Pauliina Nuutinen1, Ilkka T. Harvima2 and Leena Ackermann1
1Hospital for Skin and Allergic Diseases, Helsinki University Central Hospital, Helsinki, and 2Department of Dermatology, Kuopio University Hospital, Kuopio, Finland
In addition to histamine, leukotriene C4 (LTC4) might also play a role in mediating cold urticaria wheals. To study the significance of LTC4 vs. histamine, 6 patients with cold urticaria were challenged with the ice cube test before and after ingestion of 10 mg cetirizine (antihistamine), 10 mg montelukast (leukotriene antagonist) or a combination of both drugs. Cetirizine diminished the cold-induced wheal by 50 ± 42%. Montelukast had no significant effect, and the combination of both drugs diminished the wheal by 37 ± 33%. Furthermore, a skin microdialysis technique detected the release of histamine in the cold-induced wheal, whereas no LTC4 release was detected. In conclusion, the antihistamine is effective and histamine is released, whereas the leukotriene antagonist is not effective and LTC4 is not released in the cold urticaria wheal. Key words: cold urticaria; histamine; LTC4; skin microdialysis.
(Accepted August 25, 2006.)
Acta Derm Venereol 2007; 87: 9–13.
Leena Ackermann, MD, PhD, Hospital for Skin and Allergic Diseases, Helsinki University Central Hospital, Meilahdentie 2, FIN-00250 Helsinki, Finland. E-mail: leena.ackermann@hus.fi
In the pathophysiology of urticaria, mast cells are considered to be the major effector cells. Although mast cell-derived histamine is thought to be the principal inflammatory mediator in urticaria, other vasoactive or pro-inflammatory mediators are released or generated after mast cell activation, e.g. prostaglandin D2 (PGD2), leukotriene C4 (LTC4), proteases, kinins, neuropeptides and cytokines (1). Antihistamines are the mainstay of treatment for urticaria. As the pathophysiological mechanisms became better understood, therapeutic agents other than H1 antihistamines, have also been used in the treatment of urticaria, e.g. doxepin (2), cyclosporine (3), phototherapy (4) and leukotriene antagonists (5, 6).
Approximately 20% of chronic urticaria has various physical causes. In cold urticaria, the symptoms are caused by skin exposure to cold, e.g. cold wind, swimming in cold water, handling cold objects, eating ice-cream or drinking cold drinks. Depending on the type of urticaria concerned, the mediators released may differ according to the mechanism that activates the mast cells.
The release of histamine in patients with cold urticaria has been shown by many groups (7–10). However, investigations concerning other mediators besides histamine in cold urticaria are few. PGD2 (9, 11), leukotriene E4 (12), chemotactic factors (13, 14), platelet activating factor (PAF) (14) and platelet factor 4 (PF4) (13) have been shown to be released in cold urticaria. Also, tumour necrosis factor alpha (TNF-α) and interleukin-3 (IL-3) have been shown to be upregulated in the skin 30 min after a positive ice cube test (15). Patients with cold urticaria who get systemic symptoms have TNF-α in their blood circulation a few minutes after cold exposure (16).
H1 antihistamines have been the mainstay of treatment in cold urticaria, but the clinical responses are highly variable (2, 17). Therefore, studies concerning other drugs are needed. There are several reports in which leukotriene antagonist treatment has shown to be effective in patients with chronic urticaria (18–20). Also, 2 case reports showed effectiveness of leukotriene antagonist treatment in patients with cold urticaria (5, 6). However, in a large study of 160 patients, leukotriene antagonists were not shown to be effective as add-on therapy with antihistamines in chronic urticaria (21). One study has suggested that patients with a positive autologous serum skin test are more likely to respond to treatment with a leukotriene antagonist (22). However, leukotriene synthesis inhibitor and leukotriene antagonist alone did not have any significant inhibitory effect on the allergic prick-test wheal (23).
Cold urticaria is often difficult to treat and the symptoms may not be controlled by antihistamines alone in most patients. The aim of this study was to compare the effect of antihistamine, leukotriene antagonist and the combination of both drugs on the size of the wheal reaction after an ice cube test in patients with cold urticaria. We also measured the release of histamine and LTC4 in the wheal reaction using a microdialysis method in these same patients.
MATERIALS AND METHODS
Patients
Six patients (2 men, 4 women, age 26–48 years, mean 34 years) with previously documented cold urticaria (typical symptoms following exposure to cold and a positive ice cube test) were included in this study after giving written informed consent. In these patients, the mean duration of symptoms was 6.1 years. Three healthy subjects with no symptoms following exposure to cold and a negative ice cube test (3 women, age range 30–39 years, mean 34.5 years) served as controls. None of the subjects showed dermographism. Cryoglobulins and cold agglutinins were negative in all subjects studied, and cold urticaria secondary to other diseases was ruled out by extensive laboratory work-up (24). The patients had not received any systemic antihistamine, leukotriene antagonist or other immunomodulative medication for at least 2 weeks before entering the study. The methods used in this study were approved by the Ethics Committee of Helsinki University Hospital, Helsinki, Finland.
Skin challenge
A metallic tube with a flat round bottom (diameter 4 cm), which was routinely used for cold urticaria testing at the University Hospital of Helsinki, was filled with small ice cubes. A round area of the skin on the ventral right forearm was exposed to cold with this tube for 5, 10 and 20 min. This method allows close contact of the skin with the ice-cold metal, avoids melting of the ice cubes, and the diameter of the cold contact on the skin is constant. Ten minutes after the cold exposure the wheal reactions were outlined with a pen through a transparent plastic film. Then the marked area of film was cut out with scissors and the plastic pieces were weighed. In addition, pieces of known diameter and area were weighed in order to plot a standard curve, and thereby the size of the wheals was calculated (25). In addition, the thickness of the wheal reaction was evaluated by a visual score from 1 (slightly elevated) to 3 (clearly elevated). The time point (5, 10 or 20 min) with the largest wheal reaction was selected for further studies in each patient. The patients were then given an antihistaminic drug; cetirizine 10 mg (Histec®, Orion Pharma, Espoo, Finland), followed by a 60 min waiting period (the maximal plasma concentration of the drug is achieved within 30–60 min). Thereafter, the ice cube test was repeated on the left forearm and the wheal reaction was documented as described above. The same procedure was also performed after a one week clearance period, but the drug used was a leukotriene antagonist; montelukast 10 mg (Singulair, MSD, Haarlem, Holland). The maximal plasma concentration of this drug is achieved after 3 h, thus the second ice cube test was performed after 3 h. Finally, again at least one week later, the same challenge was performed using both drugs combined; cetirizine 10 mg + montelukast 10 mg, followed by a wait of 3 h before the second ice cube test was performed.
Microdialysis to monitor mediator release
The procedure for microdialysis has been described previously (25–28). Isotonic saline solution (Ringersteril, Orion Corporation, Medipolar, Oulu, Finland) was perfused through the system by a microinjection pump at a rate of 3.3 µl/min. In this study, a probe (CMA/20, CMA Microdialysis, Stockholm, Sweden) with a shaft length of 25 mm and a membrane length of 10 mm was used. The membranous part of the probe was 0.5 mm thick. Plastic tubing carries the perfusate to the microfraction collector and, in this study, 49.5 µl samples were collected. The samples were stored at –20ºC prior to analysis.
Two probes were inserted into the dermis of the volar aspect of the forearm, as superficially as possible so that it made a clear bump in the skin (26). One hour after the probe insertion, the baseline sample was collected for 30 min, and 90 min after the probe insertion, the skin was challenged. A metallic round tube, of 4 cm diameter, was filled with small ice cubes and placed on the skin where the probe was located. The metallic tube was placed above both probes for 10 min, after which 15-min fractions were collected for 2 h.
Analysis of histamine and LTC4
Histamine was analysed in duplicate using a radioenzyme assay with a detection limit of 0.5–1.0 nmol/l (26). LTC4 was analysed by using a commercial enzyme immunoassay kit (Leukotriene C4 EIA kit; Cayman Chemical, USA), which required a 90 µl sample and had a detection limit of 10 pg/ml. Because of the larger volume required for LTC4 analysis, two consecutive fractions were pooled.
RESULTS
Histamine is released in the cold-induced wheal
The baseline histamine concentrations before the ice cube challenge in the 6 patients with cold urticaria were below the assay detection limit. After the ice cube challenge, the first 15-min fraction showed a slight increase in the histamine concentration (32 ± 69 nM, mean ± SD), but thereafter, a clear rise was found in the 15–30 min fraction (347 ± 507 nM). A decline in the histamine concentration was observed in the subsequent 15-min fractions for up to 2 h (71.5 ± 59 nM, 10.0 ± 11 nM, 1.7 nM ± 4 nM, 0.0 nM, 0.0 nM, 0.0 nM, respectively). Therefore, a rapid release and no delayed release of histamine was observed.
Two of the 6 patients with cold urticaria showed high peak concentrations of histamine (up to 621 and 1269 nM), whereas the remaining 4 patients revealed clearly lower peak concentrations (up to 21–100 nM) during the 2-h sampling period (Fig. 1).
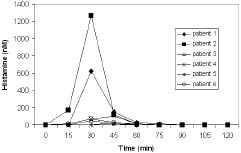
Fig. 1. Individual histamine release (in nanomoles (nM) per litre) after ice cube challenge in 6 patients with cold urticaria.
In the 3 healthy control subjects, the mean baseline histamine concentration before the ice cube challenge was below the detection limit. After the ice cube challenge, all subsequent 15-min samples showed only low histamine concentrations (from 0 to 10 nM).
Leukotriene C4 is not released in the cold-induced wheal
In the 6 patients with cold urticaria, the mean baseline LTC4 concentration was 17 ± 19 pg/ml (mean ± SD). After the ice cube challenge, the mean LTC4 concentrations in the subsequent 30-min fractions were 11 ± 24 pg/ml, 18 ± 25 pg/ml, 12 ± 25 pg/ml and 11 ± 27 pg/ml, respectively, i.e. no release was detected.
In the 3 healthy control subjects, the mean baseline LTC4 concentration was 40 ± 4 pg/ml. After the ice cube challenge, the mean LTC4 concentrations in the subsequent 30-min fractions were 37 ± 8 pg/ml, 33 ± 11 pg/ml, 40 ± 4 pg/ml and 41 ± 7 pg/ml, respectively.
Effect of cetirizine and montelukast on the wheal reaction
Peroral cetirizine 1 h prior to the ice cube challenge diminished the area of the wheal reaction by an average of 50 ± 42% (mean ± SD) (Fig. 2). It also had an effect on the thickness of the wheal reaction; mean change in the wheal thickness was –1.66 (visual score from 0; not elevated, to 3; clearly elevated).
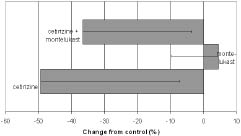
Fig. 2. Effect of peroral cetirizine, montelukast or combination of both drugs on the area of the wheal reaction induced by an ice cube challenge in 6 patients with cold urticaria. Grey area and bar indicate mean and SD respectively.
Montelukast administered 3 h prior to the ice cube re-challenge enlarged the wheal reaction slightly by an average of 4 ± 14% and did not have any effect on the thickness of the wheal reaction.
The combination of both drugs administered 3 h prior to the ice cube re-challenge diminished the area of the wheal reaction by an average of 37 ± 33%. Therefore, the combination of both drugs appeared to be rather less effective than cetirizine alone. Also, the drug combination was somewhat less effective in diminishing the thickness of the wheal reaction (mean change in the wheal thickness was only –1).
The effects of antihistamine and leukotriene antagonist medications on the wheal reaction did not correlate to the total amount of histamine or LTC4 released within 2 h in each patient.
DISCUSSION
Cold urticaria is easy to diagnose, but often difficult to manage. The clinical efficacy of H1 antihistamines in preventing and controlling symptoms of cold urticaria is often not satisfactory (29). Previously, 2 case reports in which leukotriene antagonist treatment was shown to be effective in patients with cold urticaria have been published (5, 6)
This study examined the effects of cetirizine and montelukast on wheal size in 6 patients with cold urticaria whose skin was challenged with the ice cube test. It also monitored histamine and LTC4 release using a microdialysis method that allows accurate kinetic measurements of these mediators in extracellular fluids, mediators which are known to be released upon mast cell activation in the skin. Three healthy controls served as the control group. All 6 patients with cold urticaria showed a marked reduction in the wheal size and oedema in the ice cube test after cetirizine. However, there was no reduction in the wheal size or dermal oedema after montelukast. Furthermore, the combination of montelukast with cetirizine did not give rise to additional effect. All 6 patients showed release of histamine after the ice cube test, but no marked release of LTC4 was seen compared with baseline values. Somewhat similar results have been obtained in stinging nettle-induced urticaria with no release of LTC4 and only weak release of histamine (30). Previously, using exactly the same investigation procedure, the release of LTC4 has been demonstrated after allergen challenge (25, 27, 28). Therefore, this method has been proven reliable in measuring the release of LTC4.
The extent of histamine release in the cold urticaria wheal showed wide variation, and the peak histamine concentration in the microdialysis fractions varied from 21 to 1269 nM. In patients with low histamine release, other mast cell mediators than histamine and LTC4 may be crucial for the clinical wheal reaction and therefore antihistamines may not be sufficiently effective. It is also possible that in patients with very high histamine release, the efficacy of an antihistamine is not sufficient to prevent the wheal. In the patient with the highest histamine release (77.9 pmol in 120 min), cetirizine reduced the wheal size by 10.2%, and in the patient with the lowest histamine release (1.5 pmol in 120 min), cetirizine reduced the wheal size by 17%. However, there was variation among patients and the relation between the effect of cetirizine and the extent of histamine release needs to be studied in a larger patient group in the future.
An interesting result is that LTC4 release occurs in allergic prick-test wheals (25, 27, 28), but not in stinging nettle-induced wheals (30) or in cold urticaria wheals. One explanation could be that in allergic prick-test wheals the mast cells are activated by IgE-dependent mechanisms in which both histamine and LTC4 are released. However, if mast cells are stimulated with neuropeptides, such as substance P, similar amounts of histamine are released, but 20-fold less LTC4 (31). It is possible that sensory nerves and neuropeptides are involved in mast cell activation in cold urticaria wheals, as has been suggested previously (32), and thus no marked LTC4 release occurs. Bagenstose et al. (22) showed in their study that patients with a positive autologous serum skin test are likely to respond to treatment with a leukotriene antagonist compared with patients with a negative test. In these patients the mast cells are activated by IgE-dependent mechanisms, suggesting that both histamine and LTC4 are released. It appears that leukotriene antagonists are not effective in the treatment of cold urticaria and the powerful mediator LTC4 is not released to any marked extent in the cold urticaria wheal. However, it is possible that occasional patients may benefit from these drugs affecting leukotriene activity, as has been described in two case reports (5, 6). To clarify this further, studies with a larger patient population are needed in order to evaluate the efficacy of leukotriene antagonist medication in the treatment of cold urticaria. Studies concerning other mediators, such as neuropeptides and cytokines, in cold urticaria are also needed.
ACKNOWLEDGEMENTS
The authors thank The Finnish Association of Dermatologists and the Finnish Association of Immunology and Allergology for research grants, the Hospital for Skin and Allergic Diseases at Helsinki University Central Hospital and Kuopio University Hospital for financial support, and Ms Katja Dufva for expert technical assistance.
There are no conflicts of interest to report.
References
1. Doutre MS. Physiopathology of urticaria. Eur J Dermatol 1999; 9: 601–605.
2. Neittaanmäki H, Myöhänen T, Fräki JE. Comparison of cinnarizine, cyproheptadine, doxepin, and hydroxyzine in treatment of idiopathic cold urticaria: usefulness of doxepin. J Am Acad Dermatol 1984; 11: 483–489.
3. Marsland AM, Beck MH. Cold urticaria responding to systemic ciclosporin. Br J Dermatol 2003; 149: 214–215.
4. Hannuksela M, Kokkonen EL. Ultraviolet light therapy in chronic urticaria. Acta Derm Venereol 1985; 65: 449–450.
5. Hani N, Hartmann K, Casper C, Peters T, Schneider LA, Hunzelmann N, et al. Improvement of cold urticaria by treatment with the leukotriene receptor antagonist montelukast. Acta Derm Venereol 2000; 80: 229.
6. Bonadonna P, Lombardi C, Senna G, Canonica GW, Passalacqua G. Treatment of acquired cold urticaria with cetirizine and zafirlukast in combination. J Am Acad Dermatol 2003; 49: 714–716.
7. Kaplan AP, Garofalo J, Sigler R, Hauber T. Idiopathic cold urticaria: in vitro demonstration of histamine release upon challenge of skin biopsies. N Engl J Med 1981; 305: 1074–1077.
8. Neittaanmäki H, Karjalainen S, Fräki JE, Kiistala U. Suction blister device with regulation of temperature: demonstration of histamine release and temperature change in cold urticaria. Arch Dermatol Res 1984; 276: 317–321.
9. Ormerod AD, Kobza-Black A, Dawes J, Murdoch RD, Koro O, Barr RM, et al. Prostaglandin D2 and histamine release in cold urticaria unaccompanied by evidence of platelet activation. J Allergy Clin Immunol 1988; 82: 586–589.
10. Andersson T, Wårdell K, Anderson C. Human in vivo cutaneous microdialysis: estimation of histamine release in cold urticaria. Acta Derm Venereol 1995; 75: 343–347.
11. Heavey DJ, Kobza-Black A, Barrow SE, Chappell CG, Greaves MW, Dollery CT. Prostaglandin D2 and histamine release in cold urticaria. J Allergy Clin Immunol 1986; 78: 458–461.
12. Maltby NH, Ind PW, Causon RC, Fuller RW, Taylor GW. Leukotriene E4 release in cold urticaria. Clin Exp Allergy 1989; 19: 33–36.
13. Wasserman SI, Ginsberg MH. Release of platelet factor 4 into the blood after cold challenge of patients with cold urticaria. J Allergy Clin Immunol 1984; 74: 275–279.
14. Grandel KE, Farr RS, Wanderer AA, Eisenstadt TC, Wasserman SI. Association of platelet-activating factor with primary acquired cold urticaria. N Engl J Med 1985; 313: 405–409.
15. Hermes B, Prochazka AK, Haas N, Jurgovsky K, Sticherling M, Henz BM. Upregulation of TNF-α and IL-3 expression in lesional and uninvolved skin in different types of urticaria. J Allergy Clin Immunol 1999; 103: 307–314.
16. Tillie-Leblond I, Gosset P, Janin A, Dalenne R, Joseph M, Wallaert B, et al. Tumor necrosis factor-α release during systemic reaction in cold urticaria. J Allergy Clin Immunol 1994; 93: 501–509.
17. Neittaanmäki H, Fräki JE, Gibson JR. Comparison of the new antihistamine acrivastine (BW 825C) versus cyproheptadine in the treatment of idiopathic cold urticaria. Dermatologica 1988; 177: 98–103.
18. Ellis MH. Successful treatment of chronic urticaria with leukotriene antagonists. J Allergy Clin Immunol 1998; 102: 876–877.
19. Tedeschi A, Suli C, Lorini M, Airaghi L. Successful treatment of chronic urticaria. Allergy 2000; 55: 1097–1098.
20. Nettis E, Colanard MC, Paradiso MT, Ferrannini A. Desloratadine in combination with monelukast in the treatment of chronic urticaria: a randomized, double-blind, placebo-controlled study. Clin Exp Allergy 2004; 34: 1401–1407.
21. Di Lorenzo G, Pacor ML, Mansueto P, Esposito Pellitteri M, Lo Bianco C, Ditta V et al. Randomized placebo-controlled trial companing desloratadine and monelukast in monotherapy and desloratadine plus monelukast in combined therapy for chronic idiopathic urticaria. J Allergy Clin Immunol 2004; 114: 619–625.
22. Bagenstose SE, Levin L, Bernstein JA. The addition of zafirlukast to cetirizine improves the treatment of chronic urticaria in patients with positive autologous serum skin test results. J Allergy Clin Immunol 2004; 113: 134–140.
23. Saarinen JV, Harvima RJ, Horsmanheimo M, Harvima IT. Modulation of the immediate allergic wheal reaction in the skin by drugs inhibiting the effects of leukotriene C4 and prostaglandin D2. Eur J Clin Pharmacol 2001; 57: 1–4.
24. Neittaanmäki H. Cold urticaria: clinical findings in 220 patients. J Am Acad Dermatol 1985; 13: 636–644.
25. Saarinen JV, Harvima RJ, Naukkarinen A, Horsmanheimo M, Harvima IT. Release of histamine and leukotriene C4 in immediate allergic wheal reaction as measured with the microdialysis technique. Arch Dermatol Res 2000; 292: 333–340.
26. Horsmanheimo L, Harvima IT, Harvima RJ, Ylönen J, Naukkarinen A, Horsmanheimo M. Histamine release in skin monitored with the microdialysis does not correlate with the wheal size induced by cow allergen. Br J Dermatol 1996; 134: 94–100.
27. Horsmanheimo L, Harvima IT, Harvima RJ, Brummer-Korvenkontio H, Francois G, Reunala T. Histamine and leukotriene C4 release in cutaneous mosquito-bite reactions. J Allergy Clin Immunol 1996; 98: 408–411.
28. Annila I, Saarinen JV, Nieminen MM, Moilanen E, Hahtola P, Harvima IT. Bee venom induces high histamine or high leukotriene C4 release in skin of sensitized beekeepers. J Invest Allergol Clin Immunol 2000; 10: 223–228.
29. Kennard CD, Ellis CN. Pharmacologic therapy for urticaria. J Am Acad Dermatol 1991; 25: 176–187.
30. Taskila K, Saarinen JV, Harvima IT, Harvima RJ. Histamine and LTC4 in stinging nettle-induced urticaria. Allergy 2000; 55: 679–680.
31. Benyon RC, Robinson C, Church MK. Differential release of histamine and eicosanoids from human skin mast cells activated by IgE-dependent and non-immunological stimuli. Br J Pharmacol 1989; 97: 898–904.
32. Toth-Kasa I, Jancso G, Obal F Jr, Husz S, Simon N. Involvement of sensory nerve endings in cold and heat urticaria. J Invest Dermatol 1983; 80: 34–36.
