Vladana Woznicová1, Petra Matějková2, Magdalena Flasarová1,2, Hana Zákoucká3, Eliška Dastychová4, Zuzana Vališová1 and David Šmajs2
1Department of Medical Microbiology, Faculty of Medicine, Masaryk University, Pekařská 53, CZ-65691 Brno, 2Department of Biology, Faculty of Medicine, Masaryk University, Brno, 3National Reference Laboratory for Diagnostics of Syphilis, Dermatovenerological Clinic, General Faculty Hospital, Prague, and 4Department of Dermatology, St Anne’s Hospital, Masaryk University, Brno, Czech Republic. E-mail: vladana.woznicova@fnusa.cz
Accepted September 7, 2009.
Sir,
The incidence of syphilis in developed countries has increased due to local outbreaks and is clearly associated with urban agglomerates and sexual tourism destinations (1). The recommended treatment for syphilis infection is penicillin G benzathine (2); however, suspected penicillin allergy is common among patients. Therefore, alternative therapeutic regimens are often used to avoid allergic reaction, even when the reliability of the information given by the patient is uncertain (3).
Macrolides have been used in patients with penicillin allergies for decades, especially in pregnant women (4). Multiple doses of erythromycin decrease treponema counts by greater than 300-fold, which is similar to the efficacy of penicillin (5). Clarithromycin was found to be effective in treating syphilis in the hamster model, and several human studies report that azithromycin can effectively replace penicillin therapy (6, 7). Nevertheless, treatment failure after administration of azithromycin in syphilis has been reported, and the genetic background of macrolide resistance was identified in clinical isolates as A2058G and A2059G mutations in the 23S ribosomal RNA gene of Treponema pallidum (8–11). In the Czech Republic, the prevalence of both mutations among clinical specimens is approximately 20% (11). Testing of macrolide-resistance in syphilis is limited by the fact that T. pallidum cannot be cultured under in vitro conditions, and thus routine testing is restricted to PCR amplification (11).
CASE REPORT
A 22-year-old woman presented for physical examination 2 months after unprotected vaginal sexual intercourse. Her partner had been involved in pornography and had been diagnosed recently with syphilis. The patient was afebrile, and physical examination revealed two small erosions, a 5-mm perianal erosion and a 2-mm cervical erosion, plus numerous tiny condylomata accuminata in the anal and vaginal areas. The patient reported a severe allergic reaction (extensive macular rash) after penicillin therapy 9 years previously.
Serological findings were as follows: rapid plasma reagin (RPR) 1:2, T. pallidum haemagglutination (TPHA) positive, FTA-ABS positive, enzyme-linked immunoassay (ELISA) immunoglobulin G (IgG) negative, ELISA IgM negative, Western blot IgG borderline, and Western blot IgM positive (antibodies against TpN17 and TpN47). The perianal lesion was negative using dark-field examination. However, PCR testing of the perianal lesion and the whole blood sample was positive and confirmed syphilis. The cervical erosion was not examined.
Using a nested PCR protocol, two different T. pallidum chromosomal loci were detected in the clinical samples: the polA gene (TP0105; 12) and the tmpC gene (TP0319; 13). Nested PCR detection of tmpC was performed as described previously (14). The PCR protocol for polA was modified for nested PCR, and detection was performed using the same conditions for both reactions (11).
PCR amplification and sequencing of TP0136 and TP0548 was also performed. Both genes code for hypothetical proteins and are highly divergent in the T. pallidum Nichols and SS14 strain genomes (15). Partial gene sequences were determined and compared with the sequences of T. pallidum type strains. The infecting isolate was identical to the type strain SS14.
The patient was given clarithromycin therapy (500 mg i.v. twice daily for 15 days) due to her history of penicillin allergy. The treatment was followed by oral administration of clarithromycin (500 mg p.o. twice daily for 7 days). The patient was instructed to return 6 weeks later for a follow-up examination.
However, the patient returned as late as 3 months later. Her serological findings were highly positive, including RPR 1:64 and Western blot IgM positive. The physical examination revealed slightly enlarged submandibular lymph nodes and left inguinal lymph nodes. Treatment failure was suspected; due to the patient’s personal history, re-infection was also considered a possibility.
The patient was given cefuroxime (750 mg i.m. every 8 h for 2 weeks, then 250 mg orally twice daily for 7 days) and her RPR titre decreased to 1:8 after finishing the medication. Six months later the RPR titre was negative.
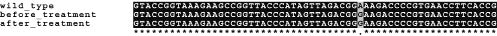
To confirm the reason for disease progression, as suggested by the serology, the patient’s follow-up whole blood sample was re-tested as at initial diagnosis and was positive. In addition, PCR amplification and sequencing of 23S rRNA genes in the initial and follow-up isolates were also performed. The follow-up isolate was identical to the T. pallidum isolate initially found in the patient’s skin lesion and whole blood and carried an A2058G mutation in the 23S rRNA gene (Fig. 1). This confirmed treatment failure and excluded patient reinfection.
Fig. 1. Partial sequence alignment of 23S rRNA gene of clinical isolates from the case report patient before and after macrolide treatment. *Identical nucleotides in all sequences; ·position corresponding to position 2058 in the E. coli 23S rRNA gene.
DISCUSSION
These findings highlight the importance of routine PCR diagnostics for patients with syphilis. In particular, it should be used for syphilitic individuals with non-penicillin treatment regimens, since T. pallidum is a non-cultivable organism and antibiotic resistance cannot be assessed using in vitro bacteriological methods. Treponemal DNA in syphilis can be detected from numerous types of clinical samples, but it is usually found in mucocutaneous swabs and whole blood (14).
Parenteral penicillin G is the only therapy with documented efficacy for treating syphilis in all clinical stages and forms, including pregnancy and neurosyphilis. If treatment with a macrolide regimen is needed, follow-up is essential. However, it should be emphasized that penicillin is preferred over macrolide antibiotics for treating syphilis.
ACKNOWLEDGEMENTS
This work was supported by a grant from the Ministry of Health of the Czech Republic (NR8967-4/2006), by a grant from the Grant Agency of the Czech Republic (310/07/0321), and by institutional support from the Ministry of Education of the Czech Republic (VZ MSM0021622415).
REFERENCES