Bong Seon Kang1, Seung Dong Lee1, Young Min Park1, Soo Yeon Cho2 and Hoon Kang1*
Departments of 1Dermatology and 2Urology, St. Paul’s Hospital, College of Medicine, The Catholic University of Korea, St. Paul’s Hospital, 620-56 Jeon Nong-Dong, Dong Dae Moon-Ku, Seoul, 130-709, Korea. *E-mail: johnkang@catholic.ac.kr
Accepted October 26, 2009.
Sir,
Pseudoepitheliomatous keratotic and micaceous balanitis (PKMB) is a condition that occurs on the glans penis of older men and may be associated with the development of a verrucous carcinoma. The exact aetiology of PKMB is largely unknown. Human papillomavirus (HPV) infection has been demonstrated in verrucous carcinoma of the genitalia and other anatomical site but has never been found in PKMB. We report here the case of a 62-year-old man who developed a PKMB on the glans penis. Using a broad-spectrum PCR technique and restriction fragment mass polymorphism for identifying HPV, the epidermis of the area of PKMB was examined and HPV type 81 was identified.
CASE REPORT
A 62-year-old Korean man was referred to our department due to a solitary slowly growing plaque on the glans penis. The lesion had been present for more than 30 months. The original penile mass had been completely excised in the Department of Urology under the diagnosis of condyloma accuminata approximately 13 months previously. However, a small lesion, similar to the previous one, was noted on the same site 5 months later. The patient had not undergone circumcision, was heterosexual, and did not report previous sexual promiscuity. He denied any urethral discharge, urinary difficulty or irritation of the glans penis.
Physical examination revealed an asymptomatic, shiny, white-to-yellowish, hyperkeratotic, 2 × 2.5 cm sized plaque confined to the right side of the urethral meatus. The peripheral margin of the plaque was well-demarcated with surrounding normal tissue and an abnormal blockage of urethral opening was not found (Fig. 1A). The penile shaft, scrotum and inguinal skin were normal and the general physical examination was also otherwise unremarkable.
An excisional biopsied specimen from the centre of the lesion showed extensive hyperkeratosis, parakeratosis, acanthosis, pseudoepitheliomatous hyperplasia and a sparse mononuclear cell infiltration in the upper dermis with no frank malignancy or cellular atypia (Fig. 1B). The findings were consistent with a diagnosis of PKMB.
Fig. 1. (A) Well-defined hyperkeratotic plaque with shiny, micaceous scales on the glans penis. (B) Photomicrograph showing marked hyperkeratosis, parakeratosis, acanthosis and an inflammatory cell infiltrate (haematoxylin & eosin; original magnification ×100).
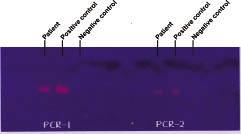
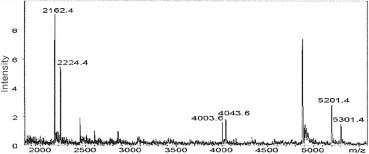
Using the broad-spectrum PCR technique, the hyperplastic epidermis of the lesion was examined and HPV DNA was identified (Fig. 2). Plasmid clones, known HPV-positive cervical tissues were used as positive controls. Matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF MS) assay, termed restriction fragment mass polymorphism (RFMP) that is suitable for genotyping multiple HPV in an accurate and sensitive manner (1), showed positive signals compatible with type 81 in the hyperplastic epidermis of the lesion (Fig. 3). The DNA sequence of the genotype determinant region was AATGGCATTTGTTGGTTTAATGAAATGTTT.
Fig. 2. The excised specimen was examined by PCR for the detection of human papillomavirus (HPV) DNA with two pairs of primers. On both PCR-1 and PCR-2, the first column is the patient’s specimen, the second is the positive control, and the third is the negative control. The photograph shows positive results, with HPV DNA in the specimen of our patient and the positive control.
Fig. 3. Restriction fragment mass polymorphism showing the intensity of signals compatible with human papillomavirus type 81 in the excised specimen.
The patient was treated with wide excision and was circumcised. There has been no evidence of recurrence on the follow-up examinations for 2 years after excision.
DISCUSSION
PKMB is a rare, acquired disease of the glans penis, which occurs exclusively in older men. It is characterized by progressive hyperkeratotic plaques and sheets of mica-like scales, often leading to phimosis. It was first described by Lortat-Jacob & Civatte in 1961 (2). The term “micaceous” refers to the white, scaly appearance of the lesions.
The lesions tend to progress slowly and recur locally. Once assumed to be a benign condition, there is now growing evidence that it should be considered as a premalignant condition or a locally invasive low-grade malignant lesion, which is associated with the development of verrucous carcinoma (3–7).
The exact pathomechanism of PKMB is unknown. Some authors suggest that HPV may be associated with PKMB, but, until now, no one has detected the virus in a PKMB lesion. Genital HPV prevalence of heterosexual men ranges from 3.5% to 45% (8). HPV detection of our case may be a confounding factor or genuine aetiology, but this is the first case of PKMB with positive HPV DNA in PCR and RFMP. Our findings provide supportive evidence that HPV may be associated with the development and recurrence of PKMB. The apparent detection of HPV DNA suggests not only a pathogenetic role for HPV in PKMB, but also its possibility of transformation to verrucous carcinoma. Therefore, it is worthwhile to perform studies on patients with PKMB for the detection of HPV DNA as a marker of transformation to verrucous carcinoma.
PKMB is treated most successfully by local excision. However cryotherapy, topical 5-fluorouracil (5) and subcutaneous interferon-α (9) have been reported as effective treatments for PKMB.
REFERENCES