Christian Apfelbacher1,2, Sonja Molin3, Elke Weisshaar2, Andrea Bauer4,5, Peter Elsner6, Vera Mahler7, Melanie Weiß2, Thomas Ruzicka3 and Thomas L. Diepgen2
1Medical Sociology, Department of Epidemiology and Preventive Medicine, University Hospital Regensburg, 2Department of Clinical Social Medicine, University Hospital, Heidelberg, 3Department of Dermatology and Allergology, Ludwig-Maximilians-University, Munich, 4Department of Dermatology, 5University Allergy Center, University Hospital Carl Gustav Carus, Technical University, Dresden, and Departments of Dermatology, 6University Hospital, Jena, and 7University of Erlangen, Erlangen, Germany
The aim of the CARPE registry is to investigate characteristics and medical care in patients affected by chronic hand eczema. Patients are assessed by dermatological examination and patient questionnaire. Socio-economic and clinical data are collected, and quality of life is measured using the Dermatology Life Quality Index (DLQI). A total of 1,163 patients with chronic hand eczema were eligible for analysis (mean age 47.0 years; 54.6% female; mean disease duration 7.6 years). At inclusion, chronic hand eczema was very severe in 23.4%, severe in 47.0%, moderate in 20.1%, and clear or almost clear in 9.6% of patients. Median DLQI was 8.0. In all, 93.8% of patients reported use of topical corticosteroids, 25.6% systemic antihistamines, 28.3% topical calcineurin-inhibitors, 38.0% ultraviolet phototherapy, and 35.3% systemic treatment (19.7% alitretinoin) prior to inclusion in the registry. A significant proportion of patients may not receive adequate treatment according to the guideline on management of hand eczema. Key words: registry; chronic hand eczema; health services research; systemic therapy; health-related quality of life.
Accepted Mar 8, 2013; Epub ahead of print Aug 27, 2013
Acta Derm Venereol 2013; 93: XX–XX.
Christian Apfelbacher, Medical Sociology, Institute of Epidemiology and Preventive Medicine, Franz-Josef-Strauß-Allee 11, DE-93053 Regensburg, Germany. E-mail: christian.apfelbacher@klinik.uni-regensburg.de
Hand eczema (HE) represents one of the most frequent diseases of the skin (1–3). According to a review of population-based studies, the point prevalence of HE is estimated at approximately 4%, and the 1-year prevalence at approximately 10% (4). The review identified female gender, the presence of a contact allergy, atopy, and exposure to wet work as important risk factors for HE.
As a disease entity, HE is not homogenous, but varies in terms of aetiology and morphology, necessitating complex differential diagnostics. Based on aetiology, the German guideline on management of HE (International Classification of Diseases (ICD-10) numbers: L20, L23, L24, L25, L30) differentiates irritant HE, allergic HE, atopic HE, protein contact dermatitis, and other forms of HE (genuine pompholyx type, tylotic, others) (5). Based on morphology, dyshidrotic (vesicular) HE, HE with erythema and scaling, hyperkeratotic-rhagadiform (tylotic) and nummular HE are differentiated. The severity of HE ranges from mild forms to severe chronic forms that require sick leave and can be partly refractory to therapy. The proportion of severe chronic HE (CHE) is estimated at approximately 5–7% and the proportion of patients refractory to topical therapy is estimated at approximately 2–4% (6). Health-related quality of life (HRQoL) is negatively affected in individuals with HE (7) and has a high socio-economic significance. Occupational skin diseases, most frequently manifesting on the hands, rank first among all occupational diseases in many countries (8).
Despite a multitude of therapeutic options, therapy for CHE remains a challenge (6). There is a notable lack of long-term data on the effectiveness and safety of the various treatment options for CHE. Therapy registries allow the collection of such data under routine conditions, thereby providing important insights that are not available from randomized controlled trials.
In the light of this paucity of long-term data on CHE the CARPE registry (German acronym CARPE: Chronisches Handekzem-Register zum Patienten-Langzeitmanagement, equivalent to: Chronic Hand Eczema Registry on Long-Term Patient Management) has been established in Germany since 2009 under the auspices of the German Dermatological Society (9).
We previously reported baseline data on the first 515 patients who were included in the registry (9). The aim of this paper is to present updated data from the registry, including socio-demographic and clinical characteristics, as well as data on the provision of medical care. In addition, data on HRQoL are reported for the first time.
MATERIALS AND METHODS
The CARPE registry was initiated as a prospective registry study and does not include any interventional component, invasive measures, or direct comparisons of therapies. Detailed information on the project is available at http://carpe.dermis.net. Any practicing dermatologist in Germany (either in private practice or in hospital) is eligible to participate. The methodology of the registry has been reported previously (9). Patients with CHE treated by a dermatologist in Germany are eligible for inclusion in the registry if the following criteria are met: (i) disease duration >3 months or >2 flares within the previous 12 months; (ii) previous treatment with topical corticosteroids; (iii) no long-lasting healing under adequate topical treatment including corticosteroids; and (iv) no other dominating active severe skin diseases or acute skin infections.
The documentation in the CARPE registry is based on a physician questionnaire (which can be completed on paper or online) and a patient questionnaire. After inclusion (T0) patients are followed-up in pre-specified time intervals after 3 (T1), 6 (T2), 12 (T3), 18 (T4), and 24 (T5) months. Fig. 1 illustrates the design of the CARPE registry.
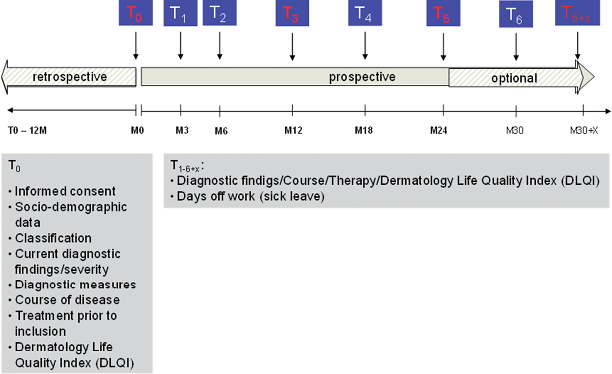
Fig. 1. Study design of the CARPE registry.
Data reported in this paper relate to the baseline assessment (T0). The severity of CHE is assessed using a Physician Global Assessment (PGA), supported by a validated photographic guide (10). Atopy criteria are recorded using the Erlangen atopy score (11, 12). The atopy score is a summary score of clinical and cutaneous signs and symptoms of atopy, which is designed to measure an atopic skin diathesis. Six diagnostic categories are provided to classify hand eczema, representing both aetiological (irritant contact dermatitis, allergic contact dermatitis, atopic hand eczema) and morphological categories (vesicular dermatitis, hyperkeratotic dermatitis, fingertip dermatitis). Data are presented in a table, as multiple answers were possible.
HRQoL is measured by the German version of the Dermatology Life Quality Index (DLQI) (13). The DLQI consists of 10 items and has a recall period of 1 week. Each item is answered on a 4-point scale and has a “not applicable” option. Total DLQI score is obtained by summing individual item scores. The maximum score is 30 and the minimum score is 0. Higher scores indicate greater impairment in quality of life. The following banding is used to derive clinically meaningful DLQI categories according to Hongbo et al. (14): DLQI scores 0–1 = no effect on patient’s life; 2–5 = small effect on patient’s life; 6–10 = moderate effect on patient’s life; 11–20 = very large effect on patient’s life; and 21–30 = extremely large effect on patient’s life.
Data management and statistical analysis
Data were entered and stored in a Microsoft Access 2003 database. Data were entered twice and plausibility checks were performed as measures of quality assurance. Analyses of quantitative and qualitative variables were carried out using SAS (version 9.2) and SPSS (version 20) for Windows. Quantitative variables were summarized by mean, median and standard deviation (SD). Qualitative variables are summarized by counts and percentages. All summary statistics refer to a total number of patients of n = 1,163, unless otherwise indicated.
RESULTS
Socio-demographic and clinical findings
The 1,163 CHE patients were recruited by a total of 95 centres, including 69 practices and 26 hospitals. Of these, 54.6% were female. Mean (age was 47.0 ± 13.7 years, age range 17.1–84.3 years, median: 48.9 years). Mean duration of hand eczema was 7.6 years (SD 9.1, median 3.8 years, n = 1,154). Mean body mass index (BMI) was 26.7 (SD 4.6, median 26.0) kg/m2 (n = 1,157). Of the included patients, 32.2% (n = 1,157) had received in-patient treatment (hospital treatment or rehabilitation measure) prior to inclusion in the registry, and 81.6% were currently gainfully employed (of these, 24.3% (N = 944) were currently unable to work, and 36.1% had been on sick leave due to HE in the past 12 months (N = 944)). Overall, 5.1% had lost or changed their occupation due to HE. Table I lists the occupations of the included patients. Nursing and healthcare, metal and electrical industry and food industry and catering were the most frequent occupations.
The most frequently reported localization was on the palm of the hand, while the least frequently reported localization was the wrist. In terms of other body localizations, the forearm was affected in 12.7% of patients, and the feet were affected in 72.9%. Irritant contact dermatitis was the most frequently occurring diagnosis (45.1%), followed by hyperkeratotic-rhagadiform (34.0%) and atopic hand eczema (34.0%). Of the 1,163 patients, 572 had a monodiagnosis (49.2%). Hyperkeratotic-rhagadiform hand eczema was the most frequent monodiagnosis (n = 198).
Table I. Most frequent occupations among the 944 subjects
|
Current occupation |
% |
|
Nursing and healthcare |
20.9 |
|
Metal and electrical industry |
18.1 |
|
Food industry and catering |
13.8 |
|
Office work, administration |
10.2 |
|
Cleaning |
5.6 |
|
Hairdressers and beauticians |
5.4 |
|
Construction |
5.3 |
|
Printing, chemical, textile and plastic industry |
4.3 |
|
Distribution, warehouse |
2.3 |
|
Motor vehicle operator |
1.6 |
|
Agriculture, animal farming |
1.6 |
An atopic skin diathesis was present in 41.2% of patients and was unclear in 9.7%. In 53.3% of patients, patch testing had been performed in the 12 months before inclusion in the registry. In 47.8% a type IV sensitization had been diagnosed previously. In 40.4% of the patients prick testing had been performed in the 12 months prior to inclusion. In 40.1% of the patients mycological diagnostics had been performed, of which findings were positive in 8.0% (Table II).
Table II. Localization and diagnoses of chronic hand eczema
|
Patients, % |
|
|
Localization (n = 1,160) |
|
|
Palm |
84.7 |
|
Back of hands |
47.8 |
|
Between fingers |
64.0 |
|
Wrist |
21.6 |
|
Forearm |
12.7 |
|
Diagnosis (n = 1,163) |
|
|
Irritant contact dermatitis |
45.1 |
|
Atopic hand eczema |
34.0 |
|
Hyperkeratotic hand eczema |
34.0 |
|
Vesicular hand eczema |
27.7 |
|
Allergic contact dermatitis |
22.3 |
|
Fingertip dermatitis |
7.7 |
Chronic hand eczema severity, itch and HRQoL
According to PGA, CHE was rated as very severe in 23.4%, severe in 47.0%, moderate in 20.1%, almost clear in 8.1%, and clear in 1.5% (n = 1,160). Overall, 81.3% of the patients reported pruritus, with mild pruritus being the most common (34.2%). 23.7% reported severe, 23.7% moderate, and 18.3% no itching. Of the patients with severe pruritus, 42.3% had atopic hand dermatitis and 37.9% irritant hand dermatitis. Median DLQI for the whole group of CHE patients was 8.0 (mean: 8.80, SD 6.3, n = 992). The spread of DLQI is illustrated in Fig. 2.
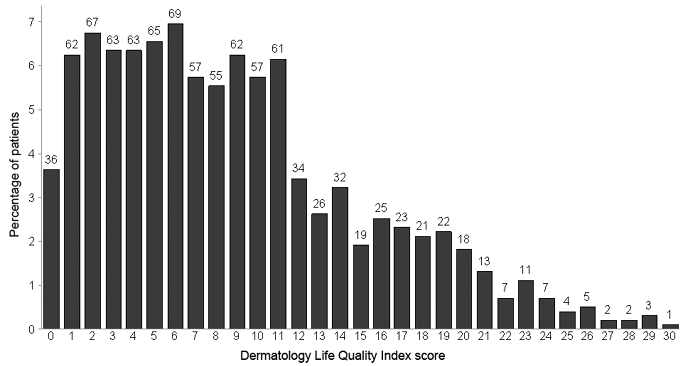
Fig. 2. Distribution of the Dermatology Life Quality Index. Number of patients are given.
Reported medical therapy in the 12 months before inclusion in the registry
Overall, use of topical corticosteroids was reported in 93.8% of patients in the 12 months prior to inclusion in the registry. Use of systemic antihistamines was reported in 25.6%, use of topical calcineurin-inhibitors in 28.3%, use of UV phototherapy in 38.0% and use of systemic treatment (except antihistamines) in 35.3%.
Further details of reported therapy with topical corticosteroids, topical therapy other than topical corticosteroids, ultraviolet (UV) therapy and systemic therapy are shown in Table III.
Table III. Reported treatments in the past 12 months (n = 1,163)
|
Topical |
Patients, % |
Ultraviolet therapy |
Patients, % |
Systemic treatment |
Patients, % |
|
Corticosteroids |
Bath Psoralen plus ultraviolet A |
5.5 |
Acitretin |
2.7 |
|
|
Highly potent |
26.8 |
Cream Psoralen plus ultraviolet A |
32.0 |
Alitretinoin |
19.7 |
|
Potent |
62.8 |
Other ultraviolet therapies |
4.7 |
Antihistamines |
25.6 |
|
Average |
52.7 |
Systemic Psoralen plus ultraviolet A |
0.3 |
Cyclosporine |
1.9 |
|
Mild |
16.2 |
Methotrexate |
0.4 |
||
|
Calcineurin inhibitors |
28.3 |
Corticosteroids |
14.4 |
||
|
Iontophoresis therapy |
5.0 |
||||
|
Other topical therapiesa |
25.8 |
||||
|
Salicylic acid |
21.3 |
||||
|
Tannin |
33.6 |
||||
|
Tar/shale oil |
18.1 |
||||
|
Urea |
57.6 |
aOther topical therapies include for instance topical antibiotics, antimycotics or antiseptics.
Table III. Reported treatments in the past 12 months (n = 1,163)
|
Topical |
Patients, % |
Ultraviolet therapy |
Patients, % |
Systemic treatment |
Patients, % |
|
Corticosteroids |
Bath Psoralen plus ultraviolet A |
5.5 |
Acitretin |
2.7 |
|
|
Highly potent |
26.8 |
Cream Psoralen plus ultraviolet A |
32.0 |
Alitretinoin |
19.7 |
|
Potent |
62.8 |
Other ultraviolet therapies |
4.7 |
Antihistamines |
25.6 |
|
Average |
52.7 |
Systemic Psoralen plus ultraviolet A |
0.3 |
Cyclosporine |
1.9 |
|
Mild |
16.2 |
Methotrexate |
0.4 |
||
|
Calcineurin inhibitors |
28.3 |
Corticosteroids |
14.4 |
||
|
Iontophoresis therapy |
5.0 |
||||
|
Other topical therapiesa |
25.8 |
||||
|
Salicylic acid |
21.3 |
||||
|
Tannin |
33.6 |
||||
|
Tar/shale oil |
18.1 |
||||
|
Urea |
57.6 |
aOther topical therapies include for instance topical antibiotics, antimycotics or antiseptics.
DISCUSSION
In their commentary on the significance of patient registries for dermatological disorders, de Souza & Rangel Miller (15) distinguish several objectives of patient registries, namely to: (i) characterize and describe the experiences of affected individuals; (ii) identify patients and treating physicians; (iii) assist the development of clinical care guidelines and improvements in care quality and disease outcome; (iv) encourage research, including genotype-phenotype correlations, and publication; (v) collect and store DNA and other biological/tissue samples from affected and unaffected family members; and (vi) collect post-marketing surveillance data for approved drugs
The data presented in this paper relate to objective (i), as we aimed to comprehensively characterize and describe the experience of patients affected by CHE. Mean disease duration was almost 8 years and CHE was graded as very severe or severe in approximately 70% of affected patients. Furthermore, approximately one-third of all patients had already received in-patient treatment and 36% had been on sick leave in the 12 months prior to inclusion in the registry. These data confirm severity and chronicity of CHE in affected patients. In Germany the social security system covers treatment of severe occupational skin disease (OSD) by means of interdisciplinary in-patient rehabilitation measures with the goal of avoiding loss or change of job (16, 17). The comparatively high figure for in-patient treatment can thus be explained by the fact that specialized centres for occupational dermatology offering such rehabilitation measures contribute significantly to the CARPE registry.
Further evidence for the impairment entailed by CHE stems from the analysis of the DLQI data. A Swedish study in 100 patients with hand eczema found a median DLQI of 6.0 (18), hence less QoL impairment compared with our data. However, a European multicentre study in 416 patients with hand eczema from 10 European patch test clinics found exactly the same median DLQI as in our study, i.e. 8.0 (19).
Several studies have investigated HRQoL in occupational hand eczema/contact dermatitis, and generally found lower estimates compared with our study. A study from the UK examined 70 patients with occupational contact dermatitis and found a median DLQI score of 5 (20). A Danish study included 758 patients with occupational hand eczema and reported a median DLQI of 5.5 for all patients and 7.8 for severe cases (21). A median DLQI score of 4.5 was found in a study in patients with occupational contact dermatitis from Australia (22). The more pronounced impairment of HRQoL found in this study in comparison to estimates reported in the literature again confirms severity and chronicity of CHE, as defined by the inclusion criteria for the CARPE registry.
Overall, 41% of patients had an atopic background and a type IV sensitization was reported in 48% of patients. Atopic hand eczema and allergic contact dermatitis were, however, reported in 34% and 22%. These data underline the multifactorial aetiology of CHE (23), which often results from the interplay of endogenous factors (atopic skin diathesis, genetic factors, such as filaggrin loss-of-function mutations (24)) and exogenous factors (allergens, irritants).
Ninety-four percent of patients included had been treated with topical corticosteroids in the 12 months preceding inclusion in the registry. This figure confirms the inclusion criteria, which include “previous treatment with corticosteroids”, as outlined above. 38% had received UV phototherapy, which is recommended as treatment step 2 for moderate-to-severe hand eczema in the guidelines on the management of hand eczema (5). Systemic immunomodulating
therapy (e.g. alitretinoin, systemic corticosteroids, and cyclosporine) is recommended additionally in step 3 if HE is persistent or chronically relapsing. Thirty-five percent had received some form of systemic treatment (except oral antihistamines); hence systemic treatment might be underutilized in CHE. A myriad of reasons may account for this finding. Systemic treatment may predominantly have been used for those patients with the most severe CHE (23.4% had very severe CHE) or the most pronounced impairment in HRQoL (33.9% had a DLQI ≥11). Patients from occupational dermatology centres may have received comprehensive measures of secondary and tertiary prevention before or instead of systemic treatment. Many patients were included in the CARPE registry when treatment by alitretinoin had just become available in Germany in 2008 and practical experience was limited.
There is no evidence-base for the use of oral antihistamines in the management of CHE, which is in contrast to the 26% of patients who report having received oral antihistamines. Oral antihistamines are probably prescribed for the itch associated with CHE, but the pathogenesis of itch involves many other mediators, such as proteases.
Strengths and weaknesses
The strength of the CARPE registry study is the comprehensive assessment of the medical history, current skin lesions, and medical care by a physician questionnaire, in parallel with an assessment of quality of life and satisfaction with care by a patient questionnaire. This allows to capture both the dermatologists’ as well as the patients’ perspectives. The assessments are carried out at regular intervals, which allows to evaluate the natural history of disease over time, as well as an investigation of the comparative effectiveness of various therapeutic options. Prospective data will be reported in the future.
Looking at the participating centres it becomes evident that a number of centres that contribute a significant proportion of the patients included in the CARPE registry are centres with a special focus in occupational dermatology. Patients with occupational CHE and severe forms of CHE thus seem to be overrepresented in the CARPE registry. It is, however, difficult to judge the degree of selection bias that may have occurred, as there are no robust population-based data on the characteristics of CHE in the general population. It would have been of value to collect blood samples for genetic analyses and to screen for psychiatric co-morbidities. However, the value of potentially important information needs to be weighed against the fact that a multi-centre registry will be successful only if the burden for physicians and patients is acceptable.
Conclusion
It proved feasible to implement a prospective CHE registry study in Germany. Both subjective and objective parameters confirm the chronicity and severity of CHE. A multitude of therapeutic options are reported in CHE patients. A significant proportion of patients may not receive adequate treatment. Future research will need to make use of longitudinal data to study the course of the disease and the effectiveness of different therapies in a comparative manner.
ACKNOWLEDGEMENTS
The authors are indebted to all the dermatologists who, with great commitment, have contributed to the CARPE registry project see Appendix S1 (available from http://www.medicaljournals.se/acta/content/?doi=10.2340/00015555-1632).
Funding source: The CARPE registry is funded by the German Dermatological Society and supported by Basilea Pharmaceutica.
Conflicts of interest: CA, SM, EW, VM, PE, TR and TLD received honoraria and lecture fees from Basilea Pharmaceutica. AB received lecture fees from Basilea, Meda, Astellas, Novartis and GlaxoSmithKline. MW declares no conflicts of interest.
REFERENCES
