Nobuyuki Kikuchi and Toshiyuki Yamamoto
Department of Dermatology, Fukushima Medical University, Hikarigaoka 1, Fukushima 960-1295, Japan. E-mail: nobuyuk@fmu.ac.jp
Accepted Nov 5, 2012; Epub ahead of print Mar 5, 2013
Palmoplantar pustulosis (PPP) is a chronic disease characterized by sterile pustules on the palms and soles. Focal infections are closely associated with exacerbation of PPP, often accompanied by arthralgia. Tonsillitis is the most common culprit, whereas reports on dental infection are scarce (1). We describe here 4 cases of PPP in which dental infection is suggested to play a triggering role in the induction or deterioration of the disease.
CASE REPORTS
Case 1. A 60-year-old man had been treated for PPP for 3 years. He was a non-smoker. Two months previously, his skin eruptions suddenly worsened and spread beyond the palmoplantar areas. Simultaneously, severe joint pain appeared on the sternocostoclavicular areas, shoulder and sacroiliac joints. On physical examination, small pustules and scales were detected on the erythematous lesions on the palms and soles. In addition, scaly erythema and solitary pustules, which were sterile, were scattered on his trunk (Fig. 1a). Laboratory examination showed increased levels of C-reactive protein (CRP, 3.8 mg/dl, normal 0.00–0.30), white blood cell (WBC) count (9,800/μl, normal 3,800–9,800/μl), and normal anti-streptolysin O (ASO) titres were elevated (289 IU/ml, normal 0–244 IU/ml). Bone scintigraphy revealed increased uptake in the sternocostoclavicular joints (Fig. 1b), and X-ray of the head revealed dento-alveolar abscess and subsequent sinusitis. Administration of clarithromycin and application of corticosteroid ointment for the skin lesions resulted in improvement in both skin lesions and joint pain (Fig. 1c, d). Thereafter, only slight scaly erythema appeared occasionally on the soles during a 4-year follow-up period, with no recurrence of joint pain.
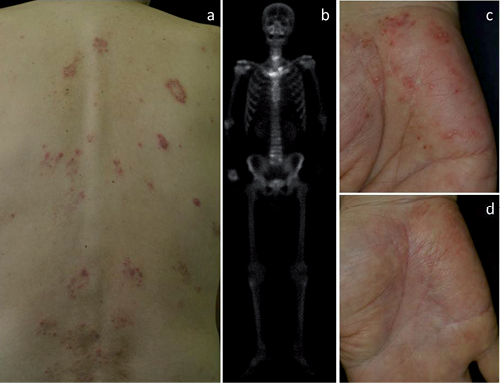
Fig. 1. (a) Scaly erythemas with tiny pustules were scattered on the back (Case 1). (b) Bone scintigraphy showing increased uptake in the right sternoclavicular joint and bilateral knees, and also sinusitis. Palmar lesions (c) before, and (d) after antibiotic therapy.
Case 2. A 61-year-old woman suddenly developed pustular lesions on the palms and trunk 5 days previously. Solitary sterile pustules were also scattered on the abdomen and back. She smoked 20 cigarettes of tobaccos a day. A skin biopsy from the pustule revealed neutrophilic abscesses in the epidermis. Laboratory data revealed a slight increase in CRP (0.69 mg/dl) and WBC (10,300/μl). ASO titres were elevated (289 IU/ml, normal 0–244 IU/ml), but laryngological examination revealed no abnormalities. Bone scintigraphy revealed an increased uptake of technetium 99 m in the sternocostoclavicular joints. Orthopantomography revealed resorption of the mandible alveolar bone due to periodontitis. Dental examination revealed abscess formation in the pocket of several teeth. Surgical extraction of 4 teeth of dental caries and the application of corticosteroid ointment for the skin lesions resulted in improvement in the skin lesions and in arthralgia. Although the patient did not give up smoking, cutaneous lesions were almost completely improved within one year, with no recurrence of arthralgia.
Case 3. A 49-year-old woman presented with diabetes mellitus. She had smoked 10 cigarettes of tobaccos a day for 30 years. She developed right knee pain one month previously, and pustular lesions appeared on her bilateral soles several days previously. Orthopantomography revealed a number of teeth with dental caries (Fig. S1; available from: http://www.medicaljournals.se/acta/content/?doi=10.2340/00015555-1552). Laboratory data showed increased CRP, but WBC counts were normal. Bone scintigraphy showed an increased uptake of technetium 99 m in both knees and in the sternocostoclavicular joints. Treatment for dental caries, by extraction of 10 teeth and application of corticosteroid ointment, resulted in a marked improvement in skin lesions. By contrast, joint pain was not significantly improved. The patient gave up smoking, and her skin lesions were almost completely resolved within several months.
Case 4. A 49-year-old woman developed pustular lesions on the palms and soles 9 months previously (Fig. S2a; available from: http://www.medicaljournals.se/acta/content/?doi=10.2340/00015555-1552). There was no associated arthralgia. She had smoked 10 cigarettes of tobaccos a day for 25 years. Laboratory examination revealed CRP, WBC and ASO titres within the normal range. The patient reported exudation of pus from the gingiva. Orthopantomography and computed tomography (CT) revealed a maxillary sinus cyst, which was surgically removed (Figs S2b and 2a). Histological diagnosis was inflammatory radicular cyst. A marked improvement in skin lesions was induced 2 months later (Fig. 2b). During a 2-year follow-up period, slight erythema appeared occasionally only on the sole, but the palmar lesions completely disappeared. The patient did not stop smoking.
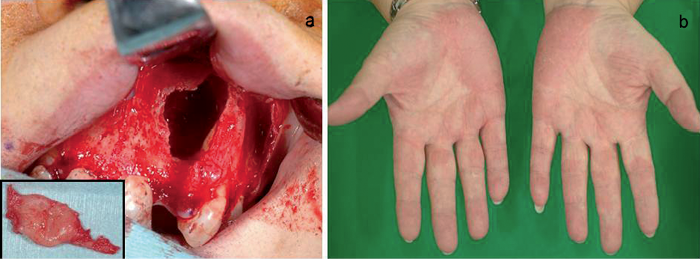
Fig. 2. (a) Surgery on the cystic nodule (inflammatory radicular cyst (insert). (b) Marked improvement after surgical operation.
DISCUSSION
None of the patients had a previous history of tonsillitis. Arthralgia was recognized in 3 patients, and 2 of them further developed extra-palmoplantar lesions. Dental treatment, with administration of antibiotics, led to improvement in the cutaneous lesions in all cases. In addition, dental treatment resulted in relief of pain in all 3 cases with arthralgia. Bacterial cultures of the dental caries were not performed.
Bacterial infection plays a significant role, in several ways, in PPP. Cutaneous lymphocyte antigen (CLA) expression on T cells is upregulated by bacterial infection (2), which migrates into the palmoplantar skin, along with enhanced cytokine production such as interleukin (IL)-6, tumour necrosis factor (TNF)-α, and interferon (IFN)-γ (3). Stimulation with α-streptococcal antigens upregulates CCR6 expression in tonsillar T cells, and expression of CCL20, a ligand of CCR6, is enhanced in the lesional skin of PPP (4), suggesting an important interaction between CCL20/CCR6. Heat shock proteins (HSPs) are recognized by γδ T-cell receptors and toll-like receptor (TLR)-2 and -4, and antibodies that react with HSP65 can be found in the sera of patients with PPP (5), suggesting that HSP-producing chronic infectious bacteria might trigger PPP (6). TLRs play a pivotal role in immune host defence against infectious pathogens, and activate innate immunity. Furthermore, bacterial products stimulate enhanced production of IL-23 (7), which triggers T cells to produce IL-17. IL-17 promotes neutrophil migration via the release of CXC chemokines (8). IL-23 is upregulated in the lesional skin of PPP (9), suggesting that IL-23/IL-17 inflammatory pathway is important in PPP.
Out of our 4 patients, 3 were women and all were smokers. Nicotine can influence cellular functions, such as induction of disturbances in polymorphic neutrophilic granulocyte chemotaxis and immunomodulation of macrophages. In vitro studies have shown that production of IL-1 and IL-8 are increased by nicotine stimulation in keratinocytes (10). Nicotine acetylcholine receptors are expressed in the eccrine glands, ducts and endothelium in the skin, which pattern is altered by smoking (11).
Pustulotic arthro-osteitis (PAO) is worsened by focal infections, e.g. streptococcal throat infection, and mitigated by systemic administration of antibiotics or the surgical removal of focal infections, i.e. tonsillectomy. T cells activated in the local areas may migrate into the skin. In the cases described here, all 3 patients with PAO were relieved of pain after treatment of the focal infection. Extra-palmoplantar lesions presenting thin, scaly erythemas, or solitary pustules occasionally appear on the forearms, elbows, the dorsa of the feet, lower legs, knees, and buttocks. The skin lesions appear on the trunk, with sudden onset, accompanied by joint pain, following focal infections (12). Two of our cases transiently exhibited extra-palmoplantar lesions, which disappeared earlier than the improvement in palmoplantar lesions.
REFERENCES
