Tomoyasu Hattori, Akihiko Uchiyama, Osamu Tago, Yayoi Nagai and Osamu Ishikawa
Department of Dermatology, Gunma University Graduate School of Medicine, Maebashi, Gunma, Japan
Mycosis fungoides usually follows an indolent clinical course. We report here a rapidly progressive case of mycosis fungoides with peculiar clinical and histological features, presenting as a haematoma-like mass on the thigh accompanied by multiple reddish brown erythematous lesions on the trunk and extremities. Histopathologically, the erythematous lesions showed epidermotropism of atypical T lymphocytes expressing CD4 and prominent syringotropism without syringometaplasia. The haematoma-like lesion consisted of diffuse and dense infiltrates of medium-to-large-sized pleomorphic lymphocytic cells expressing CD30, suggesting that CD30+ large-cell transformation had occurred. Mycosis fungoides presenting as a haematoma-like lesion is rare and may be a poor prognostic sign. Key words: mycosis fungoides; haematoma; large-cell transformation; syringotropism; CD30.
Accepted Dec 4, 2012; Epub ahead of print Mar 14, 2013
Acta Derm Venereol 2013; 93: XX–XX.
Tomoyasu Hattori, Department of Dermatology, Gunma University Graduate School of Medicine, 3-39-22, Showa-machi, Maebashi, Gunma 371-8511, Japan. E-mail: tohatt@gunma-u.ac.jp
Mycosis fungoides (MF), the most common type of cutaneous T-cell lymphoma (CTCL), is clinically characterized by a slow progression from patches to plaques, and to tumours in the majority of patients. Histologically, the disease is typified by the proliferation of small cerebriform lymphocytes showing epidermotropism. While MF has a plethora of clinicopathological manifestations (1), MF presenting as a haematoma-like lesion is rare (2). We report here a case of a rapidly progressive, fatal MF with a haematoma-like appearance associated with CD30+ large-cell transformation.
CASE REPORT
A 78-year-old Japanese woman was referred to our hospital with a one-week history of a rapidly enlarging, haematoma-like mass on the back of the right thigh. Physical examination revealed an indurated, focally ulcerated, dome-shaped, purplish skin mass approximately 20 cm in diameter on the posterior aspect of the right thigh (Fig. 1A). Multiple reddish-brown erythematous lesions without palpable infiltration were also observed on the trunk and extremities; the time of onset of these lesions was unknown (Fig. 1B). The patient also had right inguinal lymphadenopathy and a subcutaneous left breast mass. Computed tomography revealed an enhanced subcutaneous mass in the right thigh, and multiple enhanced subcutaneous nodules in the extremities, left buttock, right inguinal area and left breast. Based on the above findings, she was diagnosed with cutaneous lymphoma with a traumatic haematoma. However, an incision of the haematoma-like mass revealed neither coagulated clots nor bleeding. Laboratory examination revealed pancytopaenia (white blood cell 3,800/μl, red blood cell 2.95 × 106/μl, haemoglobin 10.3 g/dl, platelet 122 × 103/μl) and elevated values for fibrin/fibrinogen degradation products (FDP) (10.1 μg/ml), D-dimer (5.7 μg/ml), erythrocyte sedimentation rate (16 mm/h), ferritin (1,372.2 ng/ml) and C-reactive protein (1.50 mg/dl). Disseminated intravascular coagulation was considered unlikely. The serum level of soluble interleukin-2 receptor was extremely high (5,658, normal range 135–483 U/ml). Human T-cell lymphotropic virus type I (HTLV-I) serology was negative. Core needle biopsy of the breast revealed a diffuse infiltration of atypical lymphocytes expressing CD3, but not CD20 and CD79α in the mammary gland and surrounding subcutaneous tissue. Biopsy of the lymph node was not performed, and bone marrow biopsy showed no abnormality.
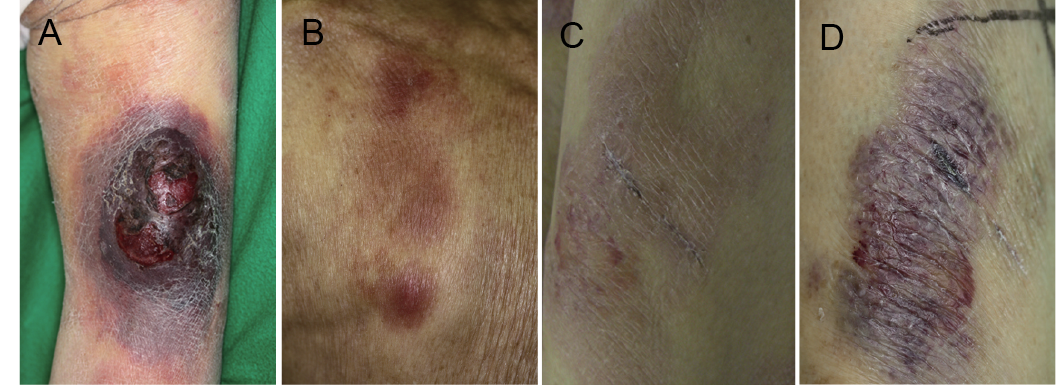
Fig. 1. (A) A haematoma-like mass on the posterior aspect of the right thigh. (B) Reddish-brown, non-indurated erythema on the trunk. (C) The non-infiltrated erythema on the left thigh evolved into (D) a violaceous nodule over a period of 2 weeks. A biopsy scar is visible in the centre of the lesion.
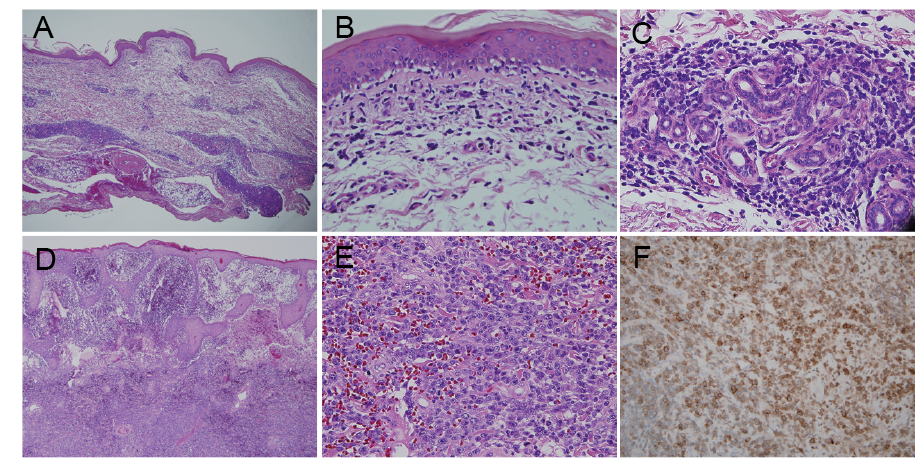
Histopathological examination of a biopsy specimen from an erythematous lesion on the left lower leg demonstrated a band-like infiltration of atypical lymphocytes with enlarged, hyperchromatic nuclei and irregular nuclear contours in the upper dermis (Fig. 2A and B). Significant epidermotropism was noted in the epidermis (Fig. 2B). Atypical lymphocytes also infiltrated densely around the eccrine glands and ducts in the reticular dermis; however, neither hyperplastic eccrine glands nor follicular involvement was present (Fig. 2A and C). A phenotypic analysis of the infiltrate revealed a predominance of CD3+ and CD4+ T cells, while CD5, CD8 and CD20 were negative. Monoclonal rearrangement of T-cell receptor Cβ gene was detected. Biopsy specimens taken from the haematoma-like lesion revealed diffuse and dense infiltrates of medium-to-large-sized pleomorphic lymphocytic cells in the epidermis, dermis and subcutaneous fat (Fig. 2D and E) admixed with red blood cells. Infiltrating lymphocytes were positive for CD3, CD30 (Fig. 2F) and MIB-1, partially positive for CD4, and negative for CD5, CD8 and CD20. Based on these findings, the patient was diagnosed with MF (tumour node metastasis blood staging: T3, Nx, M0) with CD30+ large-cell transformation. Multiple erythematous lesions evolved into violaceous plaques or nodules within a short period (Fig. 1C and D). Although local radiation therapy was started to treat the haematoma-like lesion on the thigh, it was ceased after the first session due to the patient’s poor general condition. The patient developed disseminated intravascular coagulation and died approximately 4 weeks after admission.
Fig. 2. (A) Haematoxylin-eosin staining of a biopsy specimen taken from an erythematous lesion on the left lower leg. Microscopically, a band-like lymphocytic infiltration in the upper dermis and a dense infiltration around the eccrine glands and ducts in the reticular dermis were observed on low magnification. (B) An infiltration of atypical lymphocytes with cerebriform nuclei in the epidermis and (C) around the eccrine gland without syringometaplasia was seen on high magnification. (D) Haematoxylin-eosin staining of a biopsy specimen taken from the mass on the right thigh showed diffuse and dense infiltrates with subepidermal blistering. (E) Medium-to-large-sized pleomorphic lymphocytic cells mixed with numerous red blood cells were observed on high magnification. (F) Immunohistochemical staining showed that the large atypical cells were positive for CD30. (Original magnification: A and D ×40; B, C and E ×400; and F ×200).
DISCUSSION
MF lesions in the tumour stage are usually dome-shaped, elastic and dark-red in colour. To the best of our knowledge, only one case of CTCL associated with trauma-related haematoma has been reported; the tumour was discovered after the patient presented with a haematoma of the right shin and a biopsy showed a dense infiltration of atypical cells expressing CD45RO but not CD30 in the dermis and subcutaneous tissue with prominent epidermotropism (2). Although the mechanism is unclear, the authors speculated that trauma may influence the growth of a pre-existing neoplasm (2). In our case, a history of preceding trauma was unclear, and erythematous lesions evolved into violaceous plaques or nodules without preceding trauma. Tissue destruction by the heavy infiltrate of atypical cells may have resulted in bleeding within the lesions. For example, certain neoplastic cells may release cytokines or cytotoxic proteins, such as granzyme and T-cell-restricted intracellular antigen, which affect bleeding (3–5).
In the above-mentioned report of MF associated with trauma-related haematoma, the lymphoma had an aggressive clinical course (approximately 6 months from diagnosis to death) and was regarded as d’emblée form of MF (2). The d’emblée form of MF is characterized by rapidly enlarging tumours not preceded by classic patch- and plaque-stage disease. However, d’emblée is now regarded as a clinical descriptive term and not as a subtype in the modern classification of primary cutaneous lymphomas (1, 6, 7). We believe that our case may have been d’emblée form of MF.
A peculiar presentation of MF may be indicative of a more aggressive variant of MF. Some atypical forms of MF, such as folliculotropic MF, bullous MF and granulomatous MF, have been reported to show more aggressive behaviour than classical MF (8–12). In our case, the haematoma-like mass was associated with CD30+ large-cell transformation. Transformation has been defined as the presence of large cells exceeding 25% of the total lymphoid infiltrate or forming microscopic nodules (13). Whereas transformation is associated with a more aggressive biological behaviour and course (13–17), some studies demonstrated that not all patients with transformed MF run an aggressive clinical course (18, 19). Benner et al. (18) recently demonstrated that factors including CD30 negativity, folliculotropic MF and the extent of skin involvement at the time of large-cell transformation were associated with reduced disease-specific survival. Several studies also suggest that CD30 expression in transformed MF might be associated with a better prognosis (14, 15, 17). Therefore, it remains to be determined whether CD30+ large-cell transformation in MF is associated with an aggressive disease course.
“Syringotropic MF”, a rare variant of MF with a prognosis similar to classic MF, is characterized by hyperplastic eccrine glands and eccrine ducts surrounded by a dense infiltrate of atypical lymphocytes with cerebriform nuclei (1, 20–22). Folliculotropic MF is considered to be a closely related condition, as some cases of syringotropic MF demonstrate lymphocytic infiltration involving both eccrine glands and hair follicles (23, 24). On the other hand, lymphoid infiltrates around the eccrine glands without syringometaplasia can be observed in biopsies of conventional MF usually in the tumour stage (22, 25, 26). Previous studies reported that a prominent eccrine infiltration was noted in approximately 30% of biopsy specimens from indisputable cases of MF (25, 26), indicating the syringotropic behaviour of MF. Although syringotropism of atypical T lymphocytes was quite prominent even in the non-infiltrative erythematous lesion, the present case is unlikely to be syringotropic MF because neither syringometaplasia nor follicular involvement was present.
In summary, we described a case of a rapidly progressive MF with peculiar clinical appearance and histological features. The relationship between syringotropism of atypical T lymphocytes and CD30+ large-cell transformation with the haematoma-like appearance is unknown. Doctors should be aware of unusual presentations of MF; we speculate that an unusual haematoma-like appearance of MF may be associated with a poor prognosis.
The authors declare no conflicts of interest.
REFERENCES
