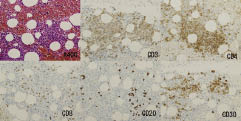
He had a slightly elevated serum soluble interleukin-2 receptor (sIL2-R) of 634 U/ml (normal: < 530 U/ml). He was a carrier of hepatitis B virus (HBV). Other investigations, including liver function tests, were all normal. Histopathological examination of the skin biopsy from the scalp showed dense infiltrates of small-to-medium-sized cells into the dermis. Large hyperchromatic cells with cerebriform nuclei were occasionally seen. These cells showed folliculotropism, but no epidermotropism (Fig. 1c). Alcian blue stain showed no mucin deposits. Immunohistochemistry revealed that infiltrating cells have a CD3+, CD4+, CD20– phenotype. Some of the large atypical cells were CD30+. Southern blot analysis detected a monoclonal rearrangement of T-cell receptor beta chain gene. There was no visceral or bone marrow involvement detected by 18F-fluorodeoxyglucose (FDG)-positron-emission tomography (PET) at that time (Fig. 2a). He was diagnosed with folliculotropic MF.
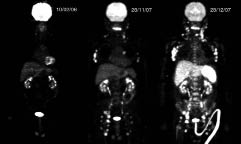
Fig. 2. Positron-emission tomography findings. Only skin nodules were detected in the neck, face and scalp area (10 February 2006) (left). Enlarged lymph nodes of his neck, axilla and inguinal area (28 November 2007) (middle). Diffuse high 18F-fluorodeoxyglucose (FDG) accumulation in the liver, spleen, bone marrow, and lymph nodes (28 December 2007) (right).
The patient was treated with psoralen plus ultraviolet A (PUVA) combined with oral etretinate (40 mg/day) and prednisolone (20 mg/day). The treatment was effective for some itchy erythematous plaques. The number of tumoural nodules was not increased till one year later, when they gradually developed on his back. Although local electron beam treatment improved the skin lesion transiently, his disease gradually progressed. Multiple tumoural nodules appeared on his head, trunk and extremities, and enlarged lymph nodes of his neck, axilla and inguinal area were also noted 1.5 years after the initial presentation. He was subsequently commenced on oral cyclophosphamide (100 mg/day) and steroid (20 mg/day). Two weeks later, he suddenly developed high fever and malaise. Blood test showed extremely elevated serum liver markers; amino aspartate transaminase (AST), 1998 IU/l (normal 9–38); alanine aminotransferase (ALT), 1675 IU/l (normal 4–36); total bilirubin, 3.9 mg/dl; and sIL-2R 7440 U/ml. He was diagnosed with serious acute hepatitis. Computed tomography (CT) showed diffuse and irregular enhancement of the liver without nodules. Considering the regression in the skin lesions after the change of medication, the hepatitis was, at first, considered to be caused by reactivation of HBV or drug hypersensitivity. FDG-PET showed an extraordinarily diffuse high FDG accumulation to the liver, spleen and bone marrow (Fig. 2). The standardized uptake value maximum of the liver was extremely high, suggesting malignancy rather than inflammation. In addition, the amount of HBV-DNA in the blood measured by PCR was not increased. Biopsy specimens from a swollen inguinal lymph node and from bone marrow, where high FDG accumulation was detected, showed diffuse infiltration of atypical lymphocytes, suggesting spread of the lymphoma (Fig. 3). White blood cell count was increased with a few percentages of atypical cells in the peripheral blood. Considering the above findings, we concluded that severe hepatic failure was due to direct hepatic involvement of lymphoma cells. In spite of the treatment with etoposide, he died within 8 weeks of the visceral involvement, especially severe hepatic failure.
Fig. 3. Immunohistochemical analysis showing bone marrow involvement of lymphoma cells. Infiltrating cells have a CD3+, CD4+, CD20– phenotype.
DISCUSSION
Extracutaneous involvement of cutaneous T-cell lymphoma (CTCL) is generally correlated to the extent of the skin lesions (2). Rappaport & Thomas (3) studied the autopsied patients with MF. Extracutaneous involvement was revealed in 71%, with highest frequency in the lymph nodes. The most commonly involved organs were lung, spleen, liver, kidney, thyroid glands and pancreas. Liver involvement was observed in 38%. Gross involvement was observed in 65%, while no gross abnormality was observed in 35%. It should be remembered that liver involvement of lymphoma cells could happen without nodules detectable with CT. Huberman et al. (4) investigated the patients with CTCL by multiple liver biopsies prior to therapy. Histological liver involvement was observed in 16% of the patients. None of the patients clinically showed liver dysfunction. Our case showed extremely elevated serum liver markers, which is quite rare in cases with liver involvement of CTCL.
FDG-PET has been reported to be useful in patient with CTCL (5, 6). These papers reported that FDG-PET can overcome many of the limitations of CT and gallium scintigraphy, especially in detecting residual or recurrent disease. As the detection of disease with FDG-PET is based on metabolism rather than on physical size, FDG-PET might be able to detect diffuse involvement without gross abnormality.
REFERENCES