Jose Hernan Alfonso1, Jacob P. Thyssen2, Tore Tynes3, Ingrid Sivesind Mehlum1 and Håkon A. Johannessen3
Departments of 1Occupational Medicine and Epidemiology and 3National Work Environment Surveillance, National Institute of Occupational Health, Oslo, Norway, and 2National Allergy Research Centre, Department of Dermato-Allergology, Gentofte Hospital, University of Copenhagen, Denmark
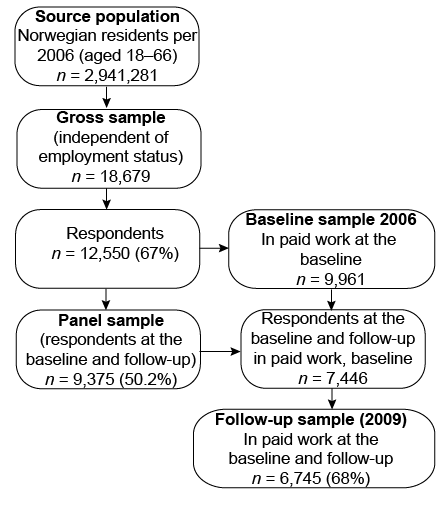
Prospective studies on occupational dermatoses in the general working population are sparse. This study investigated prospectively the impact of self-reported occupational exposure to chemicals and physical factors on the risk of skin problems. The cohort comprised respondents drawn randomly from the general population in Norway, who were registered employed in 2006 and 2009 (n = 6,745). Indoor dry air (odds ratio (OR) 1.3; 95% confidence interval (95% CI) 1.1–1.6) was a significant baseline predictor of skin problems at follow-up, whereas exposure to cleaning products (OR 1.7; 95% CI 1.2–2.5), water (OR 1.4; 95% CI 1.1–1.9) and indoor dry air (OR 1.6; 95% CI 1.1–2.1) at both measurement time-points was significantly associated with skin problems. The population risk attributable to these factors was 16%. This study quantified the contribution of occupational exposure factors to skin problems in the general working population of Norway. Key words: general working population; skin problems; occupational factors; population – attributable risk; epidemiology; prevention.
Accepted Apr 27, 2015; Epub ahead of print May 5, 2015
Acta Derm Venereol 2015; XX: XX–XX.
Jose Hernan Alfonso, Department of Occupational Medicine and Epidemiology, National Institute of Occupational Health, Pb 8149 Dep, NO-0033 Oslo, Norway. E-mail: jose.alfonso@stami.no
Skin problems caused or worsened by factors present in the work environment impose a significant burden on affected individuals and society (1). Occupational dermatoses, mostly contact dermatitis, represent an inflammatory response of the skin that typically occurs as a result of repeated exposure to irritants or allergens. The most frequent localizations of these conditions are the hands and forearms, and a major cause in the workplace is “wet work”, i.e. frequent or long-lasting contact with water, soaps, detergents and disinfectants, and prolonged wearing of occlusive gloves (2). Other occupational substances that cause dermatoses include oils, lubricants and solvents. In both female- and male-dominated occupations, the 1-year prevalence of hand eczema has been estimated at between 20% and 30% (3–6).
Although there is a well-established relationship between certain work-related skin exposures and specific dermatoses, prospective studies addressing the effects of multiple work factors in the general working population are scarce (7). Moreover, the studies that are available focus on specific occupations (3–6); and the contribution of physical factors, such as heat and cold and dry air, is often dismissed (8).
The aim of this study was to investigate the impact of self-reported work-related exposure to skin irritants and physical and chemical factors on the risk of skin problems in a 3-year prospective cohort randomly selected from the general working population of Norway.
MATERIALS AND METHODS (see Appendix S11)
RESULTS
The study cohort comprised respondents drawn randomly from the general working-age population in Norway, who were registered as being in an active employee relationship in 2006 and 2009 (n = 6,745) (Fig. 1).
Exposure to 9 chemical and physical hazards (Table I) at work was regressed on skin problems at follow-up (2009) using the following designs: (i) prospective analyses with exposure measured at baseline (2006) and; (ii) prospective analyses with exposure measured at both baseline and follow-up.
Table I. Exposure measurement at baseline (2006) and follow-up (2009)
|
Type of work environment exposure |
|
Skin contact |
|
Water |
|
Cleaning products, disinfectants, solvents or other degreasing agents |
|
Oils, lubricants or cutting fluids |
|
Physical factors |
|
Heat, i.e. temperatures of approx. 28°C or higher |
|
Cold, i.e. working outdoors in the winter, or working in cold rooms |
|
Poor indoor environment in terms of dry air |
|
Chemical factors |
|
Mineral dust, e.g. from stone, quartz, cement, asbestos or mineral wool |
|
Metal dust, e.g. from weld fumes, lead, chrome, nickel, zinc, aluminium, cobber or tin dust |
|
Organic dust, e.g. from textiles, wood, flour, clothes or animals |
Table II shows the 1-month prevalence of skin problems at different measurement times. The risk of having skin problems at follow-up (Table SI1) decreased with age, except for the oldest age group, and was higher among women compared with men (p < 0.01).
Table II. Cases of self-reported skin problems at baseline (2006) and at follow-up (2009)
|
Cases, n |
Cases, % (95% CI) |
|
|
At baseline |
1,311 |
13.2 (12.5–13.8) |
|
At follow-up |
786 |
11.7 (10.9–12.5) |
|
At both time-points |
401 |
5.9 (5.4–6.5) |
Estimation of the effect of baseline exposures on skin problems at follow-up using model #2 (adjusted for skin problems at baseline) (Table SII1) revealed that water, cleaning products and indoor dry air were significant predictors. However, in the model that included further adjustment (model #3: sex, age, and occupation), the effect of water and cleaning products was not statistically significant. Conversely, exposure to oil/cutting fluids showed a significant effect only in this model, but after adjusting for cleaning products (model #4) this association was no longer statistically significant. Work-related exposure to indoor dry air had a statistically significant effect on skin problems in all models evaluated here.
Statistically significant associations with skin problems were found for respondents exposed to water, cleaning products and indoor air at both baseline and follow-up (Table SIII1, all models). Exposure to heat and organic dust/fumes at follow-up only significantly predicted skin problems in the different models. Exposure only at follow-up and at both time-points to oil/cutting fluids had a significant effect on skin problems in model #3. However, this effect was not statistically significant after adjusting for cleaning products (model #4).
No statistically significant associations were found regarding exposure to cold, metal or mineral dust/fumes.
The total combined population-attributable risk (PAR) for significant work-related exposure factors was 15.8% (Table SIII1). Exposure to cleaning products showed the largest single PAR (7.3%), followed by water (4.4%).
In analyses that were stratified according to sex using model #4 (results not shown), the effect of occupational exposure to water at both time-points was observed in women only (OR 1.6; 95% CI 1.1–2.2 vs. men OR 1.0; 95% CI 0.5–1.9). The effect of work-related exposure to indoor dry air at both time-points was stronger among men (OR 2.0; 95% CI 1.1–3.4) compared with women (OR 1.4; 95% CI 0.9–2.0). No major sex differences were found regarding the effect of other work-related exposure factors.
DISCUSSION
This study, based on a randomly drawn cohort of the general population of Norway, has demonstrated the contribution of work-environment factors on the risk of subsequent skin problems. To our knowledge, we are the first to have shown this contribution in such a population (7, 9).
The most consistent predictors of skin problems were indoor dry air, water and cleaning products.
The consistent result regarding indoor dry air was unaffected after adjusting for other variables, which indicated that this is a robust finding and that perceived dry air acts as an independent risk factor. To the best of our knowledge, this finding has not been reported previously in a prospective study of the general working population. Therefore, dermatoses due to perceived dry air may be more distressing than their comparative paucity of physical signs might suggest (8, 10). The fact that indoor dry air was the most frequent work exposure reported is in accordance with the large number of Norwegian people working indoors. Although the perceived air “dryness” may be a proxy of actual humidity, in temperate areas such as Scandinavia, the low humidity/high temperature indoor environment is accompanied by low humidity/low temperature outdoor climate during the winter, which also has a drying effect on the stratum corneum (10). However, it is important to emphasize that the sensation of dryness should not always be interpreted as an indicator of low indoor air humidity (11), since different kind of particles and dusts may contribute to this sensation (8, 10). Nevertheless, in our study, the subjects who reported dust exposure exhibited little overlap with those who reported a sensation of indoor dry air. The sex difference observed, with stronger effect among men, may be due to a poor knowledge about skin care (12) and a lower use of moisturizers by men (13).
The finding that cleaning products and water were consistent predictors of skin problems is in agreement with results from a Norwegian register-based study, in which cleaning agents and water were among the most common exposure factors associated with notified work-related skin diseases during the period 2000–2013 (14). The effect of water was found only in women and is probably explained by jobs in which most of the tasks consist of wet work and cleaning (15).
According to our results, the injurious effects of oil and cutting fluids were partly mediated by skin exposure to cleaning products, because the risk of skin problems was lower after adjusting for exposure to cleaning agents. The effect of this occupational exposure has not been assessed previously at the population level and this constitutes a novel finding. Skin exposure to oils, fuels and solvents was the third most common exposure for the work-related skin diseases notified for the period 2000–2013 in Norway (14).
Work-related exposure to heat was a significant predictor of skin problems among workers who were exposed at follow-up only, and this is in accordance with the short-term effects of high temperatures (10). The clinical impression that cold exposure contributes to occupational dermatoses was partially verified in this study, and we speculate that sample characteristics (e.g. sample size) may have affected the significance of our results. As there is evidence of the detrimental effects of cold exposure on the skin (10, 16) further population studies are warranted.
Given that the risk of having skin conditions was increased among workers who were exposed at both time-points, our results demonstrate the harmful effect of long-lasting and cumulative exposure on the risk of having skin problems at the population level. Conversely, the low OR for exposures that occurred only at baseline may be interpreted as a result of people changing their work, or of the hardening or implementation of preventive measures in the workplace. Furthermore, the low OR obtained for subjects who were exposed only at baseline (Table SIII1) suggests that exposure reduction leads to a decreased risk of developing skin problems in the general working population.
Several studies have suggested that people change or lose their jobs because of skin problems (17, 18), and that these job changes occur early in the course of the disease (19, 20). Moreover, we do not know whether participants with chronic skin disorders were less likely to respond at baseline. In addition, it is possible that the most vulnerable people had already left their jobs (21) and were thus excluded from this cohort. Both of these selection processes are likely to lead to a healthy worker effect before recruitment and attenuated risk estimates.
This study aimed to estimate the contribution of occupational exposures on skin problems in a general population, and not a complete causal mechanism (22) where individual susceptibility (23, 24) and non-occupational exposures are also of relevance. Thus, it is reasonable that the population risk that was attributable to occupational factors was 16% in our population.
The validity of this longitudinal study was supported by a large representative sample drawn randomly from the general Norwegian working-age population with a high response frequency. The design was prospective and included the measurement of a comprehensive set of exposures and further adjustments.
Despite a non-response frequency of 33%, no systematic differences were found across the benchmarks of age, sex and region between respondents and non-respondents (25). Moreover, previous studies have shown that health problems do not necessarily differ between respondents and non-respondents and that some differences do not necessarily produce biased risk estimates (26).
A particular strength of this study was that we focused on exposure factors rather than on occupations. It has been suggested previously that using job titles as a proxy for occupational skin exposure underestimates variations in exposure within occupations or over time in the same job (27).
The lack of a validated instrument to measure exposures was a limitation of this study. Validated questions on several exposures, in particular to water, exist (27), but they have not been validated in the Norwegian working population. Nevertheless, the occupational exposure factors associated with skin problems in the present study were among the most common occupational exposures for the notified work-related skin diseases in Norway for the period 2000–2013 (14). Future studies should aim at validating self-reports of exposure.
The present study covers mainly subjectively experienced skin problems (illness) (28), where subclinical cases also may be included. Although illness data is usually self-reported (28), the fact that there was no clinically objective measure of the outcome at follow-up was a further limitation. However, our one-month prevalence estimate of 12% at follow-up is in accordance with the results from a Norwegian questionnaire study that applied a validated questionnaire for skin complaints (29).
Although we expect that the vast majority of skin problems represent hand eczema, other conditions, such as psoriasis and urticaria, may be part of our outcome entity.
As all data were collected by self-report, reporting bias and common method bias influencing exposure and outcome measures may have inflated the estimates. However, adjustment for baseline skin problems should have minimized the problem. Moreover, the questions about skin exposures and skin problems were among questions on other topics, and had different types of response categories, and questions regarding occupational exposures were asked before questions about health problems. These factors may have reduced common method bias (30).
In conclusion, the findings of this study indicate the contribution of work-environment factors to the risk of skin problems in a general working population, hence suggesting a potential for prevention via the reduction of known risk factors. Future epidemiological studies and surveillance of occupational dermatoses should include the assessment of physical factors and the effect of concomitant exposures.
ACKNOWLEDGEMENTS
JPT is a Lundbeck Foundation Fellow and is supported by an unrestricted grant. The other authors received no funding.
The authors are grateful for networking support from the COST Action TD1206 StanDerm. The authors offer special thanks to Marit Skogstad and Karl-Christian Nordby for their comments on this manuscript.
The authors declare no conflicts of interest.

1http://www.medicaljournals.se/acta/content/?doi=10.2340/00015555-2135
REFERENCES
