Andrea Bauer, Kathrin Hault, Andrea Püschel, Henriette Rönsch, Peter Knuschke and Stefan Beissert
Department of Dermatology, University Hospital Carl Gustav Carus, Technical University Dresden, Dresden, Germany
Adequate sun protection is often neglected during occupational outdoor work. To investigate the acceptance and usability of sunscreens during outdoor work a single-blind, randomized-controlled, cross-over trial was performed in 40 subjects. Two sunscreen formulations were used daily on working days for 4 weeks at a time, with a wash-out phase before crossover. The primary outcome was overall acceptance of the products with daily application. More than 80% of the outdoor workers were fully satisfied with the cosmetic properties, sweat resistance, performance and usability of both products under outdoor working conditions. With respect to overall performance, the milk was rated slightly better than the gel. In terms of ease of application, the milk was preferred (p<0.05). Sunscreens for those working outdoors must contain very high, broad-spectrum, photostable filters for both UVB and UVA, they must be easy to apply and sweat resistant, and should not irritate the eyes. Key words: sun protection; outdoor work; sunscreen; acceptance; usability.
Accepted Apr 16, 2013; Epub ahead of print Aug 27, 2013
Acta Derm Venereol 2013; 93: XX–XX.
Andrea Bauer, Department of Dermatology, University Hospital Carl Gustav Carus, Technical University Dresden, Fetscherstr. 74, DE-01307 Dresden, Germany. E-mail: andrea.bauer@uniklinikum-dresden.de
Previously published systemic literature reviews on the role of occupational solar ultraviolet (UV) exposure for the development of basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) in outdoor workers have shown occupational UV radiation to be a significant risk factor for both tumour types (1, 2). Meta-analyses show that UV-exposed outdoor workers are at a significantly increased risk of developing SCC (pooled odds ratio (OR) 1.77; 95% confidence interval (CI) 1.40–2.22) and BCC (pooled OR 1.43 (95% CI 1.23–1.66) (1, 2). However, the risk may be even higher. Pooling studies on SCC, which had adequately controlled for confounding by age, sex, skin type and leisure time exposure resulted in a much stronger association (pooled OR 4.58; 95% CI 0.89–23.59) (3–5). For BCC, studies controlling for confounders, such as sex and leisure time exposure, showed a significantly stronger association (pooled OR 3.19; 95% CI 2.33–4.36) of occupational UV exposure and BCC risk, suggesting underestimation of the true association of occupational UV exposure and BCC risk during outdoor work (1).
Thus, the necessity of adequate primary and secondary prevention of UV-induced skin damage and cancer in outdoor occupations is obvious. In the European Community there are legal regulations concerning artificial UV sources in the workplace (6), but there are no European legal regulations concerning UV-protection of solar-exposed workplaces. However, there are recommendations on prevention measures, including technical and organizational measures, as well as personal UV-protection, such as sun-protective work-clothes, hats and sunglasses, as well as the use of sunscreens on unprotected areas of exposed skin (7, 8). However, studies in outdoor workers have shown considerable compliance problems in the regular use of personal UV-protection measures (9–16).
For sunscreen use, the major factors influencing compliance are thought to lie in the cosmetic properties and usability of the products in outdoor work. Weber et al. (15) supplied 13 tinsmiths (work frequently on roofs and facades and often manipulate highly reflective metal surfaces) with different sunscreens and asked them to rate the products. Products likely to be accepted were those that were easy to apply even with dirty hands, that did not smell oily or result in a sticky feeling, that were resistant to mechanical irritation and sweat, and that did not irritate the eyes (15). However, field study data on the acceptance of sunscreens in outdoor work are scarce. The aim of the present study was to investigate the acceptance and usability of 2 different sunscreen formulations during daily use in outdoor work under real-life conditions, in order to make evidence-based recommendations for future prevention regimes.
Methods
This randomized controlled prospective cross-over study was performed at the Department of Dermatology, University Hospital, Carl Gustav Carus, Dresden, between 4 June and 19 October 2011. The protocol was approved by the Institutional Ethical Committee of the University Hospital Carl Gustav Carus, Dresden. All participants gave written informed consent before participation in the study.
Study design and patients
A single-blind, randomized-controlled, cross-over trial in outdoor workers to evaluate the acceptance and usability of 2 sunscreen formulations, a gel (LSF 50, UVA-PF 20) and a milk (LSF 50+, UVA-PF 33) (Anthelios, La Roche-Posay, Asnieres, France) in 40 outdoor-workers (male n = 26; 65%) was performed. Products were used daily on working days for a period of 4 weeks at a time, with a wash-out phase of 1–2 weeks before cross-over.
Inclusion criteria were a minimum age of 18 years, and occupations in which at least 80% of the working day was spent outdoors. Workers with skin conditions, actinic keratoses or skin cancers of the face, neck, arms and hands, as well as those with allergic reactions to the sunscreens under investigation or those who had participated in clinical studies within a 30-day period prior to this study were ineligible. Individuals with planned vacation time during the course of the trial were also not included.
Sunscreens
The sunscreens were provided by La Roche-Posay, Laboratoire Pharmaceutique (Asnieres, France). Anthelios milk (SPF 50+/PPD 33) and Anthelios gel (SPF 50/PPD 20) are (among other UV filters) formulated with Mexoryl XL (UVB/UVA) and Mexoryl SX (UVA) (17).
Outcome measures
Primary outcomes of interest were the overall acceptance of the products with daily application in an outdoor occupation, and the number of drop-outs due to adverse effects. Secondary outcome measures were differences in acceptance, differences in cosmetic properties, sweat resistance, performance and usability of the products, as well as differences in product-associated adverse effects with daily application.
Power calculation
Based on an assumed acceptance of the gel of 80% and the milk of 50% among the outdoor workers, a required sample population of 39 participants was calculated for 80% power (α = 0.05, two-tailed). To compensate for eventual drop-outs, a final sample size of 40 was chosen.
Randomization and visit plan
The 40 workers were randomly assigned a sequence of treatments using a web-based research randomizer (http://www.randomizer.org). Two sets of 20 unique numbers per set were created for the numbers 1–40, thus randomly allocating 20 patients to each of the 2 groups. Randomization was performed by the research assistants, by allocation of the consecutive patients to the lowest available number from the randomization list. Finally, half of the participants were first given the gel for 4 weeks, followed by the milk for a further 4 weeks with a 1–2-week wash-out period between treatments, while the other half of the workers applied the 2 products in reverse order (Fig. S1; available from: http://www.medicaljournals.se/acta/content/?doi=10.2340/00015555-1667). Assessors were blinded to group assignment during collection of the data.
The study started with a screening period. After baseline, a follow-up and a final visit were scheduled at the end of the first and second 4-week product application period, respectively. At baseline, participants were screened for inclusion and exclusion criteria, socio-demographic parameters (age, sex, weight, height, occupation, school qualification, skin type) and accompanying illnesses. After inclusion in the study, participants were instructed how much (2 mg/cm2) and how often (in the morning before work and ≥ 2 times a day) the sunscreens had to be applied on working days. The correct application on the sun-exposed areas of the skin (face, neck, décolleté, hands and arms) was demonstrated and was practiced by the participants at baseline. Each participant was supplied with 600 ml sunscreen per application period. Compliance was measured by weighting the tubes before and after the application periods. During the follow-up and the final visits participants completed standardized questionnaires concerning cosmetic properties, practicability, usability and adverse effects (Table SI; available from http://www.medicaljournals.se/acta/content/?doi=10.2340/00015555-1667).
In addition, personal diaries, concerning frequency of product use as well as adverse effects on the eyes and/or skin, were completed daily.
The body surface area of each participant was calculated using the Mosteller Formula, while the rule of nines was implemented to determine the approximate surface area of the head, neck, arms and hands (18). Using this information, the surface density of product applied was established for each worker.
Statistical analysis
Throughout the study, the workers’ information, including completed questionnaires, was collected in patient folders and made identifiable only by randomization numbers. Data were entered pseudonymously into a Microsoft Access databank. It was analysed using descriptive statistics with the IBM Statistical Package for the Social Sciences (SPSS) software program Version 19. As the possible answers to the questionnaire provided ordinal data, differences in the assessment of the sunscreen formulations were tested by using the Wilcoxon signed-rank test. Order effects were tested using the Mann-Whitney U test and the Fisher test.
Results
Socio-demographic characteristics and skin types
Based on the demographic data collected, the mean age of the 40 workers included in the study was 44.5 years (age range 22–57 years; 26 males, 14 females). Thirty-eight (95%) of the outdoor workers had graduated from the Mittelschul-track of the German school system, having earned a school-leaving diploma at the ninth- or tenth-grade level. Two (5%) of the participants had completed the twelfth grade and had received university degrees. The majority of participants were employed in landscape-gardening/agriculture (n = 18) or building/construction (n = 16). Also included were 4 people working in bicycle courier services, one riding instructor and one social worker, all of whom spent at least 80% of their working day outdoors.
The skin type of each participant was assessed during the baseline interview. Of the 40 outdoor workers, 6 had skin type I (according to Fitzpatrick’s skin types), 18 skin type II and 16 skin type III.
Cosmetic acceptance and usability
During the follow-up and final interviews, participating outdoor workers were asked to complete questionnaires (12 questions at follow-up, 13 questions at final visit) to evaluate the usability and cosmetic acceptance of the gel and the milk. The results are summarized in Table SII (available from http://www.medicaljournals.se/acta/content/?doi=10.2340/00015555-1667). Below some of the results are commented.
Ninety-five percent (n = 38) of participants considered the milk to be “very easy” or “easy” to apply and spread. In comparison, 77.5% (n = 31) thought the same of the gel (p = 0.02) (Fig. 1).
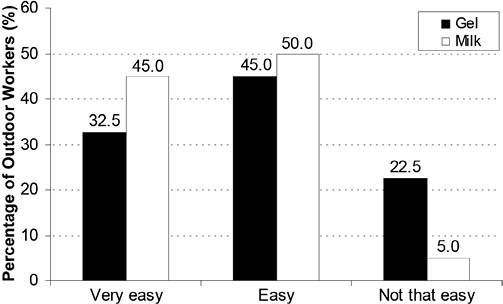
Fig. 1. Is the sunscreen easy to apply and spread on the skin?
When the participants were asked to assess how the 2 sunscreens felt on their skin, 87.5% (n = 35) found the gel, and 92.5% (n = 37) the milk, to be “pleasant” or “very pleasant” (p = 0.17).
Four (10%) of the participants using the gel and one (2.5%) using the milk (p = 0.08) reported the occurrence of minor skin irritations. Moderate eye irritations occurred in 7.5% (n = 3) of those using the gel and in 2.5% (n = 1) using the milk. Severe to extreme reactions of the eye were described by 2.5% (n = 1) of the participants with the gel and 7.5% (n = 3) with the milk (p = 0.84) (question 6).
The majority of the participants rated both the gel (85%) and the milk (90%) as being “good” or “very good” when it came to sweat resistance (p = 0.61) (question 7). Not surprisingly, the participants who rated sweat resistance as “not that good” or “poor” reported the occurrence of significantly more eye irritations (p < 0.05).
For the primary outcome measure, the overall acceptance of the sunscreens, the gel was rated “good” or “very good” in 75% (n = 30) of cases and the milk in 85% (n = 34) (Fig. 2). The mean marks for milk and gel were 1.98 and 2.25, respectively (p = 0.08).
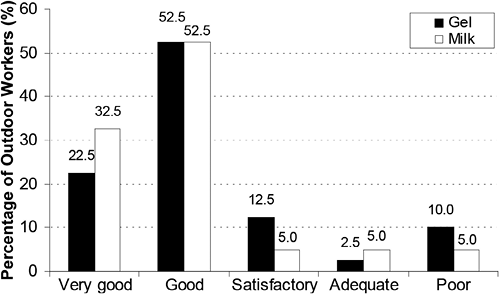
Fig. 2. What is your overall impression of the sunscreen?
All questions were tested for order effects, i.e. whether the results differed if subjects received the milk or the gel first. Concerning the gel, no order effects were observed. Concerning the milk, significant differences were observed for the questions: “Is the sunscreen easy to apply and spread on the skin?” and “Does the sunscreen cause eye irritations (burning, itchiness, erythema of the eyes)?” Those patients who had been given the milk first felt that it was more difficult to spread and rather rated it “good” rather than “very good” (compared with the other group, p = 0.038). They also reported more eye irritations (p = 0.008). No order effects were found for the amount of the sunscreens.
Sunscreen consumption and frequency of application
Over a period of 20 work-days participants applied a mean of 204 ± 131 g of the gel and 209 ± 133 g of the milk to sun-exposed skin of the face, neck, décolleté, arms and hands. On each working day 10 g of the gel and 10.5 g of the milk were used. Despite instructions provided at the baseline visit to use the sunscreens ≥ 3 times a day, products were used only 1.5 times. (Table SIII; available from http://www.medicaljournals.se/acta/content/?doi=10.2340/00015555-1667).
Discussion
The majority of UV-protection campaigns focus on leisure time exposure and on holidays. The recent discussion on under-reporting of occupationally related skin cancer in Denmark, as well as ongoing discussions in Germany about whether to include SCC of the skin due to solar UV-radiation exposure during outdoor work as a new occupational disease, makes the current report timely (19, 20).
If technical and/or organizational measures are not sufficient to shield workers from UV exposure, personal protective means, such as UV-protective clothing and hats, are recommended. The rest of the UV-exposed skin should be protected by sunscreens. The 2 products studied here are commercially available broad-spectrum, photostable sunscreens, a gel (SPF 50, UVA-PF 20) and a milk (SPF 50+, UVA-PF 33) formulation. It was recently shown that, broad-spectrum sunscreens with high UVB and UVA protection provide better protection from solar ultraviolet-simulated radiation, especially natural sunlight-induced immunosuppression, than UVB filters alone (21). Specifically, the broad-spectrum UVA absorber, Mexoryl SX was proven to prevent the cutaneous detrimental effects of UV exposure (22). Moreover, Mexoryl XL, Mexoryl SX and Tinosorb S are photostable and the specific galenism of the products allows a complete and homogenous spread of the sunscreens on the surface of the skin to provide optimal sun protection (23).
The present study is the first randomized controlled trial comparing the acceptance and usability of different sunscreen formulations under real conditions during outdoor work. This is important because, until now, workers’ compliance with the use of UV-protective measures in outdoor work has been low (9, 10, 12, 13, 15, 16, 24). Weber et al. (15) revealed that only 40% of Austrian tin-smiths used sunscreens regularly on a sunny working day (15). Geller et al. (24) reported that 50% of swimming pool staff had a history of severe sunburns, and approximately 80% remembered having acquired a sunburn during work time in the last summer season (24). Only a minority of Californian farm-workers (12), as well as postal service letter carriers used sunscreens regularly (13). In a cross-sectional study of 3 groups of workers, Stepanski & Mayer (9) found that only approximately 50% of workers protected themselves adequately. Most commonly, the face and lower arms were unprotected (9). Keeping in mind that regular sunscreen use can prevent photo-ageing of the skin, premalignant epithelial skin lesions, and skin cancer, improvement in compliance is crucial (25–31).
Our cohort includes a broad range of typical outdoor occupations. The majority were employed in landscape-gardening and agriculture occupations (n = 18), or in building and construction (n = 16). Our data suggest that outdoor workers prefer more liquid formulations, e.g. milks, because of their spreadability compared with gel formulations, which have a thicker consistency. Our findings are congruent with the results of a recent study on community members’ (Rochester, Minnesota) preferences for facial sunscreens, which revealed that subjects were significantly more likely to use products again if they were less greasy, less likely to leave a film, and less likely to trigger a hot and sweaty feeling (32). From an occupational point of view, Weber et al. (15) reported that, for Austrian tin-smiths, the most important quality was that the product was easy to apply. In this study sprays were preferred to other methods of application (15). In our study the gel and the milk came in conventional tube packaging. The majority of the outdoor workers rated the manageability of both the gel (90%) and the milk (97.5%) to be “good” or “very good. Bearing in mind that dosing of adequate amounts of sunscreen might be more difficult using a spray, conventional packaging might be preferred. Concerning sweat resistance, both products were rated by the participants as being “good” or “very good” (gel: 85%, milk: 90%). However, severe to very severe itching, burning and/or redness of the eyes after contact with the products were described by 2.5% (n = 1) of the participants with the gel and 7.5% (n = 3) with the milk. To prevent eye irritation, specific training for the correct use of the products around the eyes seems necessary. Alternatively, sunscreen sticks with a higher consistency might be a good alternative in this sensitive area. Skin irritations were rare, and those reported were generally mild (gel 10%, milk: 2.5%). From our results, we hypothesize that outdoor workers would prefer less rich, milky formulations that are highly sweat-resistant and pose a low risk for eye irritations.
Sun protection factor ratings of sun protection products are performed under laboratory conditions using 2 mg/cm2 of products. Our data confirm that, even under study conditions and individual training of the participants, the recommended amount of 2 mg/cm2 of sunscreen to be applied to the skin was not reached. Under study conditions approximately 1.3 mg/cm² were used. Other studies suggest that even lower amounts (range 0.2–0.8 mg/cm2) are applied by consumers (33). This leads to considerable lower protection levels than indicated on the products (34). To overcome this problem UV-protection training should be an integral part of regular work safety programmes. Moreover, to compensate for the well-documented issue of the application density of the products rarely reaching 2 mg/cm2, sunscreens for outdoor work should contain very high, broad-spectrum, photostable filters for UVA and UVB protection (SPF 50+, UVA-PF > 1/3 SPF).
AcknowledgementS
The study was supported by a grant from La Roche-Posay, Asnieres, France.
Conflicts of interest: SB, KH, AP, HR and PK declare no conflicts of interest, AB received lecture fees from La Roche-Posay and Spirig Pharma AG.
References
