Sara Moreno1*#, Xavier Soria1*#, Montserrat Martínez2, Rosa M. Martí1*& and Josep M. Casanova1*&
1Department of Dermatology, Hospital Universitari Arnau de Vilanova, Universitat de Lleida, and 2Department of Statistics, IRB Lleida, Spain
*These authors contributed equally and should be considered as first authors#and as co-senior author&, respectively
The worldwide incidence of malignant melanoma is increasing. The number of pigmented naevi and amount of solar exposure are important risk factors. The aim of this study was to characterize a paediatric population (from Lleida, Catalonia, Spain) in terms of phenotype, sun behaviour and naevi prevalence. Data on the numbers and distributions of acquired naevi in 369 children, aged 4, 8 and 14 years, were collected and correlated with age, sex, skin phototype and environmental factors (annual/lifetime intermittent and chronic sun exposure, sunburns and sunscreen use). The density of naevi increased with age. Boys had more naevi on the trunk and girls had more naevi on the legs. Children with light skin phototype had more naevi. A higher level of accumulated sun exposure correlated with a higher number of naevi in children with non-adequate sunscreen use. In conclusion, several risk factors associated with naevi density and distribution were found, as previously reported by others. Multivariate analysis confirmed a protective role of sunscreen in the development of acquired melanocytic naevi. Key words: childhood; risk factors; skin photoprotection.
Accepted Oct 29, 2015; Epub ahead of print Nov 9, 2015
Acta Derm Venereol 2015; XX: XX–XX.
Sara Moreno, Department of Dermatology, Hospital Universitari Arnau de Vilanova, Avda. Alcalde Rovira Roure 80, ES-25198 Lleida, Spain. E-mail: saramoreno.derma@gmail.com
Malignant melanoma is becoming an important problem in public health; incidence rates have been increasing continuously in the Caucasian population worldwide (1–3).
Epidemiological research has consistently shown that the presence of many melanocytic naevi on the skin is the major determinant of melanoma. Childhood and adolescence are an important time of life for the development and evolution of naevi, and the presence of a higher number of naevi in early life could predict a major risk of developing melanoma (4–9). There is also a site-specific risk relationship; a high density of naevi in a specific anatomical region implies an increased risk of developing melanoma in that region (9, 10). Furthermore, an atypical distribution pattern of naevi and the presence of atypical/dysplastic moles have been shown to be useful variables for identifying patients at risk of developing melanoma (9, 11, 12).
Although numerous studies have identified a range of possible risk factors for the development of naevi, there is poor agreement about which of these are materially involved (4). Constitutional factors suggested by some studies include being male, older, of European ethnicity, having pale skin, light-coloured eyes and fair hair, heavy freckling and having skin that burns after sun exposure (13). The relationship between sun exposure and naevi counts is also controversial; although several studies have indicated this association (14, 15), others have found that the prevalence of melanocytic naevi is not related to ultraviolet (UV) exposure (4).
The aims of this study are to investigate the presence, density and regional distribution of acquired melanocytic naevi among a paediatric population and to assess the associated constitutional and environmental factors. The primary research question is to establish the relationship between sun exposure habits and constitutional factors and the number and distribution of naevi. Secondary research questions are the characterization of the paediatric population in terms of sun exposure habits, constitutional factors and naevi prevalence. With these aims, unlike other studies, we explored children in 3 different age groups (4, 8 and 14 years) in order to measure differences in the number of naevi with maximum precision, avoiding variability due to age. This study confirms the importance of several previously described risk factors associated with naevi development (age, sex, phototype and sun exposure) and emphasizes the controversial protective role of sunscreens for the development of acquired naevi.
METHODS
A cross-sectional study was designed. The study population comprised children aged 4, 8 and 14 years living in the city of Lleida, Catalonia, Spain, or closely surrounding towns and villages. Children were recruited by their primary care paediatricians when they attended a routine healthy child programme medical review. The study was conducted from April 2007 to September 2008.
Twenty primary care paediatricians were involved in the study. A training course was conducted before the start of data recording. One hundred clinical images of melanocytic naevi (common, congenital, atypical, blue and halo naevi) were shown to paediatricians and discussed.
On the same day as the healthy child medical review, the paediatrician completed a questionnaire with the children’s parents (for children aged 4 and 8 years) or with both children and parents (for 14-year-old children). They were asked about the number of hours of sun exposure, tanning ability, skin phototype, number of sunburns and use of sunscreens (see Appendix S11). Hair and eye colour were recorded. Parents were informed about the study and their consent requested.
Naevi counts
Acquired melanocytic naevi were defined as non-congenital brown-to-black pigmented macules or papules ≥ 2 mm in diameter occurring on the skin. A naevus was defined as atypical if larger than 5 mm with an irregular border and/or irregular pigmentation. Congenital naevi and blue naevi were excluded. To avoid any confusion between naevi and freckles, only naevi with a diameter > 2 mm were considered. Macular lesions located in photo-exposed areas with a tendency to confluence and fading during the winter were considered freckles (16). No attempt was made to differentiate lentigo simple from junctional melanocytic naevi.
On the day of the survey the paediatrician examined the children’s skin for acquired melanocytic naevi and recorded their size. Examination of the scalp was excluded. The naevi 2–4.9 mm in diameter were noted with a plus sign (+) on a schematic figure included in the survey. The naevi ≥ 5 mm were noted with a circle (o) and atypical naevi with a square (□). All children with atypical naevi or with equivocal lesions were re-evaluated at the Department of Dermatology of Hospital Universitari Arnau de Vilanova (Lleida, Spain). A monthly meeting with primary care paediatricians was held to discuss the cases that emerged.
Statistical analysis
The description of each group of children included median plus interquartile range (or mean and standard deviation) and frequencies, for quantitative and qualitative variables, respectively.
Presence of any melanocytic naevi (i.e. excluding atypical naevi because their number was extremely low in all cohorts, < 1) was analysed by anatomical site and age. Differences in each anatomical site by age were assessed using χ2 test (or Fisher’s exact test in the presence of any expected frequency lower than 5), and if significant, odds ratio (OR) and its 95% confidence intervals (CI) were estimated to compare age groups (8- vs. 4- and 14- vs. 8-year-old children, plus, in case of no significance, OR from 14- vs. 4-year-old children). The same analysis was used to check differences in sunscreen use. Mann-Whitney test (and t-test if the normality assumption was acceptable) was used to assess differences in the number of melanocytic naevi between boys and girls by anatomical site and age.
Due to the presence of over-dispersion, negative-binomial multivariate regression models were fit to the number of melanocytic naevi in each age group, adjusted by sex, skin type (I–II vs. III–IV), sunscreen use, and accumulated sun exposure outdoors and at the beach or pool. The exponential of the coefficients and their 95% CI were also provided. Possible confounding (changes > 20%) and interaction effects between explanatory variables were checked, stratifying the analysis in the case of significant interactions.
RESULTS
During the study, 369 children were examined from April 2007 to September 2008. Demographic and clinical characteristics of the study population are shown in Table I.
Table I. Demographic and clinical characteristics of the study population (n = 369)
|
Variable |
4 years n = 182 |
8 years n = 125 |
14 years n = 62 |
|
Caucasian, n (%) |
170 (93.4) |
116 (92.8) |
61 (96.8) |
|
Sex, n (%) |
|||
|
Male |
97 (53.3) |
59 (47.2) |
32 (50.8) |
|
Female |
85 (46.7) |
66 (52.8) |
30 (49.2) |
|
Naevus, median (IQR) [min–max] |
|||
|
Overall |
1 (3) [0–17] |
5 (7) [0–40] |
10 (20) [0–84] |
|
≥ 5 mm |
0 (0) [0–2] |
0 (0) [0–3] |
0 (0) [0–8] |
|
Atypical |
0 (0) [0–4] |
0 (0) [0–1] |
0 (0) [0–1] |
|
Eye colour, n (%) |
|||
|
Light |
34 (18.7) |
21 (16.8) |
15 (23.8) |
|
Dark |
148 (81.3) |
104 (83.2) |
48 (76.2) |
|
Hair colour, n (%) |
|||
|
Fair/red |
93 (51.1) |
51 (40.8) |
22 (34.9) |
|
Dark |
89 (48.9) |
74 (59.2) |
41 (65.1) |
|
Skin type, n (%) |
|||
|
I–II |
22 (12.1) |
17 (13.6) |
15 (23.8) |
|
III–IV |
160 (87.9) |
108 (86.4) |
47 (76.2) |
|
Sun exposure |
|||
|
Accumulated (lifetime), h, median (IQR) [min–max] |
1,344 (982) [48–5,232] |
3,192 (2,068) [686–10,098] |
5,530 (3,796) [946–18,340] |
|
Hours at beach/pool, %, median (IQR) [min–max] |
19.1 (21.0) [0–100.0] |
24.3 (19.0) [0–65.6] |
24.5 (20.6) [2.9–54.8] |
|
Mean h/year (SD) |
387.6 (223.4) |
450.8 (217.8) |
456.5 (242.4) |
|
Sunscreen use, n (%) |
|||
|
Every 2 h |
119 (65.4) |
69 (55.2) |
26 (41.3) |
|
SPF ≥15 |
155 (85.2) |
102 (81.6) |
55 (87.3) |
|
Every 2 h and SPF ≥ 15 |
106 (58.2) |
60 (48) |
24 (38.7) |
|
Number of sunburns, n (%) |
|||
|
Mild–moderate |
7 (3.8) |
8 (6.4) |
22 (33.9) |
|
Severe (blisters) |
2 (1.1) |
0 (0) |
2 (3.2) |
SPF: sun protection factor; SD: standard deviation.
Results related to the characterization of our paediatric population in terms of naevus prevalence, sun exposure habits and constitutional factors are described below.
Total body naevi counts and regional naevi distribution
The median number of naevi for all groups was 6 (range 0–84). Distribution by age, number of large naevi and atypical naevi are shown in Table I. In summary, the number of atypical naevi and naevi > 5 mm was low for the 3 age groups, with a median number less than one in all cohorts.
The body distribution of the naevi in the study population was as follows: 106 children had naevi on the head, 241 on the trunk, 27 on the swimwear-covered area, 108 on the arms, 10 on the hands, 117 on the legs and 14 on the feet (Table SI1).
When the density of naevi (number of naevi/site) was analysed within each age group, significant differences were observed in naevi distribution between the regions; i.e. we found at least one zone with a density of naevi statistically different from the others. Remarkably, the trunk was the anatomical site where naevi were most common and the site that showed a more rapid increase in the number of naevi with age (Fig. S11).
When the density of naevi (number of naevi/site) was analysed within each site, looking for differences between the different age groups, we found significant differences on the head, trunk, arms and legs, which showed an increasing number of naevi with age (Table SII1).
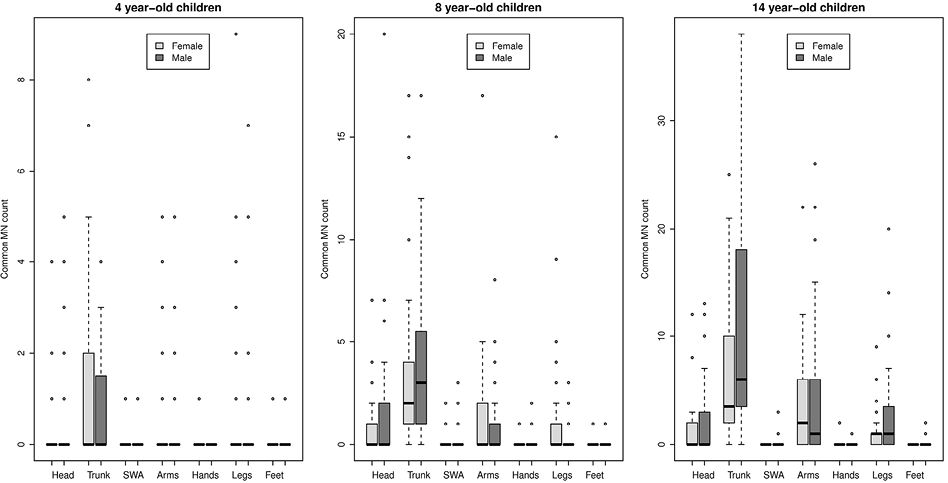
Fig. 1 (and Table SIII1) show median and mean naevus counts for each anatomical site stratified by age and sex. Statistical analysis showed significant differences in naevi distribution only in the group of girls aged 8 years who had a higher number of naevi on their legs.
Use of sunscreen and sun exposure
Concerning sun blockers and considering both groups (regardless of the sun protection factor (SPF) applied and whether they were reapplied every 2 h or specified as “using a sun blocker with SPF ≥ 15 and reapplication every 2 h”) a decreasing trend in sunscreen use with age was observed. Significant differences in the use of sunscreen outdoors and at beaches and pools were found between the 3 age groups (Table SIV1).
Total (lifetime) sun exposure and mean annual hours of total sun exposure are shown in Table I. The percentage of lifetime sun exposure at the beach/pool was 19.1% in the 4-year-old group, 24.3% in the 8-year-old group, and 24.5% in the 14-year-old group.
Naevi counts in relation to skin phototype and sunburns
Bivariate analysis showed statistically significant differences in total naevi count between light (I–II) and dark (III–IV) skin type groups in 4- and 14-year-old children (p < 0.05), with a higher number of naevi in light phototypes (data not shown). Taking into account naevus size, distribution of small naevi (2–4.9 mm) presented the same significant differences as those observed on the global group (p < 0.05). This finding can be explained by the very low number of large naevi seen in the sample.
The number of sunburns and the distribution between mild–moderate (erythema) and severe sunburns (erythema and blisters) is shown in Table I. Although no significant correlation between having had sunburns and the number of naevi was observed (except in the 14-year-old group), a trend to an increasing naevi count related to the number of sunburns was shown in all age groups (data not shown).
Multivariate analysis
With the aim of explaining the relationship between the number of naevi and the remaining variables, and because data showed over-dispersion, a regression model based on negative binomial distribution was applied. Independent variables were: sex (male), skin phototype I and II, total number of hours of sun exposure, number of hours at the beach/pool and number of hours outdoors, history of sunburns, common use of sunscreen and correct use of sunscreen (Tables II and SV1).
Table II. Multivariate analysis of factors associated with melanocytic naevi count in the sample of 4-, 8- and 14-year-old children: statistical significance, represented by p-value
|
Variable |
Negative binomial GLM by age group |
||
|
4 years |
8 years |
14 years |
|
|
Sex, male |
0.212 |
0.149 |
0.003 |
|
Skin type I–II vs. III–IV |
0.097 |
0.573 |
< 0.001 |
|
Accumulated sun exposure outdoors |
0.019 |
0.472 |
0.834 |
|
Accumulated sun exposure at beach/pool (”A”) |
0.673 |
0.011 |
0.001 |
|
Sunscreen usea at beach/pool (”B”) |
0.924 |
0.568 |
0.005 |
|
Interaction of ”A” and ”B” |
0.476 |
0.210 |
0.027 |
aSunscreen use is defined as: use of SPF>15 and reapplication every 2 h.
Adjusted p-values for the multivariate regression model for the count of melanocytic naevi for children in each age group. Sunburns did not show a significant contribution to any of the models and therefore were not included. Significant values (p < 0.05) are shown in bold.
GLM: generalized linear models.
Four-year-old group. The only variable associated with the number of naevi was total hours of sun exposure. Nevertheless, this association was related only to the number of hours spent outdoors and not to sun exposure at beaches and pools. Therefore, a greater number of hours spent outdoors (excluding time spent on beach/pool) was associated with a greater number of naevi in the 4-year-old group.
Eight-year-old group. The only variable associated with number of naevi was total hours of sun exposure. Nevertheless, this association was related only to the number of hours spent at beaches and pools and not to outdoor sun exposure. Therefore, a greater number of hours spent at beaches and pools was associated with a greater number of naevi in the 8-year-old group.
Fourteen-year-old group. The total accumulated hours of sun exposure, skin phototype (I and II) and sex (male) were variables that explained a significant part of the variability observed in number of naevi in 14-year-old children. Once again, the association of number of naevi with total sun exposure was only due to the number of hours spent at beaches and pools and not to outdoor sun exposure, as in the 8-year-old-group.
With regard to the remaining variables, the use of sunscreen showed a bivariate statistically significant association with the number of naevi, which disappeared when it was adjusted for other variables in the multivariate analysis. Indeed, the number of hours of accumulated sun exposure at the beach/pool has a significant association with the number of naevi, depending on the correct use of sunscreen, meaning that there is a significant interaction. Stratified results by sunscreen use adjusted by sex and skin type (I–II vs. III–IV) showed that more sun exposure at the beach/pool was associated with more melanocytic naevi only for children with non-adequate sunscreen use (Table SV1).
DISCUSSION
The increasing trend in melanoma rates worldwide is reflected in a recently published multicentre study reporting melanoma patients diagnosed at 23 different Catalan hospitals, during the period 2000 to 2007 (17). Our centre is the main hospital of the area of Lleida, Catalonia, Spain and covers a population of approximately 450,000 inhabitants.
The median numbers of naevi in children aged 4, 8 and 14 years from our geographical area were 1, 5 and 10, respectively. The phenomenon of new naevi development during childhood and adolescence has been previously well established (18–22). Comparing our results with those of other studies conducted in Mediterranean countries located at a similar latitude, we could observe the following: (i) in a study of Italian children (23), a median of 11 naevi among children aged 13–14 years was noted; (ii) in a study conducted in Turkey (24) the mean number of naevi was 6.53 in children aged 0–16 years; (iii) Aguilera et al. (4) reported a mean of 17.5 naevi among children from Barcelona (Catalonia, Spain) aged 1–15 years. They found a higher number of naevi than our study and other studies. This could be due to the fact that moles of < 2 mm diameter were included in Aguilera’s study. (iv) In a recent study carried out in Granada a mean naevi count of 19.38 was observed among 8–10-year-old children, which is higher than the mean of 5 naevi seen in our 8-year-old group. This result could again be attributed to the inclusion of naevi < 2 mm diameter (25).
Comparing our results with those studies conducted in countries at different latitudes, we observed a lower number of naevi compared with children of similar age. (v) Australian children aged 3 years (8) presented a median of 10 naevi, which is higher than the median of our 4-year-old group (1 naevi). We noted a median of 5 naevi in our 8-year-old group. Comparing children from different Australian regions and from Scotland, Whiteman et al. (8) noted the existence of an inverse association between latitude and naevi number, lending further support to the notion that ambient sun exposure plays a key role in melanocytic proliferation in very early childhood. However, Synnerstad et al. (9) from Sweden, reported a median of 8 naevi in children aged 8–9 years, suggesting that, besides the sun exposure pattern, other factors, such as phenotype, may play a role.
Sex variations in naevi density, with higher numbers of naevi in boys compared with girls, have been documented repeatedly (6, 26, 27). Even if discrepant data exist (14), these results could be explained by a potential role for growth and sex hormones in naevi development (4, 28). In our series, being male was an independent factor for greater number of naevi (p = 0.02) only in the 14-year-old group. As shown in Table SIII1, given the other variables are held constant, a 14-year-old boy had twice the number of melanocytic naevi compared with a girl. The fact that differences between sex are observed only at the age of 14 years could be explained by a stronger statistical power related to the higher number of naevi seen at that age and/or due to changes secondary to hormonal influence.
Regarding body distribution, naevi were more frequently present on the trunk, followed by the legs, arms, head, swimwear area and feet and hands. This is consistent with the distribution of naevi (29, 30) and melanoma in adults among the Spanish population (31). Such naevi distribution was seen in all age groups, although in younger children they were seen only on the trunk. Adolescents show a similar distribution to adults; more naevi on the trunk, followed by limbs (arms and legs). The number of naevi was extremely low on the swimwear area, hands and feet in all groups. We found significant differences in the density of naevi in intermittently sun-exposed areas (trunk, legs and arms). On the other hand, we did not obtain statistical differences in non-sun exposed areas (swimwear area and feet). Findings in chronic sun-exposed areas are more difficult to explain (significance differences in density of naevi on the head but not on the hands). Perhaps the behaviour of the chronically exposed areas is related more to the biological characteristics of the skin in these regions than to the influence of sun exposure. Indeed, melanomas arising on the hands and feet share common epidemiological and clinical features and are not related to sun exposure, whereas melanomas on the head are epidemiologically and clinically different and are related to chronic sun exposure (32). This hypothesis has been put forward previously by other authors, based on epidemiological and mice experimental studies (8).
Regional distribution of naevi and cutaneous malignant melanoma show different patterns in adult men and women. Men have more naevi and melanoma on the trunk, while women have more naevi and melanoma on the legs (11). In agreement with these, and with data from previous studies of naevi distribution in children (9, 14), we found statistically significant differences in naevi counts on the legs between the 2 sexes, with girls having higher naevi counts than boys in that region. Furthermore, we observed a trend to a higher number of naevi on the trunk in boys. Once again, growth and sex hormones affecting the sexes differently might be of importance for naevi development.
We found a significant association between lighter skin type (I–II) and higher number of naevi, again only in the group of 14 years (p = 0.0002) as an independent variable. For instance, as shown in Table SIII1, given the other variables are held constant, a 14-year-old child with skin type I or II showed a number of melanocytic naevi approximately 2.5 times greater than others with skin type III or IV. The association of skin type with the number of naevi is controversial. Some studies in adults have shown an association between dark skin and a greater number of naevi (32), while other observational studies have shown the same association with fair skin (33, 34).
Topographic variability in the density of naevi, with higher number of naevi in sun-exposed areas, seen in many studies as well as ours, supports the association of both chronic and intermittent UV exposure with naevi development (14, 15). In our series, multivariate analysis showed differences in the number of naevi in relation to the number of hours of sun exposure in the 3 age groups. For children under 4 years, only outdoors sun exposure (excluding time spent at the beach/pool) was significant (p = 0.01), perhaps because of avoidance of sun exposure at beaches and pools due to parents’ awareness. In the groups aged 8 and 14 years, sun exposure at beaches and pools was identified as an independent factor (with p-values of 0.02 and 0.01, respectively). Moreover, in the 14-year-old group, sunscreen use modified the effect of lifetime sun exposure on total naevus count, with a higher number of naevi observed in children with non-adequate sunscreen use (Tables II and SV1). In summary, the results of the current study confirm the influence of total sun exposure on naevus development and the protective role of sunscreen.
Concerning the use of sunscreen, a decrease in use was observed with age, with statistically significant differences between the 14- vs. the 8- and 4-year-old groups or between the 14- and 8- vs. the 4-year-old groups, depending on the method of evaluation of sunscreen use (always vs. almost, always/almost at the beach/pool, always/almost SPF ≥ 15 and every 2 h, etc.). We believe that this could be explained because older children are less likely to apply sunscreen and are less controlled by their parents. In fact, in a study conducted in 2004 in our region (34), we observed that only 14.6% of our general population used sunscreen properly. If we compare this result with that obtained in the current study (47.8%), we found a clearly higher percentage of correct use of sunscreen among children. There are 2 explanations for these differences. First, the subjects in the current study are children who are under their parent’s care and our previous study referred to adults (older than 50 years). Secondly, this could reflect the success of skin cancer prevention campaigns conducted in our country in recent years.
The relationship between the use of sunscreen and the number of naevi is also controversial. Regular use of sunscreen has been associated with a lower number of naevi in children in a randomized study (14, 35) and in some observational studies. Nevertheless, other studies have shown an association between sunscreen use and an increased number of naevi (36, 37). The authors suggested that the use of sunscreen gives parents a false sense of security and leads to children being exposed to the sun for longer. However, as already mentioned, in our study, sunscreen seems to have a protective role for the development of naevi that can be clearly demonstrated in the group of children aged 14 years.
Finally, we observed an increasing number of sunburns with age. As in the case of the use of sunscreen, these results could reflect the behaviour of adolescents, being less likely to apply sunscreen and being less controlled by their parents. In the bivariate study we obtained a significant correlation between having had sunburns and the number of naevi in the 14-year-old group (p < 0.05) and a tendency in the 4- and 8-year-old groups. However, we did not find significant association between sunburns and naevi counts in any of the 3 groups in the multivariate analysis. A possible explanation for these results could be the power of the study (low number of sunburns in the 3 age groups). Moreover, the lack of association between these 2 variables has also been documented in other studies (24).
In conclusion, a survey of naevi in 3 clear-cut paediatric age-groups enables maximum precision in measuring differences in the number of naevi. These results support a protective role of sunscreen against the development of acquired melanocytic naevi.
ACKNOWLEDGEMENTS
This study was partially supported by a grant from ISCIII and FEDER (PI1200260 to RMM). SM holds a predoctoral fellowship from IRBLleida/Diputació de Lleida. The authors sincerely acknowledge the contribution of the primary care paediatricians who enabled us to perform this study.

1http://www.medicaljournals.se/acta/content/?doi=10.2340/00015555-2277
REFERENCES
