Birgit Prodinger, PhD1,2*, Carolina S. Ballert, MSc, Dpl.Stat.1,2*, Martin W. G. Brinkhof, PhD1,2, Alan Tennant, PhD1,2 and Marcel W. M. Post, PhD1,3,4
From the 1Swiss Paraplegic Research (SPF), Nottwil, 2Department of Health Sciences and Health Policy, University of Lucerne, Lucerne, Switzerland, 3Department of Rehabilitation Medicine, Center for Rehabilitation, University of Groningen, University Medical Center Groningen, Groningen and 4Brain Center Rudolf Magnus and Center of Excellence in Rehabilitation Medicine, University Medical Center Utrecht and De Hoogstraat, Utrecht, The Netherlands. *Both of these authors have contributed equally.
OBJECTIVE: The Spinal Cord Independence Measure – Self Report (SCIM-SR) is a self-report instrument for assessing functional independence of persons with spinal cord injury. This study examined the internal construct validity and reliability of the SCIM-SR, when administered in a community survey, using the Rasch measurement model.
METHODS: Rasch analysis of data from 1,549 individuals with spinal cord injury who completed the SCIM-SR.
RESULTS: In the initial analysis no fit to the Rasch model was achieved. Items were grouped into testlets to accommodate the substantial local dependency. Due to the differential item functioning for lesion level and degree, spinal cord injury-specific sub-group analyses were conducted. Fit to the Rasch model was then achieved for individuals with tetraplegia and complete paraplegia, but not for those with incomplete paraplegia. Comparability of ability estimates across sub-groups was attained by anchoring all sub-groups on a testlet.
CONCLUSION: The SCIM-SR violates certain assumptions of the Rasch measurement model, as shown by the local dependency and differential item functioning. However, an intermediate solution to achieve fit in 3 out of 4 spinal cord injury sub-groups was found. For the time being, therefore, it advisable to use this approach to compute Rasch-transformed SCIM-SR scores.
Key words: functional status; independence; spinal cord injury; validity; reliability; psychometrics.
J Rehabil Med 2016; 48: 149–164
Correspondence address: Birgit Prodinger, ICF Unit, Swiss Paraplegic Research, CH-6207 Nottwil, Switzerland. E-mail: birgit.prodinger@paraplegie.ch
Accepted Dec 22, 2015; Epub ahead of print Feb 1, 2016
INTRODUCTION
Spinal cord injury (SCI) can result in a wide range of problems in functioning, including impairments of body structures and functions, limitations in activities of daily living, and restrictions in participation in social and community life (1). To respond to the health and related needs of persons with SCI, rehabilitation requires an interdisciplinary approach along the continuum of care from acute to early post-acute and long-term care, including community-based rehabilitation (2). Reliable and valid measures are therefore needed to monitor the functioning of people with SCI over time and evaluate the effectiveness of interventions. With this information it is then possible to allocate resources more effectively in response to the needs of people living with SCI.
The Spinal Cord Independence Measure – Self Report (SCIM-SR) is a relatively new self-report instrument for assessing functional independence of persons living with SCI (3). SCIM-SR was developed based on the clinician-administered SCIM III, a widely used instrument in SCI rehabilitation (4). Functional independence, as assessed with the SCIM-SR, is the ability of a person with SCI to perform specified activities independently of assistance or assistive devices. SCIM-SR, like the SCIM III, comprises 3 sub-scales: Self-Care, Respiration and Sphincter Management, and Mobility. The Mobility sub-scale contains items related to transfers and moving around indoors and outdoors. For each domain, the person is asked to indicate the extent of assistance or assistive devices needed to complete certain activities. The criterion validity of the German version of the SCIM-SR was supported by its high intra-class correlations with SCIM III sub-scale scores (range 0.80–0.86) and total score (0.90) (3). The Spanish version of the SCIM-SR showed near perfect concordance with SCIM III sub-scales and total score based on Lin’s concordance coefficient ranging from 0.988 to 0.998 (5).
The SCIM-SR widens the utility of the SCIM III for community surveys. Thus, in combination the SCIM III and the SCIM-SR are relevant instruments to monitor change in functional independence of persons with SCI from early post-acute to community-based rehabilitation. As for all versions of the SCIM, the SCIM-SR delivers an ordinal estimate of dependency, and so is non-linear. Such data must be interpreted with care when examining change, as this can lead to erroneous inferences, as apparently equal change on the ordinal scale may reflect a different amount of change depending on the baseline value (6, 7). Given the importance of monitoring change in the rehabilitation process, the Rasch measurement model can be used to derive interval scales from ordinal measures as well as examining other assumptions such as unidimensionality and group invariance. A Rasch analysis of the SCIM II (8) indicated vagueness in the wording of some items and their response categories. These findings have informed the development of SCIM III. Two studies using the Rasch model were conducted on the SCIM III (9, 10). Both studies again revealed ambiguity in the response categories of some items, as indicated by disordered response options leading to misfit of some items. No remedies have been undertaken to improve the fit of the SCIM III. Although the psychometric properties of the total score and subscale scores of the SCIM III have been examined from a classical test theory perspective (4), only the internal construct validity of the sub-scale scores, and not the total score, have been investigated based on Rasch analysis. However, the total score of the SCIM is commonly reported and used in statistical analyses in research (11–14). Unless there is evidence that the items can be summed into a common construct, the use of a total score is questionable for the monitoring of people’s functional independence over time. The aim of the current study was therefore to examine the internal construct validity and reliability of the SCIM-SR when administered in a community survey, using the Rasch measurement model, to assess the usefulness of the SCIM-SR total score for the assessment and monitoring of functional independence in people with SCI.
SUBJECTS AND METHODS
Subjects and setting
The Swiss Spinal Cord Injury Cohort Study (SwiSCI) community survey is a nationwide study conducted in collaboration with the 4 specialized Swiss SCI rehabilitation centres, the national association for persons living with SCI and their associates (Swiss Paraplegic Association), a SCI-specific home care institution (Parahelp) and a large national insurance company (SUVA). SwiSCI is hosted by Swiss Paraplegic Research, Nottwil, Switzerland. The SwiSCI community survey builds on a modular structure (15). The SCIM-SR was part of the Basic Module. Individuals aged 16 years or older, who reside in Switzerland and who have been diagnosed with traumatic or non-traumatic SCI are included in the study. The survey was available in the three official languages of Switzerland: German, French and Italian. Exclusion criteria include congenital conditions leading to SCI, new SCI in the context of palliative care, neurodegenerative disorders, and Guillain-Barré syndrome. The detailed recruitment process is outlined elsewhere (16). Participants were asked to complete the questionnaire on paper, online or by telephone interview. All information, including SCI characteristics, such as lesion level (paraplegia or tetraplegia) and degree (complete or incomplete) were self-reported. The SwiSCI community survey was formally approved by the respective regional Research Ethics Committees in the different sites. All participants gave written consent for the anonymous use of their data.
Measure
Similar to the SCIM III, the SCIM-SR consists of 17 items in 3 sub-scales (3): 6 items for Self-Care (raw score range 0–20), 4 items for Respiration and Sphincter Management (raw score range 0–40), and 9 items for Mobility (raw score range 0–40). It is worth mentioning that, in the SCIM-SR, items related to washing and dressing are divided into 2 sub-items each, 1 for the upper body, the other for the lower body, and items related to bladder and bowel management are divided into 3 sub-items. A scoring scheme was developed for the bladder and bowel management sub-items detailing the process of creating a single item score for each of these items (3). Each item of the SCIM-SR contributes between 0 and 15 points to the total score, which ranges from 0 to 100. Higher scores reflect higher functional independence. The detailed scoring format of each item is shown in Table II (second column).
Data analysis
Descriptive statistics were used to summarize the basic sample characteristics and response distributions. Floor and ceiling effects are present if at least 15% of the participants consistently provided minimum or maximum possible scores on the items addressed (17). The presence of floor and ceiling effects was investigated for the sample as a whole and for the subgroups by lesion level and degree. Descriptive analyses were performed with R Version 3.1.2 (18).
Rasch analysis is an iterative process that tests the extent to which the data satisfies a number of psychometric assumptions (19), including local item independency, unidimensionality and invariance. Rasch analyses were conducted with RUMM2030 (20). The Rasch model assumes that the higher a person’s ability the more likely the endorsement of the difficult items of a questionnaire. In the presence of items with polytomous response options, as in the SCIM-SR, the Partial Credit Model (PCM) is applied. This model from the Rasch family assumes that the distances between adjacent response options can vary within and across a scale. The equal probability point between 2 adjacent response options is called threshold (21).
The first assumption tested in this study was local item independency, which encompasses response and trait dependency of items. Response dependency implies that the response to 1 item is associated with the response of another item. Response independency is granted when there are no residual correlations > 0.2 between items left after extracting the Rasch factor (22). A preliminary analysis of the SCIM-SR total score indicated high item-person residual correlations indicating serious response dependency amongst items. A testlet design was applied to accommodate this high local dependency of the SCIM-SR items (23), an approach previously applied in a Rasch analysis of the Functional Independency Measure (FIM) (22). In this context it is worth mentioning that the SCIM development was influenced by the FIM (24). The testlets were constructed by aggregating the items with high residual correlations into super-items. The iterative process of scale adjustment based on Rasch analysis does not differ in a testlet design from a single item design, except for the examination of thresholds. Ordered thresholds are important when their order is expected to reflect an increase on the trait. Under the testlet design, this order is no longer expected (25).
Trait dependency is an indicator of the absence of unidimensionality of the scale, another assumption of the Rasch model. Unidimensionality can be examined with a principal component analysis (PCA) of the standardized Rasch residuals. If unidimensionality holds, no factor structure should be found in the residuals. This was tested with t-tests comparing pairs of ability estimates from separate Rasch calibration of the 2 sets of items, either loading positively or negatively on the first component of the PCA. The percentage of significant t-tests should not significantly exceed 5%, meaning that the lower boundary of the 95% confidence interval (95% CI) should not be above 5%.
The overall fit of the data to the Rasch model was examined with an overall χ2 statistic. This overall indicator for fit to the Rasch model constitutes a summary of individual item χ2 fit statistics. A non-significant χ2 is interpreted as evidence of good fit overall as well as on the individual item level. The significance level of the p-values for the overall model fit was adjusted for repeated measurement according to the Holm-Bonferroni strategy (26). Large negative-fit residuals are an indication that the item discriminates more strongly than expected by the Rasch model; large positive-fit residuals indicate weaker item discrimination than expected by the Rasch model.
The lack of item invariance across relevant group characteristics, so-called differential item functioning (DIF), is an important assumption in scale evaluation with the Rasch model. If no DIF is detected, it means that persons can achieve comparable levels of ability regardless of the group characteristics, e.g. that individuals with tetraplegia or paraplegia with the same ability have the same response probability on any item of the scale (27). DIF was investigated with an analysis of variance (ANOVA) test for gender (male and female), administration mode (paper-pencil or online), language (German or French), SCI aetiology (traumatic or non-traumatic), SCI level (paraplegia or tetraplegia), SCI degree (complete or incomplete), age and time since injury. Age and time since injury were dichotomized by the year threshold proposed for reporting by the International Spinal Cord Society (ISCoS) (28) closest to the median of the respective variable. Given the low, yet, for Switzerland, representative, number of questionnaires administered in Italian in this study, DIF was only examined for the difference between German and French. DIF can be resolved by splitting an item showing DIF for certain groups into group-specific items. This remedy provides different group-specific estimates of the item difficulty (29). Due to the structural missing values created in splitting items for DIF, the overall t-test for unidimensionality of the scales could be performed only on the remaining non-split items.
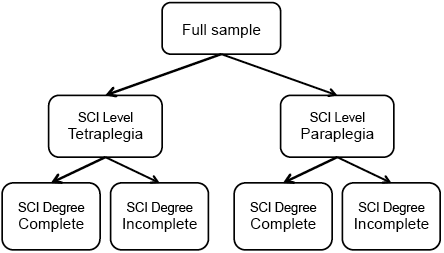
As our initial analysis revealed problems with the fit of the SCIM-SR to the Rasch model, we followed an analytic strategy that allowed examination of the metric properties in SCI-specific sub-groups in more detail while maintaining comparability across these groups. As illustrated in Fig. 1, as the starting point of the metric analysis we first fitted the Rasch model to the full sample. In case of misfit of the scale to the Rasch model due to DIF related to SCI characteristics, we divided the sample by SCI level and examined fit to the Rasch model of the SCIM-SR for each sub-group. If model fit was then still not achieved due to DIF related to degree, we would further split the respective samples by SCI degree implying the creation of a separate scale for each of the sub-groups. Subsequently, person parameters were estimated by weighted maximum likelihood estimates, taking into account that items with DIF had different item parameters in different groups. Thus, comparability across SCI sub-groups could be assured.
The reliability of the Rasch transformed SCIM-SR scores was evaluated by the person separation index (PSI). The value of the PSI can be interpreted similarly to that of the value of reliability in classical test theory (CTT). Under Rasch models the PSI is more appropriate than the CTT reliability, because the PSI refers to the reliability of the estimate of the person parameter of the Rasch model, whereas the reliability measure in CTT measures the reliability of the total raw score over all items. Values of approximately 0.70 and greater are acceptable for group level (30).
Finally, once a sound metric is achieved, the ability estimates derived from the Rasch analysis allow for constructing a user-friendly, unbiased, interval-scaled 0–100 metric. In the presence of items that were split for DIF, separate transformation tables are created for each sub-group level of the respective groups for which DIF split was performed; for instance, traumatic complete paraplegia in females, traumatic complete paraplegia in males, non-traumatic complete paraplegia in females, etc.
RESULTS
Out of 1,549 individuals with SCI who completed the Basic Module, 1,530 provided sufficient responses on the SCIM-SR to be included in the present analyses. No systematic pattern was observed in persons with high missing responses. Descriptive statistics of the study population stratified by SCI level and degree are shown in Table I.
Table I. Characteristics of the Swiss Spinal Cord Injury Cohort Study (SwiSCI) population of the community survey |
||||||
|
SwiSCI |
Tetraplegia |
|
Paraplegia |
||
Incomplete |
Complete |
|
Incomplete |
Complete |
||
Total, n |
1,530 |
310 |
156 |
|
569 |
483 |
Sex (female), n (%) |
437 (28.5) |
90 (29.0) |
25 (16.0) |
|
197 (34.6) |
122 (25.3) |
Aetiology (non-traumatic), n (%) |
327 (21.6) |
51 (16.6) |
8 (5.1) |
|
201 (35.6) |
64 (13.3) |
Language, n (%) |
|
|
|
|
|
|
German |
1,074 (70.2) |
228 (73.5) |
105 (67.3) |
|
392 (68.9) |
339 (70.2) |
French |
387 (25.3) |
68 (21.9) |
41 (26.3) |
|
154 (27.1) |
122 (25.3) |
Italian |
70 (4.6) |
14 (4.5) |
10 (6.4) |
|
23 (4.0) |
22 (4.6) |
Questionnaire type, n (%) |
|
|
|
|
|
|
Online |
633 (41.3) |
139 (44.8) |
103 (66.0) |
|
184 (32.3) |
200 (41.4) |
Paper form |
882 (57.6) |
167 (53.9) |
49 (31.4) |
|
378 (66.4) |
282 (58.4) |
Telephone interview |
16 (1.0) |
4 (1.3) |
4 (2.6) |
|
7 (1.2) |
1 (0.2) |
Age, years, mean (SD) |
52.33 (14.77) |
53.05 (15.63) |
49.57 (13.47) |
|
53.81 (15.37) |
51.08 (13.66) |
Education years, mean (SD) |
13.59 (3.26) |
13.34 (3.13) |
13.75 (3.40) |
|
13.44 (3.37) |
13.90 (3.14) |
Time since SCI, mean (SD) |
16.84 (12.70) |
14.34 (11.89) |
21.23 (13.39) |
|
13.70 (11.32) |
20.72 (13.05) |
Proportions are based on available information – missing values are not reported. SCI: spinal cord injury; SD: standard deviation. |
||||||
None of the participants in the study showed the lowest SCIM-SR total score possible. Some participants responded to every item with the maximal score, indicating that they experienced the highest level of independence that can be assessed with the SCIM-SR. The distribution of responses to the items is shown in Table II. Maximum scores were most frequent in the sub-groups with an incomplete injury, i.e. 11.4% and 12.3% of the persons with incomplete paraplegia and incomplete tetraplegia, respectively. Thus, no ceiling effects were revealed, as these figures were below the threshold of 15%. Certain response options were rare across SCI sub-groups; for example, the need for a respiration tube or permanent extra oxygen, walking indoors with supervision, walking moderate distances with walking frame or crutches, and walking 100 m with walking frame or crutches. Other response options were chosen by more than 90% of the persons with paraplegia; for example, eating and drinking independently but with assistive devices, being independent and not in need of supervision in grooming, and being able to breathe and cough independently and without assistance. The responses of people with tetraplegia showed a better distribution across response options in these items. There were also items for which the frequency of responses was more alike in persons with complete or incomplete lesions. For instance, both in persons with complete paraplegia and in those with tetraplegia, more than 90% of people indicated that they were unable to ascend or descend stairs.
Table II. Response distribution of raw scores and scoring format for each item of Spinal Cord Independence Measure – Self Report (SCIM-SR) stratified by spinal cord injury-specific sub-groups |
||||||||
|
SCIM-SR Raw Score |
Modified Raw Score |
Total n (%) |
Tetraplegia |
|
Paraplegia |
||
Incomplete n (%) |
Complete n (%) |
|
Incomplete n (%) |
Complete n (%) |
||||
Subscale: Self-Care |
|
|
|
|
|
|
|
|
Item 1 |
Eating and drinking |
|
|
|
|
|
|
|
I need artificial feeding or a stomach tube. |
0 |
0 0 |
30 (2.0) |
6 (2.0) |
19 (12.1) |
|
4 (0.7) |
0 (0.0) |
I need total assistance with eating/drinking. |
0 |
|||||||
I need partial assistance with eating/drinking or for putting on/taking off adaptive devices. |
1 |
1 |
36 (2.4) |
18 (5.9) |
11 (7.0) |
|
3 (0.5) |
4 (0.8) |
I eat/drink independently, but I need adaptive devices or assistance for cutting food, pouring drinks or opening containers. |
2 |
2 |
224 (14.8) |
94 (30.9) |
90 (57.3) |
|
31 (5.5) |
9 (1.9) |
I eat/drink independently without assistance or adaptive devices |
3 |
3 |
1,223 (80.8) |
186 (61.2) |
37 (23.6) |
|
524 (93.2) |
465 (97.3) |
Item 2A |
Washing your upper body and head |
|
|
|
|
|
||
I need total assistance. |
0 |
0 |
114 (7.5) |
43 (14.2) |
55 (35.0) |
|
9 (1.6) |
6 (1.3) |
I need partial assistance. |
1 |
1 |
182 (12.0) |
59 (19.5) |
43 (27.4) |
|
40 (7.1) |
40 (8.4) |
I am independent but need adaptive devices or specific equipment (e.g. bars, chairs). |
2 |
2 |
439 (29.0) |
66 (21.8) |
31 (19.7) |
|
149 (26.4) |
189 (39.6) |
I am independent and do not need adaptive devices or specific equipment. |
3 |
3 |
778 (51.4) |
135 (44.6) |
28 (17.8) |
|
366 (64.9) |
242 (50.7) |
Item 2B |
Washing your lower body |
|
|
|
|
|
|
|
I need total assistance. |
0 |
0 |
242 (16.1) |
79 (26.3) |
96 (61.1) |
|
27 (4.8) |
39 (8.2) |
I need partial assistance. |
1 |
1 |
163 (10.8) |
34 (11.3) |
31 (19.7) |
|
35 (6.3) |
62 (13.0) |
I am independent but need adaptive devices or a specific equipment (e.g. bars, chairs). |
2 |
2 |
509 (33.8) |
76 (25.3) |
20 (12.7) |
|
181 (32.4) |
227 (47.7) |
I am independent and do not need adaptive devices or specific equipment. |
3 |
3 |
590 (39.2) |
111 (37.0) |
10 (6.4) |
|
316 (56.5) |
148 (31.1) |
Item 3A |
Dressing your upper body |
|
|
|
|
|
|
|
I need total assistance. |
0 |
0 |
151 (10.0) |
61 (20.0) |
73 (46.5) |
|
7 (1.2) |
9 (1.9) |
I need partial assistance, even with easy-to-dress clothes. |
1 |
1 |
114 (7.5) |
35 (11.5) |
30 (19.1) |
|
26 (4.6) |
23 (4.8) |
I do not need assistance with easy-to-dress clothes, but I need adaptive devices or specific equipment. |
2 |
2 |
26 (1.7) |
6 (2.0) |
8 (5.1) |
|
6 (1.1) |
5 (1.0) |
I am independent with easy-to-dress clothes and only need assistance or adaptive devices or a specific setting with difficult-to-dress clothes. |
3 |
3 |
12 (14.0) |
61 (20.0) |
26 (16.6) |
|
63 (11.2) |
62 (13.0) |
I am completely independent. |
4 |
4 |
1,014 (66.8) |
142 (46.6) |
20 (12.7) |
|
463 (81.9) |
379 (79.3) |
Item 3B |
Dressing your lower body |
|
|
|
|
|
|
|
I need total assistance. |
0 |
0 |
257 (16.9) |
89 (28.9) |
104 (66.2) |
|
29 (5.1) |
34 (7.1) |
I need partial assistance, even with easy-to-dress clothes. |
1 |
1 |
92 (6.1) |
21 (6.8) |
16 (10.2) |
|
22 (3.9) |
33 (6.9) |
I do not need assistance with easy-to-dress clothes, but I need adaptive devices or specific equipment. |
2 |
2 |
21 (1.4) |
2 (0.6) |
2 (1.3) |
|
5 (0.9) |
12 (2.5) |
I am independent with easy-to-dress clothes and only need assistance or adaptive devices or a specific setting with difficult-to-dress clothes. |
3 |
3 |
212 (14.0) |
53 (17.2) |
19 (12.1) |
|
80 (14.2) |
59 (12.4) |
I am completely independent. |
4 |
4 |
936 (61.7) |
143 (46.4) |
16 (10.2) |
|
428 (75.9) |
339 (71.1) |
Item 4 |
Grooming |
|
|
|
|
|
|
|
I need total assistance. |
0 |
0 |
74 (4.8) |
29 (9.4) |
40 (25.5) |
|
3 (0.5) |
1 (0.2) |
I need partial assistance. |
1 |
1 |
103 (6.7) |
37 (12.0) |
36 (22.9) |
|
20 (3.5) |
10 (2.1) |
I am independent with adaptive devices. |
2 |
2 |
103 (6.7) |
32 (10.4) |
17 (10.8) |
|
32 (5.6) |
21 (4.4) |
I am independent without adaptive devices. |
3 |
3 |
1,247 (81.7) |
211 (68.3) |
64 (40.8) |
|
512 (90.3) |
450 (93.4) |
Subscale: Sphincter & Respiration |
|
|
|
|
|
|
|
|
Item 5 |
Breathing |
|
|
|
|
|
|
|
I need a respiratory (tracheal) tube … |
|
|
|
|
|
|
|
|
as well as permanent or from time to time assisted ventilation. |
0 |
0 |
5 (0.3) |
1 (0.3) |
2 (1.3) |
|
1 (0.2) |
1 (0.2) |
as well as extra oxygen and a lot of assistance in coughing or respiratory tube management. |
2 |
1 |
1 (0.1) |
1 (0.3) |
0 (0.0) |
|
0 (0.0) |
0 (0.0) |

Table II. Contd. |
||||||||
|
SCIM-SR Raw Score |
Modified Raw Score |
Total n (%) |
Tetraplegia |
|
Paraplegia |
||
Incomplete n (%) |
Complete n (%) |
|
Incomplete n (%) |
Complete n (%) |
||||
as well as little assistance in coughing or respiratory tube management. |
4 |
2 |
4 (0.3) |
2 (0.7) |
0 (0.0) |
|
1 (0.2) |
1 (0.2) |
I do not need a respiratory (tracheal) tube … |
|
|
|
|
|
|
|
|
but I need extra oxygen or a lot of assistance in coughing or a mask (e.g. PEEP) or assisted ventilation from time to time (e.g. BIPAP). |
6 |
3 |
50 (3.5) |
13 (4.4) |
16 (10.6) |
|
13 (2.5) |
7 (1.5) |
and only little assistance or stimulation for coughing. |
8 |
4 |
64 (4.4) |
20 (6.8) |
30 (19.9) |
|
6 (1.1) |
8 (1.7) |
and can breathe and cough independently without any assistance or adaptive devices. |
10 |
5 |
1,324 (91.4) |
257 (87.4) |
103 (68.2) |
|
506 (96.0) |
447 (96.3) |
Item 6 |
Bladder management |
|
|
|
|
|
|
|
Scoring of item 6: see Appendix B in Fekete et al. 2013 |
0 |
0 |
244 (17.7) |
62 (22.5) |
48 (33.6) |
|
61 (12.0) |
73 (16.4) |
6 |
1 |
184 (13.3) |
45 (16.4) |
62 (43.4) |
|
29 (5.7) |
47 (10.6) |
|
9 |
2 |
306 (22.2) |
18 (6.5) |
9 (6.3) |
|
100 (19.7) |
178 (40.0) |
|
11 |
3 |
161 (11.7) |
23 (8.4) |
8 (5.6) |
|
63 (12.4) |
66 (14.8) |
|
13 |
4 |
151 (10.9) |
29 (10.5) |
6 (4.2) |
|
54 (10.7) |
62 (13.9) |
|
15 |
5 |
334 (24.2) |
98 (35.6) |
10 (7.0) |
|
200 (39.4) |
19 (4.3) |
|
Item 7 |
Bowel management |
|
|
|
|
|
|
|
Scoring of item 7: see Appendix C in Fekete et al. 2013 |
0 |
0 |
195 (13.5) |
40 (14.0) |
15 (9.7) |
|
98 (18.5) |
40 (8.8) |
5 |
1 |
463 (32.2) |
105 (36.7) |
119 (77.3) |
|
109 (20.5) |
129 (28.2) |
|
8 |
2 |
203 (14.1) |
22 (7.7) |
6 (3.9) |
|
80 (15.1) |
93 (20.4) |
|
10 |
3 |
579 (40.2) |
119 (41.6) |
14 (9.1) |
|
244 (46.0) |
195 (42.7) |
|
Item 8 |
Using the toilet |
|
|
|
|
|
|
|
I need total assistance. |
0 |
0 |
213 (14.3) |
74 (24.5) |
91 (59.9) |
|
18 (3.2) |
29 (6.2) |
I need partial assistance and cannot clean myself. |
1 |
1 |
56 (3.8) |
9 (3.0) |
19 (12.5) |
|
5 (0.9) |
23 (4.9) |
I need partial assistance but can clean myself. |
2 |
2 |
83 (5.6) |
15 (5.0) |
15 (9.9) |
|
25 (4.5) |
27 (5.8) |
I do not need assistance but I need adaptive devices (e.g. bars) or a special setting (e.g. wheelchair accessible toilet). |
4 |
3 |
573 (38.4) |
71 (23.5) |
22 (14.5) |
|
183 (32.8) |
294 (63.0) |
I do not need any assistance, adaptive devices or a special setting. |
5 |
4 |
566 (38.0) |
133 (44.0) |
5 (3.3) |
|
327 (58.6) |
94 (20.1) |
Subscale Mobility |
|
|
|
|
|
|
|
|
Item 9 |
Movement without assistance or electric aids |
|
|
|
|
|||
None, I need assistance in all these activities [see examples in Fekete et al. 2013] |
0 |
0 |
246 (16.4) |
59 (19.4) |
85 (55.2) |
|
49 (8.9) |
50 (10.4) |
One |
2 |
1 |
100 (6.7) |
27 (8.9) |
18 (11.7) |
|
26 (4.7) |
29 (6.0) |
Two or three |
4 |
2 |
211 (14.1) |
54 (17.8) |
26 (16.9) |
|
46 (8.4) |
85 (17.7) |
All of them |
6 |
3 |
940 (62.8) |
164 (53.9) |
25 (16.2) |
|
428 (78.0) |
316 (65.8) |
Item 10 |
Transfers from the bed to the wheelchair |
|
|
|
|
|
||
I need total assistance. |
0 |
0 |
162 (10.8) |
50 (16.5) |
80 (51.0) |
|
12 (2.2) |
19 (4.0) |
I need partial assistance, supervision or adaptive devices (e.g. sliding board). |
1 |
1 |
243 (16.2) |
49 (16.2) |
42 (26.8) |
|
45 (8.2) |
107 (22.3) |
I do not need any assistance or adaptive devices. |
2 |
2 |
1,092 (72.9) |
204 (67.3) |
35 (22.3) |
|
490 (89.6) |
353 (73.7) |
I do not use a wheelchair. |
2 |
2 |
||||||
Item 11 |
Transfers from the wheelchair to the toilet/tub |
|
|
|
|
|||
I need total assistance. |
0 |
0 |
237 (16.0) |
75 (24.9) |
101 (65.6) |
|
22 (4.1) |
38 (8.0) |
I need partial assistance, supervision or adaptive devices (e.g. grab-bars). |
1 |
1 |
419 (28.3) |
59 (19.6) |
40 (26.0) |
|
101 (18.7) |
218 (46.1) |
I do not need any assistance or adaptive devices. |
2 |
2 |
823 (55.6) |
167 (55.5) |
13 (8.4) |
|
418 (77.3) |
216 (45.8) |
I do not use a wheelchair. |
2 |
2 |
||||||
Item 12 |
Moving around indoors |
|
|
|
|
|
||
I use a wheelchair. To move around, … |
|
|
|
|
|
|
|
|
I need total assistance. |
0 |
0 |
33 (2.2) |
3 (1.0) |
12 (7.7) |
|
10 (1.9) |
8 (1.7) |
I need an electric wheelchair or partial assistance to operate a manual wheelchair. |
1 |
1 |
123 (8.3) |
45 (15.0) |
42 (26.9) |
|
17 (3.1) |
18 (3.8) |
I am independent in a manual wheelchair. |
2 |
2 |
807 (54.3) |
103 (34.3) |
95 (60.9) |
|
168 (31.1) |
437 (91.2) |
I walk indoors and I … |
|
|
|
|
|
|
|
|
need supervision while walking (with or without walking aids). |
3 |
3 |
15 (1.0) |
7 (2.3) |
1 (0.6) |
|
5 (0.9) |
2 (0.4) |
walk with a walking frame or crutches, swinging forward with both feet at a time. |
4 |
4 |
14 (0.9) |
6 (2.0) |
0 (0.0) |
|
7 (1.3) |
1 (0.2) |

Table II. Contd. |
||||||||
|
SCIM-SR Raw Score |
Modified Raw Score |
Total n (%) |
Tetraplegia |
|
Paraplegia |
||
Incomplete n (%) |
Complete n (%) |
|
Incomplete n (%) |
Complete n (%) |
||||
walk with crutches or two canes, setting one foot before the other. |
5 |
5 |
95 (6.4) |
12 (4.0) |
2 (1.3) |
|
77 (14.3) |
4 (0.8) |
walk with one cane. |
6 |
6 |
49 (3.3) |
15 (5.0) |
1 (0.6) |
|
33 (6.1) |
0 (0.0) |
walk with a leg orthosis(es) only (e.g. leg splint). |
7 |
7 |
42 (2.8) |
4 (1.3) |
0 (0.0) |
|
31 (5.7) |
6 (1.3) |
walk without walking aids. |
8 |
8 |
308 (20.7) |
105 (35.0) |
3 (1.9) |
|
192 (35.6) |
3 (0.6) |
Item 13 |
Moving around moderate distances (10 to 100 m) |
|
|
|
|
|||
I use a wheelchair. To move around, … |
|
|
|
|
|
|
|
|
I need total assistance. |
0 |
0 |
59 (4.0) |
12 (4.0) |
18 (11.7) |
|
13 (2.4) |
15 (3.2) |
I need an electric wheelchair or partial assistance to operate a manual wheelchair. |
1 |
1 |
204 (13.8) |
62 (20.8) |
63 (40.9) |
|
35 (6.5) |
44 (9.3) |
I am independent in a manual wheelchair. |
2 |
2 |
686 (46.5) |
76 (25.5) |
63 (40.9) |
|
143 (26.5) |
400 (84.7) |
I walk moderate distances and I … |
|
|
|
|
|
|
|
|
need supervision while walking (with or without walking aids). |
3 |
3 |
24 (1.6) |
8 (2.7) |
4 (2.6) |
|
10 (1.9) |
2 (0.4) |
walk with a walking frame or crutches, swinging forward with both feet at a time. |
4 |
4 |
12 (0.8) |
6 (2.0) |
0 (0.0) |
|
6 (1.1) |
0 (0.0) |
walk with crutches or two canes, setting one foot before the other. |
5 |
5 |
135 (9.2) |
26 (8.7) |
2 (1.3) |
|
104 (19.3) |
3 (0.6) |
walk with one cane. |
6 |
6 |
67 (4.5) |
24 (8.1) |
0 (0.0) |
|
43 (8.0) |
0 (0.0) |
walk with a leg orthosis(es) only (e.g. leg splint). |
7 |
7 |
41 (2.8) |
3 (1.0) |
0 (0.0) |
|
32 (5.9) |
5 (1.1) |
walk without walking aids. |
8 |
8 |
246 (16.7) |
81 (27.2) |
4 (2.6) |
|
154 (28.5) |
3 (0.6) |
Item 14 |
Moving around outdoors for more than 100 m |
|
|
|
|
|||
I use a wheelchair. To move around, … |
|
|
|
|
|
|
|
|
I need total assistance. |
0 |
0 |
99 (6.7) |
24 (8.0) |
25 (16.4) |
|
24 (4.4) |
25 (5.3) |
I need an electric wheelchair or partial assistance to operate a manual wheelchair. |
1 |
1 |
349 (23.5) |
97 (32.2) |
81 (53.3) |
|
75 (13.7) |
96 (20.2) |
I am independent in a manual wheelchair. |
2 |
2 |
563 (37.9) |
47 (15.6) |
39 (25.7) |
|
131 (23.9) |
342 (72.0) |
I walk more than 100 meters and I … |
|
|
|
|
|
|
|
|
need supervision while walking (with or without walking aids). |
3 |
3 |
19 (1.3) |
6 (2.0) |
1 (0.7) |
|
9 (1.6) |
3 (0.6) |
walk with a walking frame or crutches, swinging forward with both feet at a time. |
4 |
4 |
8 (0.5) |
3 (1.0) |
0 (0.0) |
|
5 (0.9) |
0 (0.0) |
walk with crutches or two canes, setting one foot before the other. |
5 |
5 |
118 (7.9) |
22 (7.3) |
1 (0.7) |
|
90 (16.5) |
4 (0.8) |
walk with one cane. |
6 |
6 |
58 (3.9) |
20 (6.6) |
1 (0.7) |
|
37 (6.8) |
0 (0.0) |
walk with a leg orthosis(es) only (e.g. leg splint). |
7 |
7 |
36 (2.4) |
3 (1.0) |
0 (0.0) |
|
30 (5.5) |
3 (0.6) |
walk without walking aids. |
8 |
8 |
235 (15.8) |
79 (26.2) |
4 (2.6) |
|
146 (26.7) |
2 (0.4) |
Item 15 |
Going up or down stairs |
|
|
|
|
|
||
I am unable to go up and down stairs. |
0 |
0 |
844 (58.8) |
135 (46.6) |
141 (96.6) |
|
147 (27.2) |
416 (92.9) |
I can go up and down at least 3 steps … |
|
|
|
|
|
|
|
|
but only with assistance or supervision. |
1 |
1 |
47 (3.3) |
10 (3.4) |
0 (0.0) |
|
21 (3.9) |
16 (3.6) |
but only with devices (e.g. handrail, crutch, cane). |
2 |
2 |
281 (19.6) |
59 (20.3) |
2 (1.4) |
|
203 (37.6) |
14 (3.1) |
without any assistance, supervision or devices. |
3 |
3 |
264 (18.4) |
86 (29.7) |
3 (2.1) |
|
169 (31.3) |
2 (0.4) |
Item 16 |
Transfers from the wheelchair into the car |
|
|
|
|
|||
I need total assistance. |
0 |
0 |
216 (14.6) |
69 (23.3) |
77 (50.3) |
|
29 (5.3) |
40 (8.4) |
I need partial assistance, supervision or adaptive devices. |
1 |
1 |
366 (24.7) |
69 (23.3) |
49 (32.0) |
|
84 (15.3) |
163 (34.2) |
I do not need any assistance or adaptive devices. |
2 |
2 |
901 (60.8) |
158 (53.4) |
27 (17.6) |
|
435 (79.4) |
272 (57.3) |
I do not use a wheelchair. |
2 |
2 |
||||||
Item 17 |
Transfers from the floor to the wheelchair |
|
|
|
|
|||
I need assistance. |
0 |
0 |
841 (53.1) |
168 (51.5) |
149 (94.7) |
|
171 (27.4) |
349 (71.4) |
I do not need any assistance. |
1 |
1 |
689 (46.8) |
142 (48.5) |
8 (5.3) |
|
398 (72.6) |
133 (28.5) |
I do not use a wheelchair. |
1 |
1 |
||||||
Maximum Total Score |
100 |
74 |
|
|
|
|
|
|
Proportions are based on available information – missing values are not reported. PEEP: positive end-expiratory pressure; BIPAP: bi-level positive airway pressure. |
||||||||
The initial Rasch analysis with the full sample did not fit the assumptions of the Rasch model. As DIF for lesion level was found for all items except for SCIM-SR Item 7 Breathing (Table III), we proceeded with separate sub-group analyses for persons with tetraplegia and paraplegia. Furthermore, residual correlations of the Rasch residuals indicated clear issues of local dependency with similar patterns to those of the sub-scale structure of the SCIM-SR. To accommodate this issue, we opted for a testlet design by grouping items into the 3 underlying sub-scales (Table III). Following this strategy, the SCIM-SR revealed good model fit in the sub-group of persons with tetraplegia after adjusting for DIF related to time since injury, gender, and age in the Mobility testlet (Table IV). In the sub-group of persons with paraplegia, however, the strong misfit of SCIM-SR to the Rasch model persisted with strong DIF for SCI degree. A distinct sub-group analysis of persons with complete and incomplete paraplegia resulted in model fit for the group of complete paraplegia after also adjusting for DIF related to gender and SCI aetiology. The testlet design showed unidimensionality in most groups; only the group of persons with complete paraplegia presented a percentage of significant pairwise differing ability estimates slightly above 5% (lower limit of confidence interval 5%). In persons with incomplete paraplegia no model fit of the SCIM-SR was achieved even after accommodating for DIF related to age in the Self-Care testlet. Table IV shows the findings of the model fit statistics including targeting, local dependency, unidimensionality and DIF for all sub-groups; the table contains, for each analysis, the 3 testlet design before any remedies have been applied and the best fitting solution based on the 3 testlet design after relevant remedies. The detailed findings of the models reported in Table IV, namely the item difficulty and fit statistics, the split strategies, uniform and non-uniform DIF and the eigenvalues and first component, are all shown in Appendix I.
Table III. Findings of preliminary Rasch analysis based on individual items of the Spinal Cord Independence Measure – Self Report (SCIM-SR) of the full sample |
||||||||||||||||
|
Item difficulty |
|
Item fit |
|
Local item dependency Residual correlations > 0.2 |
Differential item functioning (DIF) Sub-groups with DIF |
Unidimensionality (PCA) |
|||||||||
Subscale |
Item |
Label |
Location |
SE |
|
Fit residuals |
DF |
χ2 |
Df |
p-value |
Disordered thresholds |
|
Eigenvalue |
Loadings first component |
||
Self-Care |
1 |
Eating and drinking |
–1.971 |
0.059 |
|
–0.315 |
1,325.52 |
63.178 |
9 |
0.0000 |
Yes |
|
2A; 3A°; 3B; 4 |
Level; Type |
3.657 |
–0.437 |
2A |
Washing your upper body and head |
–0.507 |
0.041 |
|
–1.181 |
1,325.52 |
83.74 |
9 |
0.0000 |
|
|
1; 2B*; 3A°; 3B; 4 |
Level; Type |
2.57 |
–0.521 |
|
2B |
Washing your lower body |
0.279 |
0.037 |
|
–7.718 |
1,318.92 |
132.948 |
9 |
0.0000 |
Yes |
|
2A*; 3A; 3B°; 8; 11 |
Level |
1.616 |
–0.561 |
|
3A |
Dressing your upper body |
–0.455 |
0.034 |
|
1.605 |
1,329.3 |
77.672 |
9 |
0.0000 |
Yes |
|
1°; 2A°; 2B; 3B***; 4 |
Level; Type |
1.148 |
–0.640 |
|
3B |
Dressing your lower body |
0.074 |
0.030 |
|
–2.024 |
1,330.24 |
94.062 |
9 |
0.0000 |
Yes |
|
1; 2A; 2B°; 3A*** |
Level; Type |
1.052 |
–0.661 |
|
4 |
Grooming |
–1.381 |
0.049 |
|
0.639 |
1,339.67 |
33.51 |
9 |
0.0001 |
Yes |
|
1; 2A; 3A |
Level; Type |
0.975 |
–0.428 |
|
Sphincter & Respiration |
5 |
Breathing |
–1.645 |
0.043 |
|
5.754 |
1,267.97 |
315.785 |
9 |
0.0000 |
Yes |
|
|
|
0.937 |
–0.134 |
6 |
Bladder management |
0.800 |
0.025 |
|
16.682 |
1,215.14 |
335.236 |
9 |
0.0000 |
Yes |
|
|
Level; Type |
0.91 |
0.058 |
|
7 |
Bowel management |
0.435 |
0.034 |
|
18.558 |
1,263.26 |
793.134 |
9 |
0.0000 |
Yes |
|
|
Level; Type |
0.817 |
–0.097 |
|
8 |
Using the toilet |
0.119 |
0.034 |
|
–7.024 |
1,306.65 |
123.036 |
9 |
0.0000 |
Yes |
|
2B; 11 |
Level; Type |
0.776 |
–0.277 |
|
Mobility |
9 |
Movement without assistance or electric aids |
–0.042 |
0.036 |
|
14.471 |
1,312.31 |
360.711 |
9 |
0.0000 |
Yes |
|
|
Type |
0.713 |
–0.144 |
10 |
Transfers from the bed to the wheelchair |
–0.942 |
0.053 |
|
–9.389 |
1,314.2 |
157.522 |
9 |
0.0000 |
|
|
11°; 16°; 17 |
Level; Type |
0.689 |
–0.198 |
|
11 |
Transfers from the wheelchair to the toilet/tub |
–0.158 |
0.047 |
|
–10.945 |
1,297.22 |
179.209 |
9 |
0.0000 |
|
|
2B; 8; 10°; 16°; 17° |
Level; Type |
0.594 |
–0.186 |
|
12 |
Moving around indoors |
0.369 |
0.021 |
|
1.736 |
1,303.82 |
77.379 |
9 |
0.0000 |
Yes |
|
13**; 14°; 15° |
Level; Type |
0.573 |
0.668 |
|
13 |
Moving around moderate distances (10 to 100 m) |
0.913 |
0.022 |
|
–1.809 |
1,293.45 |
100.756 |
9 |
0.0000 |
Yes |
|
12**; 14**; 15° |
Level; Type |
0.534 |
0.714 |
|
14 |
Moving around outdoors for more than 100 m |
1.224 |
0.021 |
|
0.443 |
1,302.88 |
43.93 |
9 |
0.0000 |
Yes |
|
12°; 13**; 15 |
Level |
0.473 |
0.607 |
|
15 |
Going up or down stairs |
1.849 |
0.034 |
|
–3.040 |
1,258.54 |
262.307 |
9 |
0.0000 |
Yes |
|
12°; 13°; 14; 17 |
Level; Type |
0.377 |
0.547 |
|
16 |
Transfers from the wheelchair into the car |
–0.324 |
0.048 |
|
–7.782 |
1,303.82 |
121.481 |
9 |
0.0000 |
|
|
10°; 11°; 17; |
Level |
0.337 |
–0.147 |
|
17 |
Transfers from the floor to the wheelchair |
1.365 |
0.062 |
|
–8.815 |
1,291.56 |
238.429 |
9 |
0.0000 |
|
|
10; 11°; 15; 16 |
Level; Type |
0.252 |
0.050 |
|
°r > 0.3; *r > 0.4; **r > 0.5; ***r > 0.6. PCA: principal component analysis; level refers to paraplegia and tetraplegia; degree refers to complete or incomplete lesion; Df: degrees of freedom. |
||||||||||||||||
Table IV. Fit statistics, including targeting, unidimensionality, local dependency and differential item functioning (DIF) for all sub-groups. For each analysis the fit statistics for the 3 testlet solutions before and after any remedies are applied are presented respectively. For the Swiss Spinal Cord Injury Cohort Study (SwiSCI) sample of the Basic module the first line represents the fit statistics prior to the 3 testlet solution |
||||||||||||||||||||||||||
Analysis |
n |
Location |
|
Fit Residual |
|
Item-trait interaction χ2 |
|
Reliability PSI |
|
Unidimensionality Paired t-tests |
|
|
|
|||||||||||||
Item |
|
Persons |
|
Item |
|
Persons |
||||||||||||||||||||
Mean |
SD |
|
Mean |
SD |
|
Mean |
SD |
|
Mean |
SD |
|
Value |
Df |
p-value |
|
WITH extremes |
NO extremes |
|
n Significant tests |
Sample |
% PST |
CI % PST |
LD |
DIF |
||
SwiSCI sample (Basic module) |
1,530 |
0.000 |
1.018 |
|
1.056 |
1.587 |
|
–0.008 |
8.643 |
|
–0.368 |
1.150 |
|
3 ,594.0 |
171 |
0.0000* |
|
0.919 |
0.936 |
|
211 |
1,422 |
14.8 |
13.7–16.0 |
Yes |
Yes |
3 Testlets |
1,498 |
0.000 |
0.683 |
|
0.870 |
0.878 |
|
1.074 |
3.696 |
|
–0.454 |
0.858 |
|
168.5 |
27 |
0.0000* |
|
0.836 |
0.881 |
|
65 |
1,179 |
5.5 |
4.3–6.8 |
|
Yes |
Paraplegia |
1,052 |
0.000 |
1.1517 |
|
1.45 |
1.363 |
|
0.0858 |
6.7998 |
|
–0.306 |
0.9408 |
|
2,464.3 |
171 |
0.0000* |
|
0.894 |
0.901 |
|
145 |
983 |
14.8 |
13.4–16.1 |
Yes |
Yes |
3 Testlets |
1,029 |
0.000 |
0.498 |
|
1.017 |
0.653 |
|
0.896 |
4.125 |
|
–0.388 |
0.807 |
|
151.4 |
27 |
0.0000* |
|
0.742 |
0.777 |
|
49 |
815 |
6.0 |
4.5–7.5 |
|
Yes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Complete Paraplegia |
482 |
0.000 |
2.503 |
|
0.858 |
1.130 |
|
2.444 |
3.820 |
|
–0.294 |
0.646 |
|
679.3 |
133 |
0.0000* |
|
0.869 |
0.863 |
|
41 |
480 |
8.5 |
6.6–10.5 |
Yes |
Yes |
3 Testlets |
480 |
0.000 |
0.836 |
|
1.031 |
0.678 |
|
0.701 |
1.189 |
|
–0.502 |
0.909 |
|
52.4 |
21 |
0.0002* |
|
0.786 |
0.799 |
|
29 |
410 |
7.1 |
5.0–8.2 |
|
Yes |
3 Testlets Final |
483 |
0.000 |
0.850 |
|
0.762 |
0.739 |
|
0.197 |
2.436 |
|
–0.516 |
1.006 |
|
45.4 |
35 |
0.1113 |
|
0.785 |
0.791 |
|
|
|
|
|
|
|
Incomplete Paraplegia |
569 |
0.000 |
0.986 |
|
1.812 |
1.445 |
|
–0.357 |
4.914 |
|
–0.197 |
1.019 |
|
1,506.2 |
152 |
0.0000 |
|
0.865 |
0.889 |
|
90 |
503 |
17.9 |
16.0–19.8 |
Yes |
Yes |
3 Testlets |
559 |
0.000 |
0.312 |
|
0.865 |
0.613 |
|
–0.063 |
3.378 |
|
–0.324 |
0.733 |
|
78.0 |
24 |
0.0000* |
|
0.611 |
0.691 |
|
21 |
405 |
5.2 |
3.1–7.3 |
|
Yes |
3 Testlets Final |
559 |
0.000 |
0.261 |
|
0.970 |
0.618 |
|
0.141 |
2.423 |
|
–0.325 |
0.720 |
|
108.9 |
40 |
0.0000* |
|
0.614 |
0.691 |
|
|
|
|
|
|
|
Tetraplegia |
462 |
0.000 |
0.933 |
|
0.357 |
1.929 |
|
–0.287 |
4.801 |
|
–0.333 |
1.261 |
|
1,031.4 |
133 |
0.0000* |
|
0.937 |
0.949 |
|
69 |
427 |
16.2 |
14.1–18.2 |
Yes |
Yes |
3 Testlets |
462 |
0.000 |
0.887 |
|
0.557 |
1.152 |
|
0.443 |
0.985 |
|
–0.491 |
0.891 |
|
40.5 |
21 |
0.0064* |
|
0.870 |
0.898 |
|
15 |
356 |
4.2 |
1.9–6.5 |
|
Yes |
3 Testlets Final |
462 |
0.000 |
0.730 |
|
0.166 |
1.306 |
|
–0.020 |
1.020 |
|
–0.489 |
0.911 |
|
32.9 |
41 |
0.8140 |
|
0.894 |
0.904 |
|
|
|
|
|
|
|
Anchored analyses |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Anchor: 3 Testlet Complete Paraplegia |
483 |
0.000 |
0.850 |
|
0.762 |
0.739 |
|
0.197 |
2.436 |
|
–0.516 |
1.006 |
|
45.4 |
35 |
0.1113 |
|
0.785 |
0.791 |
|
|
|
|
|
|
|
3 Testlet Incomplete Paraplegia |
559 |
–0.114 |
0.507 |
|
1.415 |
0.957 |
|
2.023 |
3.267 |
|
–0.151 |
0.789 |
|
117.6 |
40 |
0.0000* |
|
0.737 |
0.777 |
|
|
|
|
|
|
|
3 Testlet Tetraplegia |
462 |
0.317 |
0.654 |
|
0.432 |
1.544 |
|
1.686 |
2.007 |
|
–0.352 |
1.043 |
|
62.7 |
41 |
0.0160 |
|
0.911 |
0.927 |
|
|
|
|
|
|
|
*p < 0.01 PSI: person separation index; PST: percentage of significant t-tests; CI: confidence interval; LD: local dependency; SD: standard deviation; Df: degrees of freedom. |
||||||||||||||||||||||||||
To allow for comparability across SCI sub-groups, all sub-group analyses were anchored on the parameters of the Respiration and Sphincter testlet from the sub-group analysis in persons with complete paraplegia. This testlet was chosen as it showed good fit and invariance across all relevant groups in all the Rasch models undertaken. The results of the anchor analysis are shown at the bottom of Table IV.
Analysis of the Rasch model’s targeting revealed that the mean person’s ability is higher than the mean level of independence of the scale. The group of persons with incomplete paraplegia appeared the most-off target, with mean abilities more than 1.5 logit above the mean item difficulty in the final anchored model. The group of persons which is the best addressed by the SCIM-SR is those with tetraplegia. The application of the testlet design and the adjustments for DIF improved the targeting.
Fig. 2 illustrates the distribution of the person ability estimates stratified by SCI sub-groups. The sub-group of persons with incomplete paraplegia resulted in having the highest independence (mean 73.27; standard deviation (SD) 10.31), followed by the sub-groups of persons with incomplete tetraplegia (mean 67.87; SD 16.26) and complete paraplegia (mean 66.3; SD 7.94). The sub-group of people with complete tetraplegia had the highest functional dependency (mean 52.78; SD 7.94) as measured with the SCIM-SR.
The transformation table of the raw scores into a user-friendly, interval-scaled 0–100 metric is shown in Appendix II. It is worth mentioning, that prior to conducting the Rasch analysis, and ultimately to apply the transformation table, the response options for some item scores of the SCIM-SR had to be re-coded starting with 0, as shown in Table III. After re-coding of the SCIM-SR items, the maximum score of the SCIM-SR was 74, compared with an unmodified score of 100.
DISCUSSION
This study provides first evidence from a Rasch measurement perspective of the internal construct validity and reliability of the SCIM-SR in people with traumatic and non-traumatic SCI living in Switzerland, and provides supporting evidence for the usefulness of the SCIM-SR, a relatively newly developed self-report instrument for the assessment and monitoring of functional independence in people with SCI. Applying a testlet design aligned with the sub-scale structure of the SCIM-SR made it possible to adjust for the high number of locally dependent items in the SCIM-SR. As local dependency was not the only salient issue, but also DIF for SCI-related groups, a testlet and sub-group design was applied. After conducting sub-group analyses, fit to the Rasch model was achieved in the sub-group of persons with tetraplegia and complete paraplegia, but not in the sub-group of persons with incomplete paraplegia. Anchoring all sub-groups onto a common testlet adjusted for invariance in item difficulty caused by the injury characteristics and made it possible to retain comparability of ability estimates across SCI sub-groups.
The testlet approach is user-friendly, aggregating the locally dependent items together to make a super-item. This makes it possible to maintain the scoring tradition of the SCIM III, and recommended scoring for the SCIM-SR, namely that scores for each item can be summed into a total score. From a methodological point of view, the testlet solution is promising as it takes the information for all items into account in the scoring, while accommodating the locally dependent items. From a clinical management and researchers’ point of view, having a total score on functional independence of people with SCI is convenient for outcome evaluation and clinical resource allocation.
The various DIF patterns that emerged in different sub-groups reflect the complexity of SCI, especially with regards to effects of injury characteristics and injury level and degree. Methodologically speaking, this does not cause a problem as it can be adjusted for statistically and accounted for in group-specific transformation tables (see Appendix II). To accommodate the high DIF for lesion level across almost all items, we split the sample into SCI-relevant sub-groups and subsequently applied an anchor design. Despite a complex analytical approach, the SCIM-SR did not fit the assumptions of the Rasch model in the sub-group of incomplete paraplegia, which may introduce an unknown level of bias in the person estimates. Also, the reliability of the scale as indicated by the PSI was lower in this SCI-specific sub-group than the others, allowing only 2 groups to be distinguished reliably, and the decrease in PSI was most pronounced in the sub-group of persons with incomplete paraplegia (Table IV). Some indications of problems with the SCIM III with respect to high- vs low-ability subjects in the Rasch analysis of the SCIM III (9), and paraplegia vs tetraplegia (10) were also reported in the previous studies of the SCIM III. These issues point more to conceptual challenges on whether functional independence can be assumed to have the same underlying meaning in persons with paraplegia and tetraplegia. We recommend using the transformation Table (Appendix II) of Rasch transformed scores of the SCIM-SR, which are adjusted for SCI-specific sub-groups, to study change over time in people with SCI. Though the extent of bias introduced into the estimates for persons with incomplete paraplegia due to model misfit is unknown, this approach results in a total score on an interval level, which is better suited to monitor the functional independence of people with SCI than the ordinal raw total score. Furthermore, one must also consider the sample sizes available in the study for constructing the transformation tables. The groups of males with non-traumatic complete paraplegia and females with higher age, shorter time since injury, and tetraplegia were rather small (Appendix II); thus, the transformed scores are only provisional. Due to lack of persons achieving a certain score, in particular at the upper end of the continuum of functional independence, the transformed scores are statistical estimates. Further studies are needed with reasonable sample sizes in all sub-groups. Developing a similar scoring scheme for the SCIM III is strongly recommended to ensure that the total score can be used reliably to study change over time. Furthermore, future research should examine further the varying patterns of functioning within and across different SCI sub-groups.
With respect to the distribution of person and items along the continuum of functional independence of the SCIM-SR, some clustering can be observed in the 2 groups of paraplegia and a fairly good distribution along the continuum in the groups of tetraplegia (Fig. 2). In particular, high clustering at the upper end of the continuum, i.e. being functionally independent, is obvious in the group of persons with incomplete paraplegia. Similar observations have been reported for the SCIM III as well as in a very recently developed Greek SCIM III self-report version (31). These findings are contrary to what has been found in the previous Rasch analyses of the SCIM III, where a clustering, in particular for the mobility items, was found at the lower end of the continuum of functional independence (9, 10). This may reflect the different samples, namely inpatient rehabilitation samples at admission in the previous studies vs a community-based sample in the present study. If this interpretation holds, then further research is needed to examine the targeting of the SCIM-SR to enhance its utility along the continuum of care.
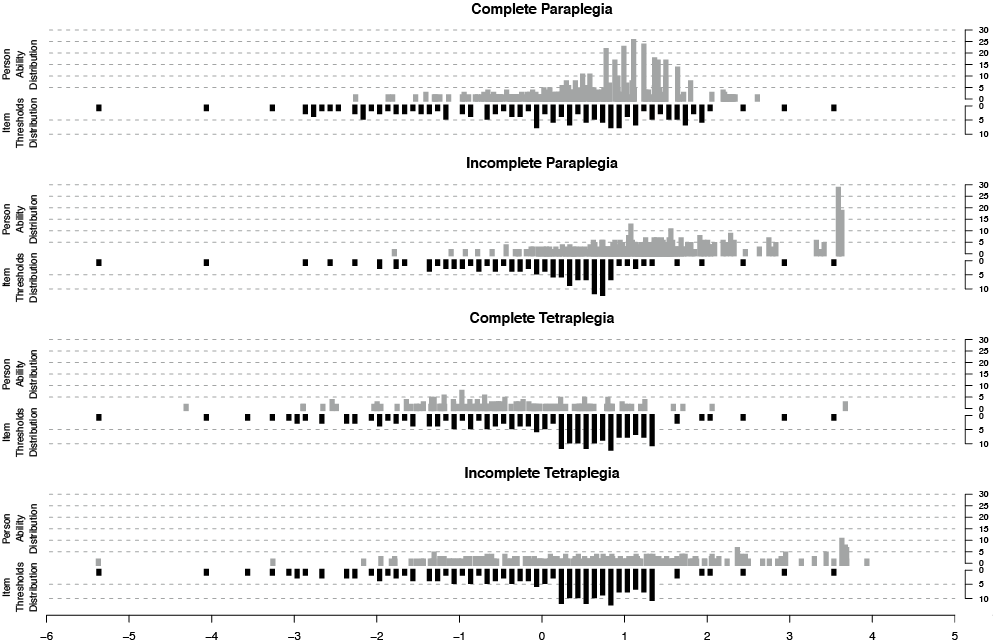
Fig. 2. Distribution of person estimates (upper line) and item estimates (lower line) plotted on the same continuum per spinal cord injury (SCI) sub-group.
To further develop the SCIM III and SCIM-SR, it is also important to examine whether the hierarchical ordering of response options presented in the SCIM has the same meaning for professionals and persons living with SCI. The previous Rasch analyses of the SCIM III have indicated problems with the thresholds (9, 10) even after accommodating some of the issues identified in SCIM II (8). In the Rasch analysis of the mobility sub-scale, for instance, it is assumed that being in a wheelchair reflects more dependency than walking with a walking frame or crutches. From a clinical management point of view this is a valid reasoning. The person living with SCI, however, may prefer to move around in a wheelchair rather than to walk with a walking frame or crutches. In that case, the ordering of the response options is no longer a good estimate of the underlying construct. Similarly, the scoring categories of the bladder and bowel management items reflect only partly an underlying construct of patient’s ability. Therefore, it is not surprising that analyses of the SCIM-III and SCIM-SR reveal problems with fit to the model. The same phenomenon has been described concerning the measurement of participation (32). Conducting cognitive debriefing of both the SCIM III and SCIM-SR would provide further insights into how patients interpret the response options and reveal potential further sources of misfit.
This study has some limitations. All information, including information about SCI characteristics, was self-reported. In particular for lesion level and degree the self-report may not always be in full accordance with a clinician’s characterization of SCI. However, linkage with medical records demonstrated substantial agreement between previously documented and self-reported information (16). Furthermore, anchoring with only one item may weaken the robustness of the anchor design (33). Although this item was a testlet with response options aggregated of 3 items, it is unknown at present if this has an impact on the precision of anchoring.
CONCLUSION
The SCIM-SR violates certain assumptions of the Rasch measurement model, as shown by the local dependency and DIF in our results. Despite this, however, we found an intermediate solution by conducting sub-group analyses and then anchoring these scales on a common testlet to facilitate comparability of persons’ scores across sub-groups. Based on the evidence gained in this study, it is advisable for the time being to use this approach to compute Rasch transformed SCIM-SR scores for the assessment and monitoring of functional independence of persons with SCI.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the support of Veronika Lay and Christine Fekete, PhD (both Swiss Paraplegic Research) for their feedback and support at the early stages of this project. This study was funded by the Swiss Paraplegic Research (SPF), Nottwil, Switzerland.
Appendix I. Detailed item fit statistics, including targeting, unidimensionality, local dependency, and differential item functioning (DIF) for each single Spinal Cord Independence Measure – Self Report (SCIM-SR) item, for Rasch analyses described in Table IV |
|||||||||||||
|
Item split for DIF |
Item difficulty |
|
Item fit |
Uniform differential item functioning (DIF) |
PCA |
|||||||
Location |
SE |
|
FitResid |
Df |
χ2 |
DF |
Prob |
Eigenvalue |
First component |
||||
SwiSCI sample |
|
|
|
|
|
|
|
|
|
|
|
|
|
3 Testlets |
Self-Care |
– |
0.036 |
0.012 |
|
3.530 |
829.73 |
41.542 |
9 |
< 0.001 |
Level, Type |
1.615 |
–0.614 |
|
Sphincter/Respiration |
– |
–0.701 |
0.015 |
|
2.870 |
711.37 |
22.605 |
9 |
0.007 |
|
1.205 |
–0.561 |
|
Mobility |
– |
0.664 |
0.006 |
|
–3.177 |
741.90 |
104.381 |
9 |
< 0.001 |
Level, Type |
0.181 |
0.96 |
Paraplegia |
|
|
|
|
|
|
|
|
|
|
|
|
|
3 Testlets |
Self-Care |
– |
–0.313 |
0.017 |
|
3.838 |
569.29 |
55.283 |
9 |
< 0.001 |
Age, TSI, Complete, Traumatic |
1.644 |
–0.547 |
|
Sphincter/Respiration |
– |
–0.262 |
0.018 |
|
2.669 |
490.98 |
11.987 |
9 |
0.214 |
|
1.134 |
–0.668 |
|
Mobility |
– |
0.575 |
0.007 |
|
–3.819 |
512.73 |
84.124 |
9 |
< 0.001 |
TSI, Complete, Traumatic |
0.222 |
0.948 |
Complete Paraplegia |
|||||||||||||
3 Testlets |
Self-Care |
– |
–0.522 |
0.027 |
|
1.262 |
282.72 |
10.933 |
7 |
0.142 |
|
1.662 |
–0.622 |
|
Sphincter/Respiration |
– |
–0.442 |
0.028 |
|
1.505 |
249.31 |
10.511 |
7 |
0.161 |
|
1.246 |
–0.561 |
|
Mobility |
– |
0.964 |
0.012 |
|
–0.664 |
257.97 |
31.002 |
7 |
> 0.001 |
Gender, Traumatic |
0.092 |
0.980 |
3 Testlets Final* |
Self-Care |
– |
–0.852 |
0.027 |
|
3.306 |
279.85 |
13.883 |
7 |
0.053 |
|
No principal components can be estimated |
|
|
Sphincter/Respiration |
– |
–0.748 |
0.029 |
|
1.493 |
246.79 |
8.743 |
7 |
0.272 |
|
||
|
Mobility |
Female |
0.741 |
0.016 |
|
–1.222 |
61.24 |
11.684 |
7 |
0.111 |
|
||
|
Mobility |
Male Non-Traumatic |
–0.156 |
0.021 |
|
0.427 |
17.76 |
7.428 |
7 |
0.386 |
|
||
|
Mobility |
Male Traumatic |
1.015 |
0.023 |
|
–3.017 |
176.36 |
3.701 |
7 |
0.813 |
|
||
Incomplete Paraplegia |
|||||||||||||
3 Testlets |
Self-Care |
– |
–0.201 |
0.021 |
|
1.634 |
282.57 |
37.593 |
8 |
< 0.001 |
Age, TSI, Traumatic |
1.701 |
–0.411 |
|
Sphincter/Respiration |
– |
–0.158 |
0.024 |
|
2.129 |
238.25 |
7.404 |
8 |
0.494 |
|
1.137 |
–0.783 |
|
Mobility |
– |
0.359 |
0.010 |
|
–3.953 |
251.18 |
33.027 |
8 |
0.000 |
|
0.163 |
0.959 |
3 Testlets Final |
Sphincter/Respiration |
– |
–0.063 |
0.024 |
|
2.304 |
235.30 |
11.268 |
8 |
0.187 |
Traumatic |
No principal components can be estimated |
|
|
Mobility |
– |
0.458 |
0.010 |
|
–3.847 |
248.06 |
35.622 |
8 |
< 0.001 |
|
||
|
Self-Care |
Age 0 |
–0.191 |
0.052 |
|
–0.187 |
72.35 |
11.610 |
8 |
0.169 |
|
||
|
Self-Care |
Age 1 TSI 0 |
–0.084 |
0.031 |
|
1.707 |
114.91 |
28.865 |
8 |
0.000 |
|
||
|
Self-Care |
Age 1 TSI 1 |
–0.120 |
0.038 |
|
0.727 |
89.38 |
21.543 |
8 |
0.006 |
|
||
Tetraplegia |
|
|
|
|
|
|
|
|
|
|
|
|
|
3 Testlets |
Self-Care |
– |
0.305 |
0.019 |
|
0.484 |
250.8 |
16.216 |
7 |
0.023 |
|
1.617 |
–0.688 |
|
Sphincter/Respiration |
– |
–0.999 |
0.026 |
|
1.406 |
212.59 |
6.453 |
7 |
0.488 |
|
1.308 |
–0.430 |
|
Mobility |
– |
0.695 |
0.013 |
|
–0.561 |
220.61 |
17.841 |
7 |
0.013 |
Age, TSI, Complete |
0.075 |
0.979 |
3 Testlets Final |
Self-Care |
– |
–0.080 |
0.019 |
|
0.156 |
245.00 |
8.176 |
7 |
0.317 |
|
No principal components can be estimated |
|
|
Sphincter/Respiration |
– |
–1.399 |
0.027 |
|
1.791 |
207.59 |
5.003 |
7 |
0.660 |
|
||
|
Mobility |
TSI 1 |
0.426 |
0.022 |
|
–0.386 |
108.02 |
7.003 |
7 |
0.429 |
|
||
|
Mobility |
TSI 0 Age 0 |
0.574 |
0.039 |
|
–0.705 |
42.24 |
5.592 |
7 |
0.588 |
|
||
|
Mobility |
TSI 0 Age 1 Female |
0.437 |
0.033 |
|
–1.140 |
16.90 |
2.827 |
6 |
0.830 |
|
||
|
Mobility |
TSI 0 Age 1 Male |
0.042 |
0.034 |
|
0.165 |
45.26 |
4.249 |
7 |
0.751 |
|
||
Appendix I. Contd. |
|||||||||||||
|
Item split for DIF |
Item difficulty |
|
Item fit |
Uniform differential item functioning (DIF) |
PCA |
|||||||
Location |
SE |
|
FitResid |
Df |
χ2 |
Df |
Prob |
Eigenvalue |
First component |
||||
Anchored Analyses: 3 testlets final for Complete Paraplegia* |
|
|
|
|
|
|
|
|
|
|
|
||
3 Testlets Incomplete Paraplegia |
Sphincter/Respiration |
– |
–0.748 |
0.032 |
|
6.810 |
236.53 |
24.205 |
8 |
0.002 |
|
No principal components can be estimated |
|
Mobility |
– |
0.659 |
0.012 |
|
–2.017 |
249.37 |
25.114 |
8 |
0.001 |
|
|||
|
Self-Care |
Age 0 |
–0.253 |
0.059 |
|
0.578 |
72.73 |
12.217 |
8 |
0.142 |
|
||
|
Self-Care |
Age 1 TSI 0 |
–0.054 |
0.037 |
|
3.119 |
115.52 |
33.559 |
8 |
0.000 |
|
||
|
Self-Care |
Age 1 TSI 1 |
–0.176 |
0.044 |
|
1.626 |
89.85 |
22.474 |
8 |
0.004 |
|
||
3 Testlets Tetraplegia |
Self-Care |
– |
–0.027 |
0.023 |
|
2.814 |
246.47 |
7.327 |
7 |
0.396 |
|
No principal components can be estimated |
|
|
Sphincter/Respiration |
– |
–0.748 |
0.034 |
|
5.085 |
208.83 |
33.956 |
7 |
< 0.001 |
|
||
|
Mobility |
TSI 1 |
0.764 |
0.028 |
|
1.266 |
108.67 |
10.761 |
7 |
0.149 |
|
||
|
Mobility |
TSI 0 Age 0 |
1.038 |
0.047 |
|
0.339 |
42.5 |
5.204 |
7 |
0.635 |
|
||
|
Mobility |
TSI 0 Age 1 Female |
0.698 |
0.039 |
|
–0.567 |
17 |
2.949 |
6 |
0.815 |
|
||
|
Mobility |
TSI 0 Age 1 Male |
0.179 |
0.043 |
|
1.180 |
45.53 |
2.552 |
7 |
0.923 |
|
||
Level refers to paraplegia and tetraplegia; degree refers to complete or incomplete lesion; Age 0: Lower age group; Age 1: Higher age group; TSI: time since injury; TSI 0: Less time since injury group; TSI 1: Longer time since injury group; PCA: principal component analysis; FitResid: fit residuals; Df: degrees of freedom; Prob: probability; SE: standard error . |
|||||||||||||
APPENDIX II. Transformation table from the modified raw scores into user-friendly, unbiased, interval-scaled 0–100 metric |
||||||||||||
Subgroups Modified Raw Score |
Complete Paraplegia |
|
Incomplete Paraplegia |
|
Tetraplegia |
|||||||
Female 0–100 Score |
Male non-traumatic 0–100 Score |
Male traumatic injury 0–100 Score |
|
Age = 0 0–100 Score |
Age = 1 TSI = 0 0–100 Score |
Age = 1 TSI = 1 0–100 Score |
|
TSI = 1 0–100 Score |
Age = 0 TSI = 0 0–100 Score |
Age = 1 TSI = 0 Female 0–100 Score |
Age = 1 TSI = 0 Male 0–100 Score |
|
n in Rasch analysis |
98 |
26 |
282 |
|
119 |
189 |
147 |
|
179 |
70 |
28 |
75 |
0 |
0.0 |
0.0 |
0.0 |
|
0.0 |
0.0 |
0.0 |
|
0.0 |
0.0 |
0.0 |
0.0 |
1 |
13.8 |
13.6 |
15.2 |
|
14.0 |
13.9 |
14.0 |
|
13.9 |
13.9 |
13.4 |
14.0 |
2 |
23.2 |
22.7 |
25.6 |
|
24.8 |
24.6 |
24.6 |
|
24.4 |
24.5 |
23.2 |
24.6 |
3 |
29.8 |
28.7 |
32.7 |
|
33.2 |
32.7 |
32.6 |
|
32.3 |
32.4 |
30.3 |
32.8 |
4 |
34.4 |
33.0 |
37.8 |
|
39.1 |
38.5 |
38.3 |
|
37.7 |
37.8 |
35.4 |
38.5 |
5 |
38.0 |
36.4 |
41.7 |
|
43.2 |
42.5 |
42.3 |
|
41.6 |
41.6 |
39.2 |
42.2 |
6 |
41.0 |
39.1 |
44.9 |
|
46.1 |
45.4 |
45.3 |
|
44.4 |
44.4 |
42.2 |
44.9 |
7 |
43.6 |
41.5 |
47.6 |
|
48.3 |
47.7 |
47.6 |
|
46.7 |
46.5 |
44.7 |
46.9 |
8 |
45.9 |
43.6 |
49.9 |
|
50.0 |
49.6 |
49.5 |
|
48.5 |
48.3 |
46.8 |
48.5 |
9 |
47.9 |
45.6 |
51.9 |
|
51.5 |
51.2 |
51.1 |
|
50.1 |
49.8 |
48.7 |
49.8 |
10 |
49.6 |
47.4 |
53.6 |
|
52.7 |
52.6 |
52.6 |
|
51.5 |
51.2 |
50.2 |
51.0 |
11 |
51.1 |
49.2 |
55.0 |
|
53.8 |
53.8 |
53.9 |
|
52.8 |
52.4 |
51.6 |
52.0 |
12 |
52.4 |
50.8 |
56.3 |
|
54.8 |
55.0 |
55.0 |
|
53.9 |
53.5 |
52.8 |
53.0 |
13 |
53.6 |
52.3 |
57.4 |
|
55.7 |
56.1 |
56.2 |
|
55.0 |
54.6 |
54.0 |
53.9 |
14 |
54.7 |
53.8 |
58.5 |
|
56.6 |
57.1 |
57.2 |
|
55.9 |
55.5 |
55.0 |
54.7 |
15 |
55.6 |
55.2 |
59.5 |
|
57.4 |
58.0 |
58.2 |
|
56.9 |
56.4 |
56.0 |
55.5 |
16 |
56.5 |
56.5 |
60.4 |
|
58.2 |
58.9 |
59.1 |
|
57.7 |
57.3 |
56.9 |
56.3 |
17 |
57.4 |
57.7 |
61.4 |
|
58.9 |
59.8 |
59.9 |
|
58.6 |
58.1 |
57.7 |
57.0 |
18 |
58.2 |
58.8 |
62.3 |
|
59.6 |
60.5 |
60.8 |
|
59.4 |
58.9 |
58.6 |
57.7 |
19 |
58.9 |
59.9 |
63.2 |
|
60.4 |
61.3 |
61.5 |
|
60.1 |
59.7 |
59.4 |
58.3 |
20 |
59.7 |
61.0 |
64.1 |
|
61.0 |
62.0 |
62.2 |
|
60.9 |
60.5 |
60.2 |
59.0 |
21 |
60.4 |
61.9 |
65.0 |
|
61.7 |
62.7 |
62.9 |
|
61.6 |
61.2 |
60.9 |
59.6 |
22 |
61.1 |
62.8 |
65.8 |
|
62.4 |
63.3 |
63.5 |
|
62.3 |
61.9 |
61.6 |
60.2 |
23 |
61.7 |
63.7 |
66.6 |
|
63.0 |
63.9 |
64.0 |
|
63.0 |
62.6 |
62.3 |
60.8 |
24 |
62.4 |
64.5 |
67.4 |
|
63.6 |
64.5 |
64.5 |
|
63.6 |
63.2 |
63.0 |
61.4 |
25 |
63.0 |
65.2 |
68.2 |
|
64.2 |
65.0 |
64.9 |
|
64.3 |
63.9 |
63.7 |
61.9 |
26 |
63.7 |
65.9 |
68.9 |
|
64.8 |
65.5 |
65.4 |
|
64.9 |
64.5 |
64.3 |
62.5 |
27 |
64.3 |
66.7 |
69.7 |
|
65.3 |
66.0 |
65.8 |
|
65.5 |
65.2 |
64.9 |
63.0 |
28 |
64.9 |
67.4 |
70.4 |
|
65.8 |
66.5 |
66.2 |
|
66.1 |
65.8 |
65.5 |
63.5 |
29 |
65.5 |
68.0 |
71.1 |
|
66.3 |
66.9 |
66.5 |
|
66.7 |
66.4 |
66.1 |
64.0 |
30 |
66.2 |
68.7 |
71.8 |
|
66.8 |
67.4 |
66.9 |
|
67.2 |
67.0 |
66.7 |
64.5 |
31 |
66.8 |
69.4 |
72.5 |
|
67.3 |
67.8 |
67.2 |
|
67.8 |
67.5 |
67.3 |
65.0 |
32 |
67.5 |
70.0 |
73.3 |
|
67.7 |
68.2 |
67.6 |
|
68.4 |
68.1 |
67.9 |
65.5 |
33 |
68.1 |
70.7 |
74.0 |
|
68.1 |
68.6 |
68.0 |
|
68.9 |
68.7 |
68.5 |
65.9 |
34 |
68.8 |
71.4 |
74.7 |
|
68.5 |
69.1 |
68.4 |
|
69.5 |
69.2 |
69.0 |
66.4 |
35 |
69.5 |
72.2 |
75.5 |
|
68.9 |
69.5 |
68.8 |
|
70.0 |
69.8 |
69.6 |
66.8 |
36 |
70.2 |
73.9 |
76.3 |
|
69.4 |
69.9 |
69.2 |
|
70.5 |
70.4 |
70.3 |
67.2 |
37 |
71.0 |
74.8 |
77.1 |
|
69.8 |
70.4 |
69.6 |
|
71.1 |
70.9 |
71.3 |
67.6 |
38 |
71.8 |
74.9 |
78.0 |
|
70.2 |
70.9 |
70.1 |
|
71.6 |
71.5 |
72.0 |
68.1 |
39 |
72.6 |
74.9 |
78.8 |
|
70.7 |
71.3 |
70.6 |
|
72.1 |
72.0 |
72.3 |
68.5 |
40 |
73.5 |
75.0 |
79.8 |
|
71.1 |
71.8 |
71.2 |
|
72.7 |
72.6 |
72.5 |
68.9 |
41 |
74.4 |
75.0 |
80.7 |
|
71.6 |
72.3 |
71.7 |
|
73.2 |
73.2 |
72.7 |
69.3 |
42 |
75.3 |
75.1 |
81.8 |
|
72.1 |
72.8 |
72.3 |
|
73.7 |
73.8 |
72.8 |
69.6 |
43 |
76.3 |
75.1 |
82.8 |
|
72.7 |
73.3 |
72.9 |
|
74.3 |
74.5 |
73.0 |
70.0 |
44 |
77.4 |
75.1 |
84.0 |
|
73.3 |
73.8 |
73.5 |
|
74.8 |
75.1 |
73.1 |
70.4 |
45 |
79.6 |
75.2 |
85.2 |
|
73.9 |
74.3 |
74.1 |
|
75.4 |
75.8 |
73.2 |
70.8 |
46 |
81.1 |
75.2 |
86.4 |
|
74.4 |
74.8 |
74.6 |
|
75.9 |
76.5 |
73.2 |
71.1 |
47 |
81.1 |
75.3 |
87.8 |
|
75.0 |
75.3 |
75.2 |
|
76.4 |
77.2 |
73.3 |
71.5 |
48 |
81.2 |
75.3 |
89.2 |
|
75.5 |
75.7 |
75.6 |
|
76.9 |
77.9 |
73.4 |
71.9 |
49 |
81.2 |
75.3 |
90.6 |
|
76.0 |
76.1 |
76.1 |
|
77.3 |
78.7 |
73.5 |
72.2 |
50 |
81.2 |
75.4 |
92.2 |
|
76.4 |
76.4 |
76.4 |
|
77.7 |
79.4 |
73.6 |
72.6 |
51 |
81.3 |
75.4 |
93.9 |
|
76.7 |
76.7 |
76.8 |
|
78.0 |
80.2 |
73.7 |
72.9 |
52 |
81.4 |
75.5 |
98.1 |
|
77.0 |
76.9 |
77.0 |
|
78.3 |
81.0 |
73.8 |
73.3 |
53 |
81.4 |
75.6 |
98.2 |
|
77.3 |
77.2 |
77.3 |
|
78.5 |
81.7 |
73.8 |
73.6 |
54 |
81.5 |
75.6 |
98.3 |
|
77.5 |
77.4 |
77.5 |
|
78.7 |
82.4 |
73.9 |
74.0 |
55 |
81.5 |
75.6 |
98.4 |
|
77.7 |
77.6 |
77.7 |
|
79.0 |
83.1 |
74.0 |
74.3 |
56 |
81.5 |
75.6 |
98.5 |
|
77.9 |
77.8 |
77.9 |
|
79.2 |
83.7 |
74.1 |
74.7 |

APPENDIX II. Contd. |
||||||||||||
Subgroups Modified Raw Score |
Complete Paraplegia |
|
Incomplete Paraplegia |
|
Tetraplegia |
|||||||
Female 0–100 Score |
Male non-traumatic 0–100 Score |
Male traumatic injury 0–100 Score |
|
Age = 0 0–100 Score |
Age = 1 TSI = 0 0–100 Score |
Age = 1 TSI = 1 0–100 Score |
|
TSI = 1 0–100 Score |
Age = 0 TSI = 0 0–100 Score |
Age = 1 TSI = 0 Female 0–100 Score |
Age = 1 TSI = 0 Male 0–100 Score |
|
57 |
81.6 |
75.7 |
98.5 |
|
78.1 |
78.0 |
78.1 |
|
79.4 |
84.3 |
74.2 |
75.1 |
58 |
81.6 |
75.8 |
98.6 |
|
78.3 |
78.2 |
78.3 |
|
79.6 |
84.7 |
74.3 |
75.4 |
59 |
81.6 |
75.8 |
98.7 |
|
78.5 |
78.3 |
78.5 |
|
79.7 |
85.2 |
74.4 |
75.8 |
60 |
81.8 |
75.9 |
98.8 |
|
78.7 |
78.6 |
78.7 |
|
80.0 |
85.5 |
74.5 |
76.2 |
61 |
81.8 |
75.9 |
98.9 |
|
78.9 |
78.7 |
78.9 |
|
80.1 |
85.9 |
74.7 |
76.6 |
62 |
81.8 |
75.9 |
98.9 |
|
79.1 |
79.0 |
79.1 |
|
80.3 |
86.2 |
74.9 |
77.0 |
63 |
81.8 |
75.9 |
99.0 |
|
79.3 |
79.2 |
79.3 |
|
80.6 |
86.5 |
75.2 |
77.5 |
64 |
81.9 |
76.1 |
99.1 |
|
79.5 |
79.4 |
79.5 |
|
80.8 |
86.8 |
75.7 |
77.9 |
65 |
81.9 |
76.1 |
99.1 |
|
79.8 |
79.6 |
79.8 |
|
81.0 |
87.1 |
77.4 |
78.5 |
66 |
81.9 |
76.1 |
99.2 |
|
80.1 |
80.0 |
80.1 |
|
81.3 |
87.4 |
78.6 |
79.1 |
67 |
82.0 |
78.3 |
99.2 |
|
80.4 |
80.3 |
80.4 |
|
81.7 |
87.7 |
79.8 |
79.8 |
68 |
82.0 |
80.9 |
99.4 |
|
80.8 |
80.8 |
80.9 |
|
82.1 |
88.0 |
81.1 |
80.6 |
69 |
82.1 |
83.1 |
99.4 |
|
81.4 |
81.5 |
81.5 |
|
82.8 |
88.4 |
82.6 |
81.7 |
70 |
82.2 |
85.4 |
99.6 |
|
82.2 |
82.6 |
82.5 |
|
83.7 |
88.9 |
84.4 |
83.1 |
71 |
82.2 |
88.9 |
99.6 |
|
84.0 |
84.5 |
84.3 |
|
85.3 |
89.5 |
86.5 |
85.0 |
72 |
82.2 |
92.4 |
99.6 |
|
87.0 |
87.6 |
87.4 |
|
88.0 |
90.5 |
89.4 |
87.9 |
73 |
92.8 |
98.0 |
99.8 |
|
91.9 |
92.4 |
92.3 |
|
92.5 |
93.1 |
93.6 |
92.6 |
74 |
100.0 |
100.0 |
100.0 |
|
100.0 |
100.0 |
100.0 |
|
100.0 |
100.0 |
100.0 |
100.0 |
Age 0: Lower age group; Age 1: Higher age group; TSI 0: Less time since injury group; TSI 1: Longer time since injury group; n: Number of people included in sub-group specific analysis. |
||||||||||||
REFERENCES
