Recurrent Boils of the Axilla and Groin: A Quiz
Kristina Ibler1, Lars Erik Bryld1, Preben Løvgreen Nielsen2 and Gregor B. E. Jemec1
Departments of 1Dermatology and 2Pathology, Roskilde Hospital, Health Sciences Faculty, University of Copenhagen, Køgevej 7–13, DK-4000 Roskilde, Denmark. E-mail: ksi@regionsjaelland.dk
A 32-year-old man presented with a 5 × 2 cm large painful abscess in the axilla. The lesion had developed over a year and started with follicular inflammation. Similar painful lesions developed in both genito-femoral folds and gradually progressed in extension. Lesions in the intergluteal fold were diagnosed by a general surgeon as fissures. There was no family history of hidradenitis suppurativa, and the patient had tried treatment with topical clindamycin solution 0.1% and systemic tetracycline with no effect.
Clinically the patient presented with nodular, suppurating lesions in the axilla surrounded by erythema and papulopustular lesions (Fig. 1). Similar lesions were found in the groin. The intergluteal lesions had resolved without scarring at the time of presentation, and there were no palpable lymph nodes.
Fig. 1. Nodular, suppurating lesions in the axilla surrounded by erythema and papulopustular lesions.
Following clinical examination a diagnostic procedure was performed.
What is your diagnosis? See next page for answer.
doi: 10.2340/00015555-1241
Recurrent Boils of the Axilla and Groin: Comment
Acta Derm Venereol 2011; 91: XX–XX.
Diagnosis: Langerhans’ cell histiocytosis
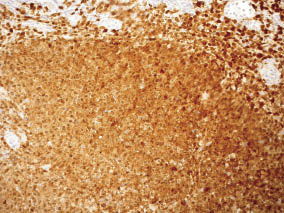
The clinical presentation and absence of palpable lymph nodes was not dissimilar from hidradenitis suppurativa (1, 2), but lack of scarring and sinus tracts and spontaneous resolution of some lesions prompted a biopsy. Histological examination revealed infiltration of S-100-positive histiocytes and remarkable eosinophilia in the dermis (Fig. 2), which was in agreement with a diagnosis of Langerhans’ cell histiocytosis. Further investigations included computed tomography (CT) scan of the thorax, biopsy of the bone marrow and ortopan X-ray (due to gingivitis) and all results were normal.
Fig. 2. Histology: eosinophilia in the dermis, S-100-positive histiocytes.
Langerhans’ cell histiocytosis is a rare disease. It belongs to a group of disorders characterized by clonal proliferation of the histiocytes, which can migrate to lymph nodes, skin, bones and internal organs and cause disease. The disease is rare and approximately one-third of those with Langerhans’ cell histiocytosis are adults. The prevalence in adults is approximately 1–2 per million, but the true incidence is unknown, since the disease is often under-diagnosed (3). The disease encompasses a broad clinical spectrum, ranging from an acute, fulminant and disseminated form (Letterer-Siwe disease), to the appearance of solitary or few indolent and chronic lesions in bones or other organs (eosinophilic granulomas). An intermediate form (Hand-Schuller-Christian disease) involves chronic multifocal lesions and classically presents with the triad of diabetes insipidus, exophthalmus and lytic bone lesions. A self-healing congenital form (Hashimoto-Pritzker disease) has also been described. Immune dysregulation, inflammation and malignancy have been proposed as causative for Langerhans’ cell histiocytosis (4).
The histology of Langerhans’ cell histiocytosis in the skin differs. In Letterer-Siwe disease the Langerhans’ cells are uniform, the cytoplasm abundant and eosinophilic and xanthomatized cells can be found. In the Hand-Schüller-Christian disease the infiltrate is often polymorphous with aggregated eosinophils, and xanthomatized cells are rare. Immunohistochemistry shows expression of S-100 and possibly also vimentin, HLA-DR and Ki-67. Often CD68 is weakly positive (5).
Treatment depends on the extent and severity of the disease. Localized skin disease is best treated with moderate-to-super-potent topical steroids or topical nitrogen mustard solutions if the cutaneous involvement is severe. Acitretin and psoralen plus ultraviolet A (PUVA) may also be effective (6–8). Chemotherapy, such as prednisone with or without vinblastine, can be used for widespread cutaneous disease. For isolated skin nodules or single node infiltration, excision is the treatment of choice. Multisystem disease or single-system disease unresponsive to other
therapies require chemotherapy. A combination of cytotoxic drugs and systemic steroids is generally effective (9).
The clinical course of Langerhans’ cell histiocytosis is variable. For isolated skin lesions or single node infiltration, the prognosis is excellent, but for elderly patients or those with organ dysfunction the course is less favourable, and even limited involvement may be serious depending on particular site involved and responsiveness to therapy. Haematological involvement or involvement of lungs, liver and spleen is associated with a poor long-term prognosis (10), and the mortality rate of multifocal disease is 10% (11). Most adults survive the disease, but in some cases the disease may run a progressive course and become life-threatening. A team approach of different specialities may be appropriate, since many organs may be affected. The congenital form of histiocytosis usually resolves spontaneously (12).
REFERENCES