Svetlana Bobko1, Claudia Zeidler2, Nani Osada3, Claudia Riepe2, Bettina Pfleiderer4, Esther Pogatzki-Zahn5, Andrey Lvov1 and Sonja Ständer2*
1Moscow Scientific and Practical Center of Dermatovenerology and Cosmetology, Moscow, Russia, 2Center for Chronic Pruritus, Department of Dermatology, 3Institute of Medical Informatics, 4Department of Clinical Radiology, and 5Department of Anesthesiology, Intensive Care and Pain Therapy, University Hospital Münster, Von-Esmarch-Str. 58, DE-48149 Münster, Germany. *E-mail: sonja.staender@uni-muenster.de
Accepted Sep 1, 2015; Epub ahead of print Sep 4, 2015
Prurigo nodularis (PN) is characterized by the presence of intensely itchy nodules and papules, which are frequently refractory to therapy (1). The results of previous morphological studies indicate that nerve fibres have an important function in PN; in support of this, a dermal neuronal hyperplasia was observed in immunohistochemical studies (2, 3), although this could not be confirmed in histological analysis (4). As intraepidermal nerve fibres have been identified to be of great importance for the sensation of pruritus (5), we investigated them in PN (6). Surprisingly, decreased intraepidermal nerve fibre density (IENFD) independent of clinical parameters was found (6). With this, we hypothesized that reduced nerve fibre density might be due to scratching and, accordingly, that hypoplasia normalizes during healing of PN. To further investigate the role of nerve fibres in PN, we examined the IENFD of PN at different stages.
MATERIALS AND METHODS
Skin biopsies (4 mm) from representative lesional (n = 30), inter-lesional (n = 23; area between nodules) and non-lesional areas (n = 24; outside affected areas, no nodules, normally looking skin) and healed skin (n = 21; previous nodules present, no itch present) were obtained in local anaesthesia from patients with typical clinical features of PN (19 women, 11 men; age range 18–83 years; mean age 54.9 ± 17.1 years; median 55 years). Before biopsies were obtained, patients gave their written informed consent. Biopsies were fixed in 4% paraformaldehyde/PBS (Morphisto, Frankfurt, Germany) for 2 h and were then prepared for immunostaining with an antibody against protein gene product 9.5 (PGP 9.5; rabbit polyclonal, 1:200, Zytomed, Berlin, Germany) and for an assessment of IENFD, as previously described (6). The intraepidermal fibres of 3 30-mm cryosections from each biopsy were counted for their intraepidermal nerve fibres by a trained blinded observer according the guideline counting rules (7) using an Olympus BX43XC10 (Olympus, Hamburg, Germany). The length of the epidermis was measured with Olympus cellSens Dimensions (version 1.7) software (Olympus, Tokyo, Japan). The IENFD was calculated as the mean number of nerve fibres per mm epidermal length (IENFD fibres (F)/mm).
Data were collected and encoded using Microsoft Excel for Windows XP Professional and statistical analysis completed using SPSS for Microsoft Windows version 22 (SPSS Inc., Chicago, IL, USA). Comparisons of PN biopsies with normal, non-lesional skin and healed skin were performed using the Wilcoxon, Mann-Whitney, Kruskal–Wallis and Friedmann tests. A 2-sided significance test was performed for each statistical test, for which p ≤ 0.05 was considered statistically significant.
This study was approved by the local ethics committee and has been registered in the German Clinical Trials Register (Deutsches Register Klinischer Studien, DRKS, No. DRKS00008006).
RESULTS
Thirty patients with PN with different underlying diseases (Table SI1) were included in this study. The majority of patients (70%) had a combination of more than one disease responsible for pruritus. The mean pruritus intensity on the visual analogue scale (VAS), on the day the biopsy was obtained, was 4.8 ± 3.1; in the past 4 weeks the mean VAS was 5.9 ± 2.6 and the worst 7.6 ± 3.0. The quality of the symptom was described as itching (100% of patients), burning (54.3%), stinging (25%), painfulness (33.3%), pricking (45.8%), needle pricking (12.5%), feeling of warmth (16.7%) and formication (8.3%).
Biopsies from 30 patients were obtained from different representative areas of the body (Table SII1). The IENFD was dependent on topography in lesional (p = 0.011; Kruskal–Wallis test) and inter-lesional skin (p = 0.03, Kruskal–Wallis test), but not non-lesional or healed skin areas. Statistically significant differences were seen between IENFD from arm and leg lesional areas (Mann-Whitney test, p = 0.016), trunk and leg lesional areas (Mann-Whitney test, p = 0.010) and inter-lesional areas (Mann-Whitney test, p = 0.013), respectively.
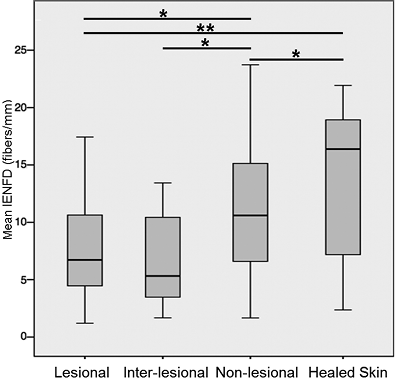
Comparing the IENFD from the whole group of patients and the 30 collected biopsies, the IENFD was lowest in lesional and inter-lesional skin and higher in non-lesional and healed skin. We selected 14 biopsies for further statistical analysis, thus allowing for an intra-individual comparison of identical biopsy localization, confirming our finding (Table SII1, Fig. 1). The Wilcoxon test showed a significant difference between the IENFD of lesional skin (7.4 ± 5.5 F/mm; p = 0.035) and inter-lesional skin (7.0 ± 7.3 F/mm; p = 0.016) compared with non-lesional skin (10.2 ± 6.1 F/mm). Furthermore, the difference between lesional and healed skin (13.4 ± 6.6 F/mm; p = 0.009) revealed a significant difference compared with non-lesional and healed skin (p = 0.04). Interestingly, there was no difference between the IENFD of lesional and inter-lesional PN biopsies (p = 0.397) nor between inter-lesional and healed skin (p = 0.123). There was also no correlation of IENFD at the various stages with the age of patients.
DISCUSSION
PN may be induced by various underlying diseases, but clinics and histology are similar in all affected patients. As demonstrated here, this also refers to cutaneous neuronal changes. There was a significant reduction in the IENFD in lesional PN skin compared with non-lesional skin, as previously described (6). Interestingly, inter-lesional skin exhibited a similar reduction in IENFD, which was statistically significantly compared with non-lesional skin. Thus, IENFD in lesional skin (nodules) and the inter-lesional skin between nodules seem to be similar in patients with PN. As inter-lesional PN skin is frequently lichenified and thickened, these results support the assumption that scratching or rubbing leads to reduced epidermal nerve fibres. Alongside the healing of nodules, epidermal innervation returns to normal values accompanied by clinical cessation of pruritus. However, the reduced IENFD might also indicate small fibre neuropathy (SFN) in PN. In the past few years, cutaneous small fibres, such as C and Aδ- fibres, have been found to be involved in mediation of pruritus (8). In neurology, the detection of reduced IENFD in skin biopsies is used as a sensitive and specific method to detect SFN, which may be clinically associated with pain and paraesthesia, such as burning (53.7% of patients) (7, 9). Our patients also reported a sensation similar to burning (54.3%); however, this sensation is not statistically correlated with reduced IENFD in different areas in our study. Neuropathy was previously thought to be involved in PN emergence (10, 11). Many patients with PN respond to therapies used to treat neuropathic pain, such as gabapentin and pregabalin (12), suggesting a neuropathic contribution in these patients. The aetiology of SFN in PN is currently unknown. Diabetes mellitus (DM), for example, is a common cause of SFN (7, 9); however, only 3 of our patients were diagnosed with DM. Moreover, the localized and transient nature of reduced IENFD excludes a generalized SFN and rather suggests delayed re-innervation of the lesioned sites.
In summary, this study showed that hypoplasia of epidermal nerves is an important finding for PN in lesional and inter-lesional areas. It can normalize during healing, paralleling relief of pruritus. By identifying SFN factors and testing PN using skin biopsies to identify neuronal mediator patterns or quantitative sensory testing, future studies investigating the functional activity of small fibres will elucidate the interesting association between SFN and PN.
ACKNOWLEDGEMENTS
The authors would like to thank E. R. Burnett for editing this manuscript. This work was supported by a grant from the Interdisciplinary Center for Clinical Research (IZKF; CTRP 07 to SST and EPZ) and a Russian presidential grant for the SB scholarship.

1http://www.medicaljournals.se/acta/content/?doi=10.2340/00015555-2232
REFERENCES
