Ru-Lan Hsieh, MD1,2 and Wen-Chung Lee, MD, PhD3
From the 1Department of Physical Medicine and Rehabilitation, Shin Kong Wu Ho-Su Memorial Hospital, 2School of Medicine, College of Medicine, Taipei Medical University and 3Institute of Epidemiology and Preventive Medicine, College of Public Health, National Taiwan University, Taipei, Taiwan
OBJECTIVE: To investigate the immediate and medium-term effects of custom-moulded insoles on patients with knee osteoarthritis.
DESIGN: Before-after trial, followed up for 6 months.
SUBJECTS: Forty participants, mean age 61 years, who fulfilled the combined radiographic and clinical criteria for knee osteoarthritis, as defined by the American College of Rheumatology.
METHODS: Custom-moulded insoles with a 5º lateral wedge and arch support were prescribed. Immediate assessment was performed with and without the custom-moulded insoles, and follow-up assessments on pain, balance control, physical function, and physical activity were performed at 1, 3, and 6 months.
RESULTS: Significant medium-term effects were represented by reductions in pain (p = 0.003), improved physical functioning (p = 0.006), and decreased chair-rising time (p = 0.016) over the duration of the 6-month follow-up period. Significant immediate increases in physical activity scores for the 10-m normal-speed walking test (p = 0.007), stair-climbing test (p = 0.040), and chair-rising test (p = 0.030) were also observed in patients wearing the custom-moulded insoles, compared with tests performed without the insoles.
CONCLUSION: Using custom-moulded insoles provides medium-term pain reduction and improved physical functioning and physical activity, as well as immediate beneficial effects regarding physical activity.
Key words: insole; knee osteoarthritis; pain; physical function; balance.
J Rehabil Med 2014; 46: 00–00
Correspondence address: Ru-Lan Hsieh, Department of Physical Medicine and Rehabilitation, Shin-Kong Wu Ho-Su Memorial Hospital, 95 Wen-Chung Rd, Shih-Lin District, Taipei 111-01, Taiwan. E-mail: M001052@ms.skh.org.tw
Accepted Sep 3, 2013; Epub ahead of print Nov 13, 2013
INTRODUCTION
Knee osteoarthritis (OA) is usually associated with pain, stiffness, poor proprioception, periarticular muscle atrophy, restricted movement, and decreased physical activity (1). In our previous study, patients with knee OA were found to have lower postural stability and health-related quality of life (HRQOL) than age-matched controls (2). The goal of treatment for knee OA is to control pain, improve physical function, and increase HRQOL, while optimally avoiding aversions to therapy (3).
It has been estimated that 60–80% of the weight of the body is distributed to the medial compartment of the knee during the midstance phase during normal gait (4). Patients with knee OA were reported to display greater external knee adduction moment during walking than age-matched controls (5). In addition, positive relationships were observed between the adduction moment and the levels of knee pain and radiographic severity (6). Therefore, non-surgical approaches, such as wearing orthopaedic shoe insoles and knee braces, are often used to reverse the negative effects of biomechanical factors on the progression of knee OA (7).
Foot insoles have commonly been used to reduce pain and increase physical functioning in patients with knee OA (8). Yasuda & Sasaki (4) have reported that lateral-wedge insoles changed the relative spatial positions of the calcaneus, tibia, and femur, and reduced the medial knee-joint-space load. A biomechanical study showed that using lateral-wedge insoles reduced adduction moment and varus malalignment (9). Nevertheless, Kakihana et al. (10) reported that the biomechanical effects of lateral-wedged insoles were inconsistent, with some participants exhibiting increased knee adduction moment. People with medial compartment knee OA are associated with a higher incidence of pronated foot than are controls (11–13). The ankle and foot complex is multifunctional (11). Pronation occurs when the subtalar joint rotates in a closed kinetic chain, leading to loose foot joints and a flat medial arch with poor shock absorption (11). Re-supination occurs when the weight-bearing limb rotates externally as the body weight passes over the foot, and the contralateral limb moves forward (14). Re-supination allows the foot to be a lever for propulsion (15). The transition from supination to pronation and back to supination occurs concurrently in the closed kinetic chain of the ankle (11). If the patient has a pronated foot, a lateral-wedge insole might further increase pronation, and lead to further deviation from a normal gait (13). Some studies have shown that the use of lateral-wedged insoles can improve pain and knee adduction moment in patients with knee OA (16, 17). However, a randomized control trial (18) and a systemic review (19) have shown that using lateral-wedged insoles did not result in a superior outcome. Therefore, the therapeutic effects of lateral-wedge insoles for knee OA remain unclear (8, 16–20).
Insoles with arch support are widely prescribed based on their enhancing effects on support, stability, shock absorption, and maintenance of proper foot position during walking and running (21). In sports medicine, a pronated foot is usually treated with medial-wedge orthotics (22). Adding arch support to lateral-wedge insoles can maintain the normal motion of the rear foot and reduce the knee adduction moment, enabling patients with knee OA to walk more naturally (23). Arch support can enhance the biomechanical effect by increasing walking speed and progression angle, and reducing valgus angle at the subtalar joint and external knee adduction moment in patients with knee OA (17).
Previous studies on the effects of insoles on knee OA have primarily used non-custom-moulded insoles. Hence, the therapeutic effects of custom-moulded insoles on knee OA have not been thoroughly studied. The biomechanical effects of lateral-wedged insoles may be influenced by the particular characteristics of the feet of different individuals (12). Therefore, customization could reduce the risk of overpronating when using lateral-wedge insoles (12). One study suggested that full-length lateral-wedge insoles, rather than rear-foot wedges, can reduce the external knee adduction moment and may optimize the potential benefits in patients with medial knee OA (24). The objective of our study was therefore to evaluate the immediate and medium-term therapeutic effects of using lateral-wedge custom-moulded total-contact insoles with longitudinal arch support on pain, balance control, physical activity, and physical functioning in patients with knee OA. However, larger-angled wedges may cause greater foot and ankle discomfort (9). Therefore, for our study, we selected a 5º lateral-wedge insole. We hypothesized that: (i) using lateral-wedged custom-moulded total-contact insoles with arch support increases both the immediate and medium-term assessment scores for physical activity and balance control; and that (ii) the medium-term use of custom-moulded insoles reduces pain and improves physical function in patients with knee OA.
METHODS
Participant selection
The study was approved by the Institutional Review Board for the Protection of Human Subjects at Shin Kong Wu Ho-Su Memorial Hospital, Taipei, Taiwan. Written informed consent was obtained from each participant. Participants were recruited from the clinic of the Department of Physical Medicine and Rehabilitation at Shin Kong Wu Ho-Su Memorial Hospital during 2011, and all subjects were followed for 6 months. Inclusion criteria were: participants fulfilled the combined clinical and radiographic criteria for knee OA, as established by the American College of Rheumatology; Kellgren-Lawrence scores of 2 or higher for the isolated medial compartment based on anteroposterior radiographic views of both knees while weight-bearing; age range 40–80 years. Exclusion criteria were: a history of previous knee surgery involving an implant, a reduced lateral compartment, or combined medial and lateral compartments in the knee joints; pregnant or planning to become pregnant; a self-reported history of vertigo, malignancy, stroke, or other conditions that might impair vestibular function.
Basic demographic evaluation
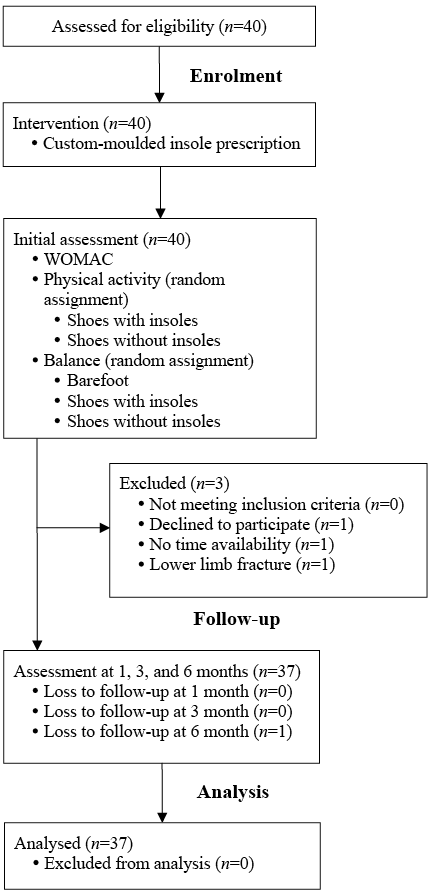
General demographic data regarding age, sex, educational level, marital status, and employment status were collected. Data regarding smoking, alcohol use, hypnotics or sedative use, fall history in the 6 months preceding the study, and comorbidities were also collected. Body weight and height were recorded, and the body mass index (BMI) of each participant was calculated (Fig. 1).
Fig. 1. Trial profile. WOMAC: Western Ontario and McMaster University Osteoarthritis Index.
Foot posture evaluation
The foot posture of each participant was tested using the Foot Posture Index (FPI) (25). The participants were asked to stand in a relaxed position with double-limb support, their arms by their sides, and looking straight ahead. The FPI is used to rate weight-bearing foot posture according to a composite score of clinical observational criteria: talar head palpation, curve above and below the lateral malleolus, inversion/eversion of the calcaneus, prominence in the talonavicular joint region, congruence of medial longitudinal arch, and abduction/adduction of the forefoot on the rearfoot. Each score for these criteria ranges from –2 to +2, and the scores of all components are added to yield a final score. Foot posture can be classified as follows: normal (0 to +5), pronated (+6 to +9), highly pronated (+10 to +12), supinated (–1 to –4), and highly supinated (–5 to –12). The index demonstrated a high level of intra-rater reliability (12).
Treatments
After the demographic and health-related data were collected, participants were prescribed a pair of bilateral custom-moulded insoles. The insoles were made of 100% high-density ethyl vinyl acetate with a closed-cell construction, which prevented compression of the insoles and prolonged the support function. A full-length 5º wedge along the posterior-lateral border, which tapered down towards the metatarsal heads with longitudinal arch support, was incorporated into the structure of the insole (Fig. 2). After heating for 40 s with a heat gun with timing gates measurement, the thermoplastic insoles were individually moulded according to a static pedometer evaluation by a qualified physiatrist to maintain the subtalar joint in a neutral standing position, thus preventing supination or pronation of the foot. The neutral position of the subtalar joint was maintained by hand to fix the foot position relative to the talar head, maintaining equal prominence both medially and laterally during the insole modification process (12). Additional pads were added to the insoles to correct leg-length discrepancy or forefoot valgus deformity, if indicated. Participants were initially instructed to use the insoles for 1 h, thereafter increasing usage for an additional 1 h per day until full-time use was achieved. Participants who experienced discomfort returned to the clinic for insole remoulding during the following 1–2 weeks. The insoles were also evaluated at each follow-up examination for remoulding in case of degradation.

Fig. 2. Insoles with a 5º lateral wedge and longitudinal arch support.
Outcome measures
Physical activity. Physical activity was assessed based on the time results of a 10-m fast-speed walking test, a 10-m normal-speed walking test, a stair-climbing test, and a chair-rising test. The 10-m fast-speed walking test and 10-m normal-speed walking test were measured as participants walked across a hard, flat surface. The stair-climbing test was measured as the time required for participants to ascend a flight of stairs (14 steps, 18 cm each) as quickly as possible. The chair-rising time was measured as the time required for the participants to rise 5 times from a seated position in a standard chair to a standing position as quickly as possible without using their arms for support. Longer times to complete the tests represented greater limitations of physical activity.
Balance control. The Biodex Stability System is used to assess balance control by measuring changes in body weight distribution while standing in a fixed position on a movable platform at various degrees of tilt. Postural stability was measured by moving the platform along both the anterior-posterior and medial-lateral axes. Higher scores on the anterior-posterior, medial-lateral, and overall stability indices indicated greater postural variability and less stability (26). To test the dynamic limits of stability, the participants moved a cursor on the monitor screen from the centre of the screen to different peripheral boxes that appeared in random order by shifting their body weight on a platform, and the movement of the cursor was synchronized with the movement of the platform. Higher scores indicated higher levels of dynamic balance control. Fall risk was assessed at different speed levels with resistance. Higher scores indicated a greater risk of falling, compared with age- and gender-matched control patients. The system has good inter-rater and intra-rater reliabilities (27). We used the most stable resistance level (Level 8) to measure balance control. The participants were instructed to maintain a bipedal stance with their eyes open. The foot position of each participant was recorded to ensure that the same stance was maintained throughout all the test sessions. All participants were allowed one practice attempt, followed by one formal test for each measurement.
Knee osteoarthritis-related health status. Self-reported measures of knee OA-related health status were assessed using the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) (28). Using a visual analogue scale, total WOMAC scores for pain, stiffness, and level of physical functioning from 0 to 500, 0 to 200, and 0 to 1,700, respectively, were collected from each participant. Higher scores represented more severe symptoms and greater functional limitations. The reliability and validity of the 3 visual analogue scale assessments were reported elsewhere (29).
Immediate effect. An investigator blinded to the insole-wearing status of the participants evaluated their physical activity and balance control to assess the immediate insole treatment effects at the time of intervention (immediate assessment).To test physical activity, participants were randomly assigned to 2 conditions (wearing shoes without custom-moulded insoles or wearing shoes with custom-moulded insoles). To test balance control (including postural stability, dynamic limits of stability, and risk of falling), they were assigned to 3 conditions (barefoot, wearing shoes without custom-moulded insoles, or wearing shoes with custom-moulded insoles). Condition assignment was performed using block randomization with a block size of 4 and computer-generated random numbers. Participants were randomly assigned to the different conditions by drawing a sealed envelope. The insole modification and test procedures were all performed on Wednesday afternoons for 2 participants each week. The tests for physical activity and balance control were approximately 30 min per participant.
Medium-term effects. The medium-term effects of wearing shoes with the custom-moulded insoles were assessed according to the WOMAC, physical activity, and balance control at 1-, 3-, and 6-months follow-up.
Primary and secondary outcome measures
The primary outcome measure was the pain subscale score of the WOMAC. The secondary outcome measures were the physical function subscale of the WOMAC assessment and the physical activity tests.
Sample size
Based on previous reports of the estimates of variability in WOMAC pain scores and the range of minimal percentile clinical improvement for WOMAC (9–12 on a scale of 100) (17, 23), we determined that a sample size of 22–39 participants was needed to conduct a test of repeated-measures (analysis of covariance ANCOVA) with a statistical significance level of 0.05 and a power of 0.8 for our WOMAC analysis (pain score 0–500). Considering the possibility of participant withdrawal during follow-up, we initially selected 40 participants.
Statistical methods
The paired t-test was used to assess the immediate treatment effects on physical activity and balance control. A repeated-measures ANCOVA was used to assess the 3 domains of the WOMAC, physical activity, and balance control in the immediate and follow-up assessments using the baseline measurements as the covariates. The results of ANCOVA were expressed as the F statistic, degrees of freedom, and p-value. Intention-to-treat analysis (last observation carried forward) was initially performed for all participants.
RESULTS
A total of 40 subjects were consecutively enrolled in the study; 35 women and 5 men, age range 40–79 years, mean age 61 years. The subjects’ demographics, smoking and alcohol use, and comorbidity data of the participants are shown in Table I. The mean Kellgren-Lawrence score was 2.6 (standard deviation (SD) 0.5). Three participants withdrew after the initial evaluation. One participant withdrew from the study for unstated reasons, another withdrew because of limited personal time, and another withdrew because of a lower limb fracture from a traffic accident. One participant refused the follow-up examination at 6 months because of pain aggravation. The drop-out rate was 10%. At 6 months of follow-up, 33 participants (82.5%) wore the insoles while performing outdoor activities, and the mean wearing comfort score (from 0 to 10) was 9.0 (SD 1.41). No degradation of insoles occurred and no replacement of insoles was necessary during the follow-up period.
|
Table I. Basic demographics of the study subjects |
|
|
Variables |
|
|
Age, years, mean (SD) |
61.0 (9.9) |
|
Sex, n (%) |
|
|
Female |
35 (87.5) |
|
Male |
5 (12.5) |
|
BMI, kg/m2, mean (SD) |
25.0 (4.7) |
|
Married, yes, n (%) |
34 (85.0) |
|
Educational level, n (%) |
|
|
Below ninth grade |
15 (37.5) |
|
Above ninth grade |
25 (62.5) |
|
Working status, yes, n (%) |
17 (42.5) |
|
Comorbidities, yes, n (%) |
27 (67.5) |
|
Smoking, yes, n (%) |
1 (2.5) |
|
Drinking, yes, n (%) |
5 (12.5) |
|
Hypnotics or sedatives, yes, n (%) |
7 (17.5) |
|
Fall history in the previous 6 months, yes, n (%) |
6 (15) |
|
Foot Posture Index, n (%) |
|
|
Normal (0 to +5) |
7 (17.5) |
|
Pronated (+6 to +9) |
33 (82.5) |
|
Kellgren-Lawrence scores, mean (SD) |
2.6 (0.5) |
|
BMI: body mass index; SD: standard deviation. |
|
Repeated-measures ANCOVA showed a significant time effect for pain (p = 0.003) and physical function (p = 0.006) for the duration of the follow-up period based on the WOMAC assessment (Table II). No significant time effects were found for the stiffness, 10-m normal-speed walking, or stair-climbing assessments (Table II). Statistically significant shorter times were recorded for the immediate assessments of the 10-m normal-speed walking test (11.2 (SD 2.6) vs 12.2 (SD 3.1); p = 0.007), the stair-climbing test (12.9 (SD 6.3) vs 14.8 (SD 8.5); p = 0.040), and the chair-rising test (17.8 (SD 5.5) vs 19.7 (SD 7.4); p = 0.030) for patients using the custom-moulded insoles than were recorded for patients who did not wear the insoles (Table III). However, repeated-measures ANCOVA revealed that only the chair-rising time showed significant medium-term improvement over the baseline physical activity assessments of patients using the custom-moulded insoles (p = 0.016; Table III). No significant immediate or medium-term differences were observed for the 10-m fast-speed walking test or the balance control evaluations (Tables II–III).
|
Table II. Medium-term effects of insole wearing on pain, physical functioning, physical activity, and balance control |
|||||
|
Variables |
Initial (n = 40) Mean (SD) |
1 month (n = 37) Mean (SD) |
3 months (n = 37) Mean (SD) |
6 months (n = 36) Mean (SD) |
p-value |
|
WOMAC |
|||||
|
Pain |
217.9 (125.4) |
164.4 (118.8) |
133.5 (86.2) |
100.0 (74.8) |
0.003 (F(2,68) = 6.42) *** |
|
Stiffness |
74.7 (56.6) |
51.8 (45.9) |
45.8 (45.3) |
48.8 (42.9) |
0.465 (F(2,68) = 0.77) |
|
Physical function |
656.3 (380.1) |
538.1 (344.5) |
475.5 (314.5) |
402.3 (279.1) |
0.006 (F(2,68) = 5.51) ** |
|
Physical activity |
|||||
|
10-m normal-speed walking time |
11.2 (2.6) |
10.6 (2.6) |
10.0 (2.1) |
10.2 (2.1) |
0.115 (F(2,67) = 2.24) |
|
10-m fast-speed walking time |
9.1 (1.9) |
8.7 (2.1) |
8.4 (2.0) |
8.4 (1.9) |
0.177 (F(2,67) = 1.78) |
|
Stair-climbing time |
12.9 (6.3) |
12.2 (4.9) |
12.6 (6.8) |
12.3 (6.8) |
0.949 (F(2,67) = 0.05) |
|
Chair-rising time |
17.8 (5.5) |
17.5 (7.0) |
15.9 (4.8) |
16.4 (6.3) |
0.016 (F(2,67) = 4.39) * |
|
Balance |
|||||
|
Postural stability |
|||||
|
Anterior/Posterior Index |
0.6 (0.7) |
0.6 (0.4) |
0.6 (0.4) |
0.6 (0.5) |
0.979 (F(2,67) = 0.02) |
|
Medical/Lateral Index |
0.4 (0.4) |
0.4 (0.2) |
0.3 (0.3) |
0.4 (0.4) |
0.230 (F(2,67) = 1.50) |
|
Overall Stability Index |
0.9 (0.8) |
0.8 (0.5) |
0.8 (0.5) |
0.8 (0.6) |
0.818 (F(2,67) = 0.20) |
|
Limits of stability |
38.9 (16.8) |
43.8 (14.2) |
47.5 (15.6) |
44.6 (13.8) |
0.354 (F(2,67) = 1.05) |
|
Fall risk |
2.2 (1.8) |
1.6 (1.6) |
1.7 (1.3) |
1.4 (1.0) |
0.529 (F(2,67) = 0.64) |
|
*p < 0.05, **p < 0.01, ***p < 0.005. SD: standard deviation; WOMAC: Western Ontario and McMaster University Osteoarthritis Index. |
|||||
|
Table III. Immediate effects of insole wearing on physical activity and balance |
||||
|
Variables |
Barefoot (n = 40) Mean (SD) |
Shoes without custom-moulded insoles (n = 40) Mean (SD) |
Shoes with custom-moulded insoles (n = 40) Mean (SD) |
p-value |
|
Physical activity |
||||
|
10-m normal-speed walking time |
Not tested |
12.2 (3.1) |
11.2 (2.6) |
0.007** |
|
10-m fast-speed walking time |
Not tested |
9.3 (2.1) |
9.1 (1.9) |
0.367 |
|
Stair-climbing time |
Not tested |
14.8 (8.5) |
12.9 (6.3) |
0.040* |
|
Chair-rising time |
Not tested |
19.7 (7.4) |
17.8 (5.5) |
0.030* |
|
Balance |
||||
|
Postural stability |
||||
|
Anterior/Posterior Index |
0.8 (0.8) |
0.9 (1.2) |
0.6 (0.7) |
0.252 |
|
Medical/Lateral Index |
0.6 (0.6) |
0.5 (0.5) |
0.4 (0.4) |
0.168 |
|
Overall Stability Index |
1.2 (1.0) |
1.1 (1.0) |
0.9 (0.8) |
0.150 |
|
Limits of stability |
39.7 (12.6) |
40.7 (13.7) |
38.9 (16.8) |
0.709 |
|
Fall risk |
2.5 (2.0) |
2.4 (1.9) |
2.2 (1.8) |
0.750 |
|
*p < 0.05, **p < 0.01. SD: standard deviation. |
||||
We also analysed the cigarette smoking, alcohol use, comorbidity, and foot posture (either normal or pronated) data of participants, which could affect the results. In addition, the present study did not exclude participants who were using hypnotics or sedatives, or those with a history of falling in the 6 months preceding the study. The results showed that neither of these factors confounded the results.
DISCUSSION
Based on our thorough review of relevant literature, this is the first study that evaluated the immediate and medium-term therapeutic effects of lateral-wedge custom-moulded insoles with arch support and foot alignment correction for maintaining a neutral subtalar joint position in patients with knee OA. Using the custom-moulded insoles resulted in significant reduction in medium-term pain, improvement in physical functioning, and time reduction in the chair-rising tests. Our results also showed that, although there were no immediate effects on balance control, a significant immediate improvement in physical activity occurred when using the custom-moulded insoles, which is represented by the shorter times recorded for the 10-m normal-speed walking, stair-climbing, and chair-rising tests.
Pain and decreased physical activity may interfere with the daily-life activities of patients with knee OA (30), thereby increasing their disability and economic burden (31). Therefore, determining methods to reduce pain and improve physical function is a crucial task. Thus, the medium-term improvements in pain management and physical activity achieved using our custom-moulded insoles are encouraging. Wedge insoles can realign the foot 5–10º in either the varus or valgus plane (32), and may change the spatial positions of the lower limb through muscle activation and changes in the position of the trunk (4). The angle of the lateral wedge is related to the unloading force exerted on the knee (9, 33). A 1-mm lateral displacement of the centre of pressure is known to reduce the peak knee adduction moment by 2%, resulting in a 1% reduction of the peak force acting in the medial compartment (34).
Lateral-wedge insoles can reduce foot supination and accentuate foot pronation in a balanced foot and ankle during gait (35). Therefore, lateral-wedge insoles may aggravate the pronation of an over-pronated ankle and foot (35). In addition, wedges may inhibit normal foot and ankle biomechanics, aggravating OA symptoms (36). Deformities of the ankle, midfoot, or hindfoot may lead to lower limb malalignment and aggravate knee OA symptoms (32). To prevent over-pronation or supination of the foot, as well as possible exaggeration of the compression load on the medial knee compartment (7), we maintained the subtalar joint in a neutral position by adjusting the height of the arch support and/or using additional pads under the insoles. Although the present study showed that the foot position did not influence the effects of wearing insoles, the feet of most patients (82.5%) in our study were in a pronated position. Additional studies, focused on the effects of insoles on different foot positions, such as normal, pronated, or supinated, should be performed in the future.
Adaptive insoles with a well-padded longitudinal arch support may improve foot alignment and shock attenuation during walking and running (32). Although no significant changes in the peak knee varus torque have been reported for an early stance during walking, greater torque has been observed for a late stance during walking and running in young people using arch supports (21). Lateral-wedge insoles with arch support enabled healthy volunteers to walk in a more natural manner because the insoles efficiently reduced the knee adduction moment (17). It has been shown that lateral-wedged insoles with arch support significantly increased walking speed and reduced the early stance external knee adduction moment and the knee adduction angular impulse in patients with knee OA (23). These biomechanical effects may redistribute the load from the medial compartment to the lateral compartment of the knee joint and reduce pain in patients with knee OA. The use of custom-moulded insoles with a 5º lateral wedge and longitudinal arch support in participants with knee OA was a novel aspect of our study. The relationship between the mechanical loading effects and pain in knee OA is complex (23). However, we did not evaluate the biomechanical changes that may have occurred during standing and walking when using our custom-moulded insoles. Therefore, the relationship between the biomechanical effects of the custom-moulded lateral-wedge insoles with arch support and pain in patients with knee OA warrants further investigation.
Discomfort is a crucial factor that may affect adherence to a treatment, and adherence is likely to have a substantial effect on the outcome of a treatment. Several previous studies, with a randomized controlled trial or non-randomized controlled trial, have reported substantial variance (57–88%) regarding adherence to insole wearing (16). Previous studies have reported different distributions of discomfort, ranging from 0% to 47%, in participants using 5º lateral-wedge insoles (9, 18). The treatment adherence of the present study was 82.5%, and the participants experienced high comfort using the custom-moulded insoles. This result is consistent with that of a previous study, which reported that the use of modified insoles could reduce discomfort and enhance clinical results (37).
Previous studies have shown no short-term (1–3 months) degradation of wedge insoles (38). Although typically made of high-density materials, insoles may compress over time, causing a reduction in the angle of the wedge and the arch support, which renders them less effective than when new (38). Therefore, we checked the insoles in our study at each of the follow-up examinations and remoulded them when necessary. A few cases required remodelling of the insoles because of discomfort. No insoles were replaced because of degradation in the present study. Compared with using non-custom-moulded insoles, treatments using custom-moulded insoles are more expensive, more time-consuming, and require special techniques and knowledge for the moulding and adjustment processes. However, the medium-term therapeutic effects on pain, physical activity, and physical functioning justify the cost of custom-moulded insole treatments, and represent a relatively simple alternative to more expensive and complex interventions, such as knee replacement surgery (3).
Insoles can affect muscle forces across the hip, knee, and ankle joints (39). Long-term use of lateral-wedge insoles can lead to reduced adduction moments during walking through gait adaptations (40). Thus, using lateral-wedge insoles may reduce pain in the lower limbs and improve balance (39). However, our study showed that custom-moulded insoles had no immediate or medium-term effects on balance control. We did not assess the vestibular, visual, or proprioceptive abilities of the participants. Furthermore, we did not exclude participants who were using hypnotics or sedatives, or those with a history of falling, all of which may be associated with diminished balance control. Factors including cigarette smoking, alcohol use, comorbidities, hypnotics or sedative use, and a history of falling in the 6 months preceding the study did not confound the effects of insole wearing in patients with knee OA. In addition, the non-significant changes in balance control could have been produced by the ceiling effect, or the tests may not have been adequately sensitive to evaluate the actual changes in patients with knee OA. Therefore, additional studies that control for additional factors that may affect balance control are required.
This study has some limitations. First, we did not assess the biomechanical effects of the custom-moulded insoles. Secondly, although the immediate effects of the custom-moulded insoles on improving physical activity were demonstrated under different conditions, we did not use a randomized, double-blind, placebo-controlled design for medium-term follow-up. Additional double-blind, randomized, placebo-controlled, long-term follow-up studies comparing the different types of insoles (i.e. custom-moulded insoles with lateral-wedge and arch support vs lateral-wedge insoles without arch support, and custom-moulded insoles vs non-custom-moulded insoles) are warranted. Thirdly, multiple comparisons (12 outcome measures), the selection of consecutive patients (35 women and only 5 men were included in this study), and lack of long-term follow up (results may change at a 1-year follow-up) could affect the generalizability of this study. Fourthly, although our study found that the medium-term improvement in the WOMAC pain score exceeded the 50-point minimal percentile improvement (500 maximum) (23, 28), we cannot exclude natural recovery from pain or natural causes for the observed improvements in physical functioning and level of physical activity in these participants.
In conclusion, wearing custom-moulded insoles with a 5º lateral wedge and arch support provided medium-term pain reduction, as well as improvement in physical functioning and physical activity in patients with knee OA. Patients with knee OA who used custom-moulded insoles exhibited higher physical activity scores than did those not using the insoles. Additional randomized, controlled clinical studies are necessary to determine the long-term effectiveness of the custom-moulded insoles for patients with knee OA.
ACKNOWLEDGEMENTS
This study was supported by research grants from the Shin Kong Wu Ho-Su Memorial Hospital (SKH-8302-100-DR-21; SKH-8302-102-DR-32) and the Taiwan National Science Council (NSC 102-2628-B-002-036-MY3; NSC 102-2314-B-341-001).
The authors declare no conflicts of interest.
REFERENCES
